INTRODUCTION
In December 2019, 27 index cases of a pneumonia of unknown etiology in Wuhan (Hubei, China) led to a pandemic caused by SARS-CoV-2 that shocked humanity. 1 COVID-19 infection, at first of a respiratory nature, progresses to a severe multisystem condition with an etiology consisting of strong inflammatory and immunological activation caused by the virus. 2 Epidemiological studies have early shown that patients with a higher risk of serious complications are elderly patients with underlying cardiovascular or pulmonary disease, or those with a higher cardiovascular risk as a result of blood hypertension (HTN), diabetes mellitus (DM), dyslipidemia, or obesity. 3 To reduce the impact of the pandemic, global social distancing and quarantine actions were taken with both direct and indirect consequences on people’s health. 4,5
Permanent isolation evidenced increased morbidity and mortality as a result of non- COVID-19 conditions. 6 Factors such as decreased physical activity, stress, and diet changes were typical during this period. 7-9 The pandemic and social isolation, in particular, increased the already high prevalence of obesity, an aspect that seems to be exacerbated in our region. 10,11 In addition, it is known that even mild increases in body mass index (BMI) may have a strong long-term impact on cardiovascular health. 12,13 All these aspects promote emergence or impair management of cardiovascular risk factors (CVRF), such as hypertension, dyslipidemia, and diabetes.
Measuring the impact of this period of time on the cardiometabolic profile will provide relevant information helpful to establish management strategies avoiding any long-term consequences. Therefore, the aim of this study was to assess the cardiometabolic profile of a population before and after COVID-19 lockdown. It was also to analyze the prevalence and characteristics of the population with increased weight and obesity in this period.
METHODS
An observational retrospective cohort design was used to compare the times before and after lockdown as a result of the COVID-19 pandemic. This study was conducted at Hospi tal Universitario René G. Favaloro, in the Autonomous City of Buenos Aires, Argentina. Fundación Favaloro has a Cardiovascular Health Prevention Program (Programa de Prevención de Salud Cardiovascular, PPS) aimed at monitoring general health, giving advice, educating on healthy lifestyle habits, and identifying patients with a high cardiovascular risk. In Argentina, the national government ordered the start of preventive and mandatory social isolation on March 19, 2020. Thereafter, medical services were restricted, and healthcare was readjusted to the requirements of the pandemic. The program began to become flexible and reopened after December 2020. All male and female individuals aged over 18 taking part in the program during 2019 (the time immediately preceding the pandemic) were included and took part again in 2021 (the time following the strict lockdown). The aim was to have individual information on each participant before and after lockdown. Patients with untreated hypothyroidism, a history of acute or chronic hepatic and/ or renal disease, pregnant or breastfeeding women, and patients with malignancies or diseases with less than one year life expectancy were excluded. For HTN and type 2 DM, the incidence of new cases was compared to a similar period of time in patients attending the program between 2017 and 2019.
Data were collected from medical records, including anthropometric parameters, medical history, and laboratory results. Only data derived from clinic visits on the days scheduled for the program were considered.
Night fasting venous blood samples were collected from each subject. Fasting glycemia (GLY), total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), and glycosylated hemoglobin (HbA1c) were measured using colorimetric methods with a semi-automatic biochemistry analyzer (Architect 8000/4000, Abbott Diagnos tics, USA). Low-density lipoprotein cholesterol (LDL-C) was estimated using the Friedewald’s formula.
The waist circumference (WC) was measured using a non-expanding metric tape on a midpoint between the lower edge of ribs and the iliac crests with the patient standing in normal exhalation. The BMI, weight/height2, was estimated, and obesity was diagnosed with an BMI of ≥30 kg/m2. The characteristics of the group of patients with a higher than 5% increase in their body weight (W+5%) were explored and compared to the rest of the population (W-5%). DM was diagnosed when the patient had a history of fasting glycemia ≥126 mg/dL in at least 2 measurements, or was administered insulin or oral hypoglycemic drugs. 14 HTN was considered with a repeated systolic blood pressure (SBP) ≥140 mmHg and/or diastolic blood pressure (DBP) ≥90 mmHg, or use of antihypertensive drugs. 15 Smoking (SMK) was considered with a history of >100 cigarettes in a lifetime and ex-smoker (ex-SMK) with no cigarette use in the last six months. 16 Metabolic syndrome (MS) was diagnosed based on National Cholesterol Education Program - Adult Treatment Panel III (NCEP-ATP III) criteria. 17
Subclinical carotid atheromatosis, as a dichotomic vari ant, was evaluated through an ultrasound using an Affinity 50 ultrasound system (Philips HealthCare, USA) and a vas cular 9-12 Mhz probe. Images were defined as a focal protru sion towards arterial lumen with a thickness over 0.5 mm, or an increase over 50% in the adjacent intima-media thickness (IMT), or a diffuse >1.5-mm increase in the IMT measured between the media-adventitia and intima-lumen. 18.19
This study was approved by the institutional ethics commit tee.
Statistical analysis
Quantitative variables are described as the mean ± standard deviation, or median and interquartile range, based on distribution. Comparisons before and after the pandemic were made using the Student’s t-test for paired data, or Wil coxon test for paired data, as appropriate. Categorical variables were described as the total number and percentage and compared with the Chi-square test or the Fisher’s exact test, or McNemar test in case of paired proportions. The odds ratio was estimated with its corresponding 95% confidence interval when comparing the incidence of DM and HTN be tween 2017-2019 and 2019-2021. To evaluate the correlation between increased weight and age, the Pearson correlation test, expressed with the correlation coefficient r and its sta tistical significance, was used. All tests were 2-tailed, and a <0.05 p-value was considered to be statistically significant.
RESULTS
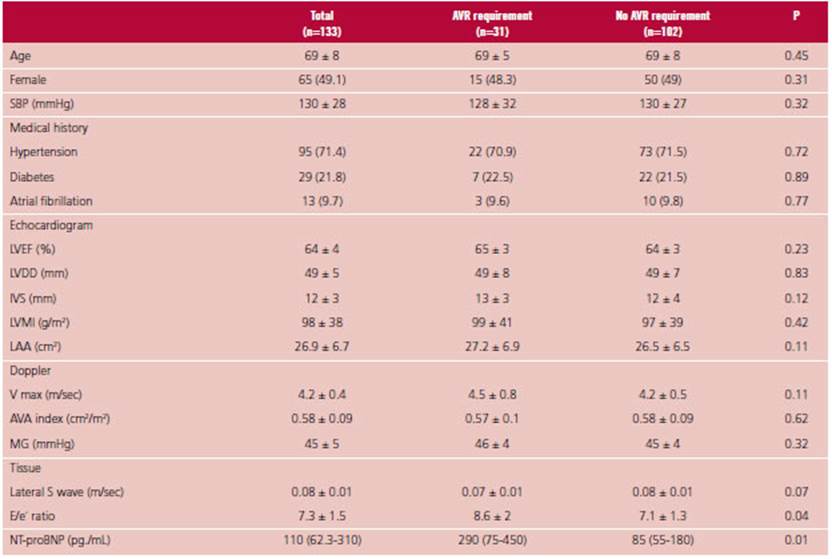
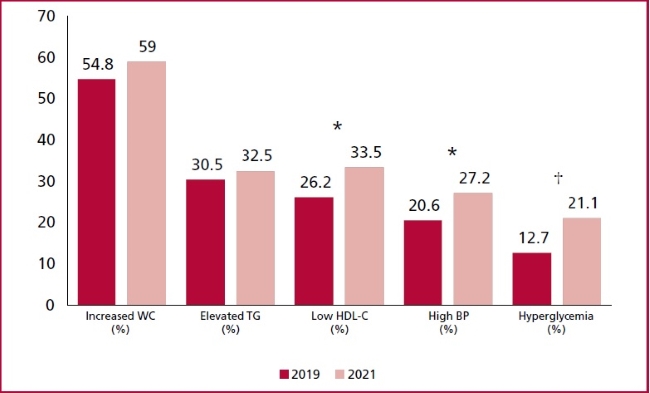
There were 5423 patients in the PPS in 2019, and 3423 patients in 2021. Patients who were part of the program both in 2019 and 2021 were 558. In 2019, the average age was 52.2 ± 12.8 years, and 41.2% were women. An average of 1.8 ± 0.5 years elapsed between both evaluations. Table 1 shows baseline demographics and compares data in 2019 to data in 2021. A mild but significant 1.2% increase was observed in body weight (p<0.0001), similar for the BMI (1.4% increase; p<0.0001). No changes were observed in the percentage of patients with obesity. There was an absolute 3% increase in HTN diagnosis during the pandemic, together with increased mean SBP and DBP levels. As for glycemia, 3% new cases of DM were diagnosed. The median glycemia increased 4 mg/dL in the 2-year follow-up (p<0.0001). In the overall population, the frequency of SMK and ex-SMK was similar between visits, with 4.5% (n=25) new smokers in 2021, and 3% (n=17) patients who had quitted smoking upon the evaluation that year. The lipid profile was affected, with an HDL-C decrease (51.8 ± 12.7 vs. 49.3 ± 12.8 mg/dL; p<0.0001), and no changes in other aspects under analysis. MS diagnosis significantly increased in the population (21.5% vs. 34.1%; p<0.0001) (Figure 1). The average criteria in the MS increased from 1.5 ± 1.2 to 2 ± 1.3 (p<0.0001).
New HTN and DM diagnoses in 2017-2019 and in 2019-2021 were evaluated. There were 7884 partici pants in the PPS in 2017, of whom 2111 repeated the test in 2019. Of these, 165 had DM and 629 were hy pertensive patients at the beginning of the period. In 2017-2019, 23 new cases of DM and 26 new cases of HTN were identified. The incidence of new cases was higher in 2019-2021, with 17 newly diagnosed cases of DM (OR 3.5, 95% CI 1.8-6.7; p<0.001) and 16 of HTN (OR 2.4, 95% CI 1.3-4.6; p<0.005).
In the W+5% group (n=105), no differences were observed in the baseline weight in 2019 (W+5% 81.8 ± 20.3 kg vs. W-5% 82.1 ± 17.1 kg; p=NS) or the BMI (W+5% 29.3 ± 5.2 vs. W-5% 29.6 ± 6.3 kg/m2; p=NS). However, this population was represented by younger patients (W+5% 47.6 ± 14 years vs W-5% 53.3 ± 12 years; p<0.0001), and a significant reverse correlation was observed between age and scope of weight increase (r=-0.1; p<0.02). In addition, it was observed that W+5% patients were less likely to have HTN (22.8% vs 33.6%; p<0.05). No differences were observed in this group as for DM (W+5% 7.6% vs W-5% 9%; p=NS), SMK (W+5% 20.9% vs W-5% 15.9%; p=NS), ex-SMK (W+5% 27.6% vs W-5% 29.6%; p=NS), fre quency for females (W+5% 48.6% vs W-5% 39.5%; p=NS), or a history of cardiovascular disease (W+5% 1.9% vs W-5% 4.2%; p=NS).
The analysis of adherence to treatment showed that, out of 39 patients using metformin in 2019, 3 (7.7%) discontinued this drug. However, out of 13 patients using another antidiabetic treatment, 23.1% (3 patients) discontinued their medication. Of the total number of patients with HTN in 2019, 96% (169 pa tients) received drug therapy. In 2021, 19.9% of patients with HTN had discontinued their medication, 12.5% (22 patients) reduced the number of drugs, and 11.4% (20 patients) increased the number of drugs used. The most common hypolipidemic agent in 2019 were statins (116 patients, 20.8%), followed by ezetimibe (9 patients, 1.6%) and fibrates (8 patients, 1.4%). By 2021, the use of statins among participants was 24.7% (138 patients), fibrates 2.3% (13 patients), and ezetimibe 2% (11 patients), with no significant differences as compared to 2019. Of the total number of patients receiving statins in 2019, 14.6% (17 patients) discontinued treatment. During the study period, 7% of the population (39 patients) began to use statins.
The evaluation of carotid atheromatosis showed a non-significant increase between 2019 and 2021 (36.4% vs 40.7%; p=NS). In the period under analysis, patients had 3 acute myocardial infarctions, 2 coronary angioplasties, and 1 coronary artery bypass grafting.
DISCUSSION
The COVID-19 pandemic has shocked the world. The World Health Organization (WHO) defines a disaster as a series of events that disrupt daily life in a community or society causing material, economic or environmental damage. 20 The COVID-19 pandemic is a biological disaster which is still unsolved and with consequences for many years to come. 21 This paper could identify an increased prevalence of risk factors in the period before and after the pandemic, reflected by a higher prevalence of hypertension, dyslipidemia (characterized by lower HDL-C), high BMI, hyperglycemia, and type 2 DM. This was associated to an increased prevalence of MS, particularly as a result of more frequent hyperglycemia, low HDL-C, and elevated blood pressure. Various studies have assessed the incidence of new cases of DM, HTN, and dyslipidemia, with inconsistent results. Particular ly glycemia worsened in patients with DM, with no changes in glycosylated hemoglobin according to a recent meta-analysis. 22 Burekovic et al. have shown more new cases of DM in a period similar to the one under analysis. 23 These authors also suggest that acute COVID-19 infection might favor hyperglycemia and a subsequent DM diagnosis. During the pandemic and lockdown, increased HTN has also been observed; the direct impact of the infection and interaction with the renin-angiotensin-aldosterone system as the root cause cannot be ruled out. 24 The incidence observed in new cases of DM and HTN was significantly higher in 2019-2021, as compared to 2017-2019; this result suggests an increase due to the pandemic and lockdown. Further studies should elucidate whether the impaired cardiometabolic profile results from adverse lifestyle changes or the direct influence of COVID-19 infection.
Observations regarding the BMI and obesity should be considered separately. Several reports have shown increased obesity and overweight relative to lockdown. 10,11 This may be because physical and social isolation are well-known risk factors for obesity. 25 A lower-quality diet has also contributed. The combination of lack of physical activity, staying at home, increased intake of snacks and high-calorie meals lead to rapid weight gain. 26 Overeating is particularly increased when there are emergency food stocks available. 27 It is important to note that about 1 in 5 patients increased weight by more than 5%. In this respect, Mozaffarian et al. showed that moderate weight gain has an adverse effect on metabolism, increases the risk of diabetes and the incidence of cardiovascular events. 12 Therefore, preventing the weight gain frequently observed in the pandemic may be one major way to avoid long-term consequences. In our study, weight gain was associated to a younger age. Simone et al. showed that 70% of individuals from a young population admitted that the events related to the COVID-19 pandemic affected their eating habits. 28 This group mentioned lack of concern about food, higher food intake, or eating “to bear the situation,” among other characteristics of their eating habits during the pandemic. Variables relative to these findings were anxiety/depression, stress management, financial difficulties, and sudden changes of schedule. These factors, associated with a lower concern for the future consequences of weight changes, might partly explain this.
Adherence to treatment was one major health problem during the pandemic, mainly due to impaired access to drugs. 29 In a study evaluating difficulties in access to drugs for 1103 patients with chronic diseases, 51% of patients found it hard to find their medication during the pandemic and lockdown, and the most reported cause was doctor’s unavailability. 30 Many of these conditions were likely to be temporary in the first stage of the period. In our population, the patients most prone to discontinue medication were those who received antihypertensive agents and those with diabetes under treatment with a combination of drugs. There was no lack of adherence to hypolipidemic agents.
Note that our study had some limitations. The population consists in PPS participants, rather than the general population. Even so, the frequency of CVRF is similar to the one reported in the 4th National Survey on Risk Factors. 31 The retrospective design makes it impossible for us to know what happened between both periods of time under analysis. This is important, as many of the variables being assessed may have been temporarily altered (e.g., changes in bodyweight or medication availability) throughout the pandemic.
In conclusion, our study shows increased exposure to CVRF during the pandemic and social isolation because of COVID-19. This aggravates the adverse landscape of exposure to such factors, already present before the pandemic. We need to identify the changes above, particularly those relative to an increased BMI in young individuals, to seek a healthy lifestyle for our patients. The prospective implications of these findings might become apparent in the next few years if these metabolic changes are not reversed. Future studies need to prospectively monitor the progress of these findings.