Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista argentina de cardiología
On-line version ISSN 1850-3748
Rev. argent. cardiol. vol.92 no.1 Ciudad Autónoma de Buenos Aires Mar. 2024 Epub Feb 28, 2024
http://dx.doi.org/10.7775/rac.es.v92.i1.20732
SCIENTIFIC LETTER
Coronary Angiography and Stress Myocardial Computed Tomography Perfusion: a Clinical Reality
1 Cardiothoracic Imaging Section. Radiology Service. Clínica Universidad de Navarra.
The reference standard for diagnosing coronary artery disease is conventional coronary angiography. This is an invasive and not free of complications technique, which is still performed for purely diagnostic purposes in a large number of patients who do not really require it. 1 This has led to the search for diagnostic alternatives that help in clinical management and that allow better selection of subjects requiring this procedure.
We present the case of a 70-year-old patient with hypercholesterolemia as the only cardiovascular risk factor without medical treatment, who had an active life, varied diet and occasional alcohol consumption. His brother had died of a heart attack at 55 years of age and his sister was diabetic.
He came to the clinic for cardiological evaluation due to episodes of chest tightness for the past 3 months. The tightness appeared during exertion, when walking quickly or climbing a hill, and subsided with rest. In the last week symptoms had been more serious, with greater chest tightness and dyspnea when walking.
Physical examination revealed a blood pressure of 150/85 mmHg. Cardiac and pulmonary auscultation was normal with no signs of heart failure. The ECG showed sinus rhythm of 67 beats per minute, horizontal axis, normal PR interval and narrow QRS complex. Lab test showed total cholesterol of 234 mg/dL, with an LDL cholesterol of 166 mg/dL. The chest x-ray was normal.
A coronary computed tomography angiography (CCTA) was requested to study the symptoms reported by the patient (Figure 1). The right and circumflex coronary arteries were diffusely ill, with calcified and non-calcified plaques that caused < 50% stenosis. A large calcified and non-calcified plaque of about 23 mm length was observed located in the mid left anterior descending coronary artery, at the ostium of the diagonal branches, that caused lumen stenosis of 70-99%. Given these findings, it was decided to complete the exploration using stress CT-perfusion with a vasodilator drug (regadenoson) (Figure 2). The test was positive for myocardial ischemia in the territory corresponding to the left anterior descending coronary artery. The study was classified as CAD-RADS 4A/P3/I+ (corresponding to severe stenosis with a large size plaque and demonstration of ischemia). With this result, the patient was referred to the Hemodynamics service, where a catheterization, that confirmed the serious lesions described in the CCTA (Figure 2), was performed. The first stenosis was treated with stent implantation. The most distal lesion could not be treated percutaneously because the vessel was sub-occluded. Finally, it was treated by aortocoronary bypass surgery with a graft from the left internal mammary artery to the mid left anterior descending coronary artery and from the saphenous vein to the diagonal branch.
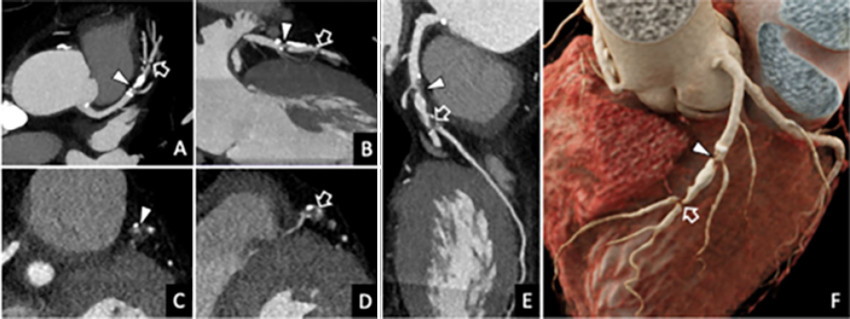
Figure 1 Coronary CT angiography. A, B: Multiplanar reconstructions of the left anterior descending coronary artery. C, D: Reconstructions perpendicular to the long axis of the vessel. E. Curved planar reconstruction. F. Kinematic volumetric reconstruction. The study demonstrated 70-99% stenosis in the mid third of the left anterior descending coronary artery, which involves its origin (arrowhead) and second diagonal branch (hollow arrow).
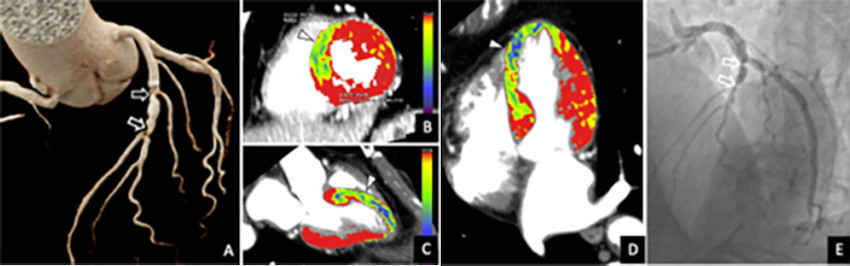
Figure 2 Coronary CT angiography, stress CT-perfusion study and conventional coronary angiography. A. Kinematic reconstruction of the coronary tree. B, C, D. Short axis (B), three-chamber (C), and four-chamber (D) stress CT-perfusion reconstructions. E. Conventional coronary angiography. CCTA demonstrated two points of 70-99% stenosis in the mid third of the left anterior descending artery (hollow arrows in A). The study was completed with stress CT-perfusion to assess its functional significance, demonstrating inducible ischemia in septal segments (arrowheads). Based on these findings, the test was classified as CAD-RADS 4A/P3/I+. Conventional coronary angiography confirmed the CCTA findings (hollow arrows in E).
CCTA has become the reference standard to evaluate the coronary tree in a non-invasive, reliable and accurate way. Specifically, given its ability to rule out coronary artery disease, this technique plays a very important role in the management of patients with chest pain, as demonstrated in the SCOT-HEART (Scottish Computed Tomography of the Heart), PROMISE (Prospective Multicenter Imaging Study for Evaluation of Chest Pain) and DISCHARGE (Diagnostic Imaging Strategies for Patients with Stable Chest Pain and Intermediate Risk of Coronary Artery Disease) studies. Thus, the most current international guidelines and recommendations consider CCTA as the imaging technique of choice for the clinical management of patients with chest pain, especially when they have a low or intermediate pretest probability of suffering from coronary heart disease. 2,3 The great limitation of the technique is its relative low specificity, for example, in patients with extensive coronary calcification or stent. In these cases, it is not uncommon to have to resort to functional techniques to complete the study and demonstrate the presence of ischemia: stress echocardiogram, stress magnetic resonance imaging, single photon emission computed tomography (SPECT) and positron emission tomography (PET).
Therefore, the most recent advances in CT have allowed for this technique, in addition to providing detailed information of the arterial coronary system, to understand the functional meaning of a coronary stenosis, either by applying artificial intelligence algorithms and principles of computational fluid dynamics to CCTA images (known as FFR-CT) or by performing a myocardial perfusion study using the CT equipment itself (CT-perfusion) under stress induced by a vasodilator drug.
In general, compared with the rest of the ischemia detection tests, CT-perfusion provides anatomical and functional information integrated in a single examination. The acquisition is fast, has submillimeter spatial resolution and allows perfusion to be quantified with precision given the linear relationship between the amount of iodinated contrast and the attenuation of the myocardial tissue. The limitations of perfusion- CT include the use of ionizing radiation, possible artifacts, both due to movement as hardening of the X-ray beam, and the need to use specific software to interpret the study.
In the present clinical case, the incremental diagnostic value of CT-perfusion compared with CCTA is demonstrated and it can be seen that adding CT-perfusion to CCTA allows increasing the specificity of the test. In this sense, there are several works that advocate completing CCTA with a CT-perfusion study. For example, the CRESCENT-II (Comprehensive Cardiac CT Versus Exercise Testing in Suspected Coronary Artery Disease 2) study concludes that, in patients with stable chest pain, the combination of CCTA and CT-perfusion in subjects with ≥50% stenosis is an effective alternative to conventional traditional methods of detecting ischemia, with which a significantly higher proportion of catheterizations with an indication for coronary revascularization (88% vs. 50%; p= 0.017) 4 is achieved.
The results of the work carried out on CT-perfusion are incorporated into the most recent cardiac CT guidelines, which indicate that it may be appropriate to perform CT-perfusion to evaluate the functional importance of intermediate stenosis detected on CCTA (stenosis of 30-90% diameter), particularly in the context of multivessel disease, to help select patients who require conventional coronary angiography, and to plan revascularization treatment. 5 Additionally, the updated recommendations of the standardized CCTA report (Coronary Artery Disease Reporting and Data System, CAD-RADS 2.0) includes CT-perfusion assessment of ischemia as a new modifier (modifier I of ischemia), pointing out that this technique allows the exclusion of myocardial ischemia in moderate coronary stenosis (50 to 69%) or in suspected severe coronary stenosis (≥70%) with dense calcified or mixed plaques, avoiding additional later tests. 6
In conclusion, CCTA allows us to exclude coronary heart disease with great reliability, but has low diagnostic specificity. Taking into account that the clinical benefit of revascularization is limited to lesions causing ischemia and not only to quantify the degree of coronary stenosis, CT-perfusion plays an important role and has great added value in patients with proven coronary stenosis demonstrated by CCTA, not only from a diagnostic point of view (by increasing the precision and predictive value of the test) but also in risk stratification, prognostic assessment and for therapeutic decisions.
REFERENCES
1. Patel MR, Peterson ED, Dai D, Brennan JM, Redberg RF, Anderson HV, et al. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010;362:886-95. https://doi.org/10.1056/NEJMoa0907272 [ Links ]
2. Writing Committee Members; Gulati M, Levy PD, Mukherjee D, Amsterdam E, Bhatt DL, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/ SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021;78:e187-e285. https://doi.org/10.1016/j.jacc.2021.07.053 [ Links ]
3. Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck- Brentano C, et al. ESC Scientific Document Group. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41:407-77. https://doi.org/10.1093/eurheartj/ehz425 [ Links ]
4. Lubbers M, Coenen A, Kofflard M, Bruning T, Kietselaer B, Galema T, et al. Comprehensive Cardiac CT With Myocardial Perfusion Imaging Versus Functional Testing in Suspected Coronary Artery Disease: The Multicenter, Randomized CRESCENT-II Trial. JACC Cardiovasc Imaging. 2018;11:1625-36. https://doi.org/10.1016/j.jcmg.2017.10.010 [ Links ]
5. Narula J, Chandrashekhar Y, Ahmadi A, Abbara S, Berman DS, Blankstein R, et al. SCCT 2021 Expert Consensus Document on Coronary Computed Tomographic Angiography: A Report of the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr. 2021;15:192-217. https://doi.org/10.1016/j.jcct.2020.11.001 [ Links ]
6. Cury RC, Leipsic J, Abbara S, Achenbach S, Berman D, Bittencourt M, et al. CAD-RADS(tm) 2.0 - 2022 Coronary Artery Disease-Reporting and Data System: An Expert Consensus Document of the Society of Cardiovascular Computed Tomography (SCCT), the American College of Cardiology (ACC), the American College of Radiology (ACR), and the North America Society of Cardiovascular Imaging (NASCI). J Cardiovasc Comput Tomogr. 2022;16:536-57. https://doi.org/10.1016/j.jcct.2022.07.002 [ Links ]











 text in
text in 



