Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista argentina de cardiología
On-line version ISSN 1850-3748
Rev. argent. cardiol. vol.92 no.1 Ciudad Autónoma de Buenos Aires Mar. 2024 Epub Feb 28, 2024
http://dx.doi.org/10.7775/rac.es.v92.i1.20734
SCIENTIFIC LETTER
Non-Contrast Electron Density Detection of Pulmonary Thromboembolism and Myocardial Infarction
1Department of Cardiovascular Imaging, Instituto Medico ENERI, Clínica La Sagrada Familia, Buenos Aires, Argentina
2 Department of Cardiology , Instituto Medico ENERI, Clínica La Sagrada Familia, Buenos Aires, Argentina
3 Department of Radiology , Instituto Medico ENERI, Clínica La Sagrada Familia, Buenos Aires, Argentina
4 Stroke Unit , Instituto Medico ENERI, Clínica La Sagrada Familia, Buenos Aires, Argentina
Most research involving spectral computed tomography (CT) has been related to its ability to improve tissue characterization in contrast-enhanced acquisitions, while preliminary investigations have suggested its usefulness for tissue characterization in non-enhanced examinations. 1,2
Dual-layer spectral CT enables the direct estimation of tissue electron density (ED) on a voxel (volumetric pixel, the minimum processable unit of a three-dimensional matrix, the equivalent of the pixel in a 2D object) basis, without modifications of acquisition protocols. 3 Previous studies have suggested improved tissue characterization using ED imaging. 4
We report the case of a patient admitted with an acute ischemic stroke, in whom a cardiac CT requested to rule out a cardiac embolic source, identified the presence of pulmonary thromboembolism and myocardial infarction, both findings being identifiable using the non-contrast coronary artery calcium scan.
A 66-year-old man with hypertension and type 2 diabetes as coronary risk factors, and a history of coronary artery bypass grafting (left internal mammary artery to left anterior descending artery) 17 years ago, presented to the clinic with right hemianopsia, 30 hours after symptoms onset (NIHSS 2). His blood pressure was normal (129/85 mmHg) and his pulse was regular (77 bpm). A brain magnetic resonance was performed demonstrating a temporooccipital acute ischemic lesion, with occlusion of the P2 segment of the posterior cerebral artery, outside the therapeutic window for acute treatment.
Five days before he had been admitted to another institution due to a non-ST elevation myocardial infarction, and after percutaneous coronary revascularization with stent deployment in the left circumflex artery, he was discharged with no complications.
On admission, his daily treatment included aspirin 100 mg, clopidogrel 75 mg, bisoprolol 2.5 mg, dapaglifozin 10 mg, and rosuvastatin 20 mg.
The ECG showed sinus rhytm, with negative T waves in DIII and AvF leads. The first cardiac troponin value was 500 ng/mL, descending thereafter.
A transthoracic echocardiogram was performed, reporting a preserved global left vetricular function (left ventricular ejection fraction 58%) with inferior and inferolateral hypokinesis. A cardiac CT (IQon Spectral CT scanner, Philips Healthcare, The Netherlands) was requested to rule out an embolic source (Figure 1). Contrast-enhaced images identified the presence of pulmonary thromboembolism (Figure 1, panel a, arrow), and a severe perfusion defect of the basal inferior left ventricular wall (Figure 1, panel b, arrows). A patent stent was detected in the left circumflex artery, whereas a severe irregular lesion was identified at the distal (large and dominant) right coronary artery (Figure 2). Of note, using ED imaging, the pre-contrast coronary artery calcium scan (32 x 0.625 mm collimation, 2.5 mm thickess, 120 kV, 80 mAs, rotation speed 0.33 seconds, triggered at 75% of the RR interval), enabled the detection of both the pulmonary thromboembolism (Figure 1, panel c, arrow) and the inferior basal myocardial infarct (Figure 1, panel d, arrows). The ED value measured at the high-density area corresponding to the pulmonary thrombus was 107.9 %EDW (mean percentage ED relative to water), compared with values of 104.3%EDW at the main pulmonary artery and of 103.9 %EDW at the ascending aorta. The ED value measured at the low-density area corresponding to the myocardial infarct was 101.9 %EDW, compared with values of 104%EDW at the remote myocardium.
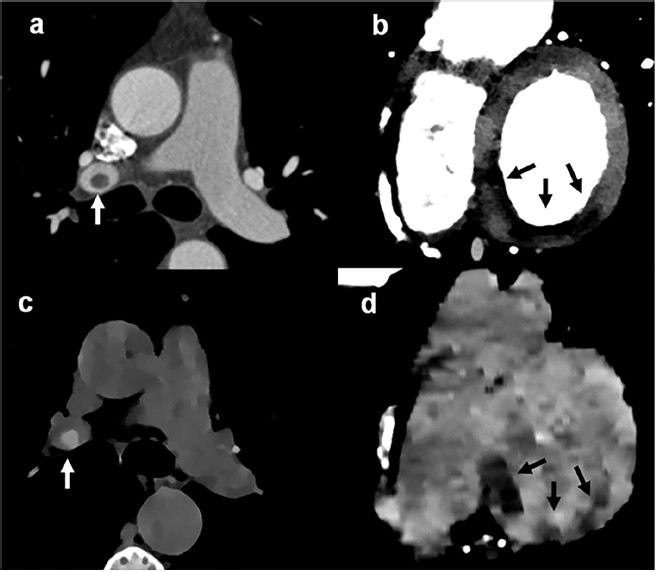
Fig 1 Contrast-enhanced cardiac computed tomography (panels a and b) showing a pulmonary thromboembolism (panel a, arrow) and a myocardial perfusion defect of the inferior wall (panel b, arrows). Non-contrast electron density images derived from coronary calcium scoring scan (panels c and d) showing the same findings without contrast administration. Thrombus displayed as white, related to high electron density values (panel c), whereas the perfusion defect is displayed as an area with low electron density values (panel d).
Cardiac magnetic resonance confirmed the findings (Figure 2), showing transmural myocardial edema using T2-weighted imaging, and a predominantly subendocardial inferior myocardial infarction.
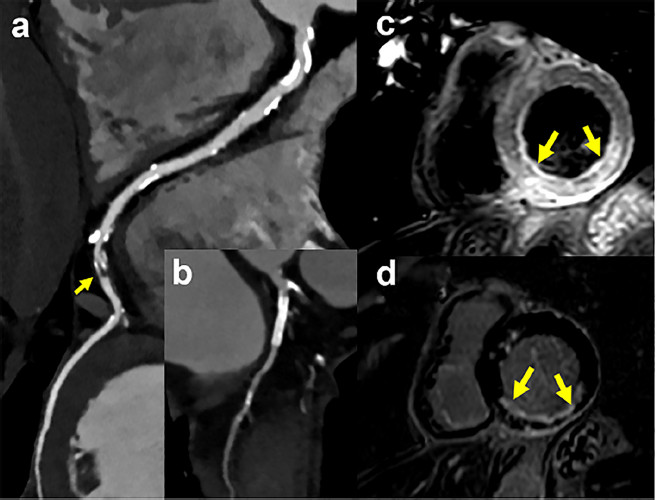
Fig 2 Coronary CT angiogram, showing a large and dominant right coronary artery with a severe distal lesion (panel a, arrow), and a patent stent in a small left circumflex artery (panel b). Cardiac magnetic resonance (panels c and d) images displayed in basal short axis views, demonstrating an inferior- wall myocardial infarction (panel c: T2-weighted imaging, panel d: late enhacement).
The case was interpreted as an ischemic stroke in the context of an acute myocardial infarction. Given the presence of pulmonary thromboembolism, he received enoxaparin 60 bid for seven days, and oral apixaban 5 mg bid thereafter. The patient evolved stable and was discharged.
The assessment of acute myocardial infarction and pulmonary thromboembolism requires contrastenhanced examinations. Although dual energy CT improves tissue characterization, with an incremental value among diverse clinical settings, particularly involving cardiothoracic imaging, most research about dual energy CT involves the ability of iodine density maps and low monoenergetic imaging to enhance tissue discrimination. On the contrary, the potential usefulness of spectral imaging for non contrast examinations remains widely unexplored, especially the role of ED imaging.
Coronary artery calcium scoring (CAC) has been extensively validated for atherosclerotic cardiovascular disease risk assessment among asymptomatic patients. Nonetheless, the role of CAC testing as a gatekeeper within the Emergency Department remains uncertain if not discouraged. In this regard, a recent large registry including patients presenting to the emergency department with acute chest pain at low to intermediate risk for acute coronary syndrome, who underwent CAC and coronary CT angiography, identified a 99% negative predictive value of CAC for ruling out obstructive coronary artery disease and revascularization.
To the best of our knowledge, this is the first case to report that CAC might potentially be able to detect, aside from the presence and extent of coronary artery calcifications, pulmonary artery thromboembolism and early tissular changes associated with myocardial infarction. CAC is an unsophisticated, non-contrast, fast, and safe (associated with low radiation dose) tool. While performed in a dual-layer configuration CT scanner, CAC allows the simultaneous acquisition of spectral data such as ED imaging without affecting routine workflow. 4 In this regard, in a previous study ED imaging had the lowest deviation from phantom tissue-equivalent inserts compared to other spectral parameters. 5 Our findings are in line with those from a recent preliminary report including non-gated chest CT examinations, showing the potential of ED imaging to improve the detection of low contrast structures, in part due to the almost absence of noise in ED images. 6 The clear identification of pulmonary thromboembolism using unenhanced scans shown in our case might warrant further research in the field of pulmonary and cardiac embolic detection. Indeed, pulmonary embolism is one of the major complications of stroke, with high rates of death. Furthermore, the possible identification of myocardial infarction without the requirement of contrast administration might provide added value among non-enhanced examinations, wich is conceivably relevant for patients with impaired renal function or for those at risk for contrast- induced nephropathy.
In conclusion, we present the first report showing the potential of CAC perfomed in a dual layer spectral CT scanner to identify, aside from the presence and extent of coronary artery calcifications, pulmonary artery thromboembolism and signs of myocardial infarction.
REFERENCES
1. Chakrabarti R, Gupta V, Vyas S, Gupta K, Singh V. Correlation of dual energy computed tomography electron density measurements with cerebral glioma grade. Neuroradiol J 2022;35:352-62. https://doi.org/10.1177/19714009211047455 [ Links ]
2. Shim E, Kim BH, Kang WY, Hong SJ, Kang CH, Ahn KS, et al. Diagnostic performance of electron-density dual-energy CT in detection of cervical disc herniation in comparison with standard gray-scale CT and virtual non-calcium images. Eur Radiol 2022;32:2209-20. https://doi.org/10.1007/s00330-021-08374-y [ Links ]
3. Mei K, Ehn S, Oechsner M, Kopp FK, Pfeiffer D, Fingerle AA, et al. Dual-layer spectral computed tomography: measuring relative electron density. Eur Radiol Experiment 2018;2:20. https://doi.org/10.1186/s41747-018-0051-8 [ Links ]
4. Abdullayev N, Große Hokamp N, Lennartz S, Holz JA, Romman Z, Pahn G, et al. Improvements of diagnostic accuracy and visualization of vertebral metastasis using multi-level virtual noncalcium reconstructions from dual-layer spectral detector computed tomography. Eur Radiol 2019;29:5941-49. https://doi.org/10.1007/s00330-019-06233-5 [ Links ]
5. Hua CH, Shapira N, Merchant TE, Klahr P, Yagil Y. Accuracy of electron density, effective atomic number, and iodine concentration determination with a dual-layer dual-energy computed tomography system. Med Phys 2018;45:2486-97. https://doi.org/10.1002/mp.12903 [ Links ]
6. Rodriguez-Granillo GA, Cirio J, Vila JF, Langzam E, Ivanc T, Fontana L, et al. Noncontrast Myocardial Characterization in Acute Myocardial Infarction Using Electron Density Imaging. J Thorac Imaging. 2023. Epub ahead of print. https://doi.org/10.1097/RTI.0000000000000749 [ Links ]











 text in
text in 



