INTRODUCTION
Chronic lower limb ulcers (CLLU) remain a challenging problem in modern society, and represent significant medical, economic and social burdens[1,2].The epidemiological rates vary considerably depending on diagnosis, year and country[3]. Chronic ulcers will continue to be a growingconcern as increases life expectancy and more people will be at risk for developing these conditions[4]given the increasing prevalence of diabetes and other chronic diseases that may affect wound healing[5].
Successful treatment that stimulates healing is an essential step toward eliminating morbidity, improving quality of life for patients, and decreasing healthcare costs[6]. Surgical treatment accounts for the major portion of treatment activity[7].The standard of care for chronic ulcers are debridement[8], infection control, moisture balance[9],[10]and wound cleansing, with pressure offloading for diabetic foot ulcers (DFU)[8] and pressure ulcers (PU)[4]and compression therapy for venous ulcers (VU)[9].The combination of the high prevalence of chronic ulcers with the resource intensity of treatment, results in a high economic burden to the health-care system[4].
Data on treatment cost for CLLU are inconsistent andvary largely depending on disease, health system and evaluation method[11].More precisely, in developed countries reported annual costs per patient for VU range from US$4000 to US$35000[11]. Pressure ulcers have been observed to result in US$700 to US$90000 excess hospital cost and DFU has ranged from US$11710 to US$21400in the first year[12]. Limited evidence is available on the costs of CLLUin LatinAmerican countries.One study in Brazil with DFU showed an estimated average cost for outpatient management that range fromUS$400 to US$1600[13] and the average hospitalization cost per patient range from US$400 to US$2700[13].Meanwhile, in Peru the annual cost perpatient hospitalizationrangefrom US$1022 to US$7360 according to the treatment applied[14].Major cost drivers were hospitalization, nursing costs and dressing material for health system[15] and topical drugs and medical products for patients[15]. In Argentina, there is a lack of information about epidemiological and economic impact of CLLU.Burden information is important for public health policy makers to advocate for implementation of prevention, treatment recommendations[13] and therapeutic effectiveness. Therefore, this study was undertaken to analyze the demographic and hospital economic characteristics of chronic lower limb ulcers in a public hospital in Argentina.
METHODS
II.A. Study population and data assessment
A retrospective study of outpatients and inpatients treated at Angel C. Padilla Hospital during the period from January 1, 2013 to December 31, 2014 was performed.This is a referral hospital in Province of Tucuman and the northwest of Argentina.The examined population comprised all hospital consultations and admissions, based on the International Classification of Diseases (ICD-10): L97 (Ulcer of lower limb, not elsewhere classified), E11.5 (Type 2 diabetes mellitus with peripheral circulatory complications), I83.0 (Varicose veins of lower extremities with ulcer), I77.8 (Other specified disorders of arteries and arterioles) and L89 (Decubitus ulcer and pressure area).
Demographic information (age and gender) were collected from the patients’ medical records over the study period. To estimate the cost of hospitalization the length of stay for inpatient and the number of consultations for outpatient were obtained. There were also identified treatments performed to the ulcer and to the control of infection, surgical procedures and laboratory tests.
II.B. Calculation of cost
The associated costs were calculated using the Nomenclator of Health Benefits for the Public Hospitals (NHM National Health Ministry Resolution No. 60-2015) and converted to 2014 US dollars. The estimated cost of CLLU inpatients includes total hospitalization days (medical and nursing fees, drug treatment, disposables and practice fees), laboratory tests and surgical procedures (amputation, surgical debridement, skin biopsies, bone biopsies, vascular surgery and skin graft). Outpatient costs include the total number of consultations, nursing fees and disposables for cleansing the ulcerand laboratory tests.
II.C. Statistical analysis
Data have been summarized and reported as percentage and frequency tables. All analyses were performed using SPSS (Statistical Package for Social Science) software (version 22.0) (SPSS Inc., Chicago, IL).
II.D. Ethical standards
This study was conducted with the approval of the Ethics and Teaching Committee from the Angel C. Padilla Hospital.
RESULTS
III.A. Consultations and outpatients characteristic
The overall number of consultation with ICD-10 codes showing in Table 1 in the period of study was 7224, corresponding to 640 patients. The highest ratio of consultation occurred between 50 and 59 years old (55.46%)with almost 97% of consultation recorded as L97.The mean age (±SD) for male outpatient consultations was 59.53(±13.06) years and 59.04(±10.93) years for female outpatient consultations. The oldest patient was 88 years and the youngest was 16 years. A slight male predominance was observed in consultations (53.16%).
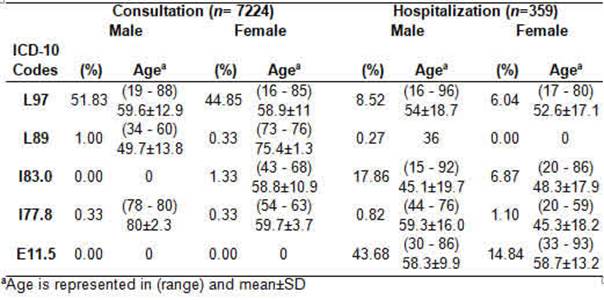
Table 1:“Age and gender distribution according to ICD-10 codification for consultation and hospitalization”.
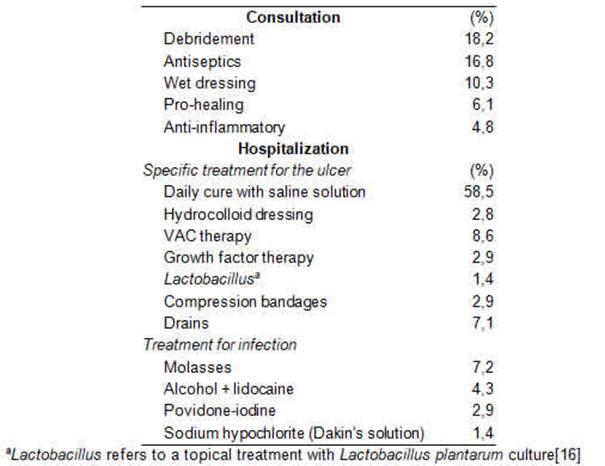
Twice a week outpatients assisted to the hospital to have wound cleansing with saline solution. A total of 65016 cleansings were registered in this study. Other treatments showing in Table 2 were performed on outpatients with CLLU. Topical medication was applied in 48.6% of the treatments. The most common were autolytic debridement products (chloramphenicol-collagenase ointment), antiseptics (molasses, silver sulfadiazine cream, Dakin’s solution, ethanol, acetic acid and povidone iodine), moist occlusive dressing (soft dressing and transdermal patches) and pro-healing (skin graft, platelet-rich plasma and Centellaasiatica). Two clinical laboratory tests(complete blood count, erythrocyte sedimentation rate, blood glucose test, blood urea nitrogen, creatinine blood test and urinalysis) were requested per year to each outpatient. A number of 1204 clinical laboratory tests and 602 bacterial identifications by culturing from biopsies samples(antibiotic sensitivity and Gram stain) were performed.
III.B. Hospital admissions and inpatients characteristics
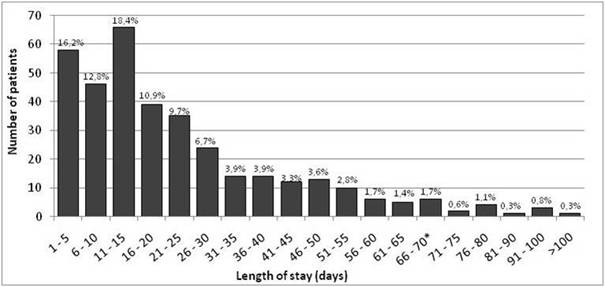
During the 2-years study period, 359inpatientswere admitted in the Padilla Hospital and recorded using ICD-10 codes showing in Table 1. On the subject of the number of hospitalizations, 91.36% of inpatients were hospitalized once, while 7.52% were hospitalized twice, followed by 0.84% with three hospitalizations and 0.28% hospitalized four times. The sum of hospitalization days was 8214. The average length of stay was 22.88 daysand71.0 % stayed hospitalized more than 10 days (Figure 1). On the other hand, 42.0% of patients were hospitalized previous to the study period.
There was a considerable male predominance (71.15%) among CLLU inpatients. The oldest patient was 96 years and the youngest was 16 years. The mean age (±SD) for females was 54.5(±8.6) years and 63.9(±10.4) years for males. The age range with the highest frequency of inpatients for women was 50-59 years (39.0% of female population), and 60-69 years for men, (34.0% of male population). The leading ICD-10 codes among CLLU inpatients were E11.5 (58.52%), I83.0 (24.73%) and L97 (14.56%).
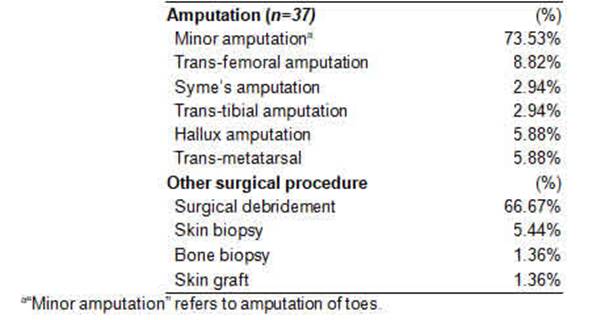
Treatments performed for the management of the ulcer are shown in table 2. Specific treatments for the ulcer and the infection were applied in 19.77%and1.39% had vascular surgeries. A total of 147 surgical procedures were performed, with 25.20% amputationsduring the study (Table 3). There was 9.47% of inpatient with an amputation before this study.Each week a clinical laboratory test (complete blood count, erythrocyte sedimentation rate, blood glucose test, blood urea nitrogen, creatinine blood testand urinalysis) were performed per patient. For these patients, a total of 2347 clinical laboratory tests and 378 bacterial identifications by culturing (antibiotic sensitivity and Gram stain) were performed.
III.C. Hospital cost
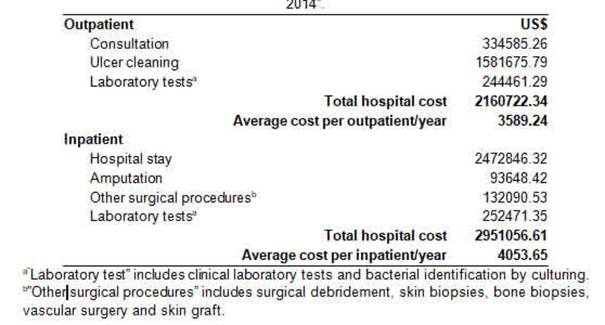
Table 4 shows the estimated costs for CLLU hospitalizations and consultations. The mean cost to a single public Hospital per year was US$4053.65 per inpatient and US$3589.24 per outpatient. Hospital stay (medical and nursing fees, drug treatment, disposables and practice fees) were the main costfactor. The inpatients incurred relevant costs through the self-purchase of topical drugs and medical products (e.g. antibiotics). The majority of the inpatients were Medicare beneficiaries (67.69%) with healthcare coverage. The main cost factor for outpatients was the nursing fees for wound cleansing using saline solution and sterile gauze.
DISCUSION
The management of chronic wounds is complex, time-consuming, and requires high level of resources[3],and can result in an important economic and public health burden, especially in low and middle income countries[13]. In Argentina healthcare is provided by both public and private sectors. Public healthcare service offers free of charge, and universal access to all the population. Despite the significant health and economic burden[17-20],there are not previous studies about epidemiological information and economic impact of chronic wounds in Argentina. This study was undertaken to analyze the demographic and hospital economic characteristics of chronic lower limb ulcers in a public hospital in Argentina.
The most frequent age range of ulceration in this study was between 50 and 59 years. This finding agreed with a nationwide study in Germany using ICD-10 codes for leg ulcers in outpatients and inpatients populations showing that theprobability of developing a wound doubled between the ages of 50 and 60 years[3].
The use of ICD-10 codes allowed us to obtain results with standardized international coding criteria. However, the identification of patients based on the clinical diagnosis and subsequent coding could lead to an underestimation of casesbecause in our community physicians are not used to ICD-10 codes. Besides in some cases, patients were coded by the underlying disease and not by the ulcer-related code. Also, in the first consultation the codification is performed by the hospital's administrative staff. We found a very clear difference in classification distribution between outpatients and inpatients. In the outpatient population, 97% were classified as L97, while only 14.56% of the inpatients received the same classification. This clearly shows that only when the patients are hospitalized they receive an accurate codification. The lack of accurate classification (and maybe of diagnosis) during consultations could be consider as a negative marker explaining the lack of healing effectiveness in this study population.
On the other hand, most of inpatients were E11.5 (58.52%). This result is influenced by the internal organization of the Province Health System (SIPROSA)that derives mainly diabetic patients to this hospital. This also could explain the high male predominance in inpatients (Table 1).Male gender predominance is consistent with many earlier studies[21],[22],[23]. Also, it is possible to suggest that males are more liable to foot trauma and hence they are commoner in diabetic foot ulceration[23].
This study shows major cost associated to wound cleansing. This burden could be underestimating considering that usually patients performed daily home cleansing of the wound or in Primary Health Care Centers, leading to anunderregistration of the procedure.
During this study we observed different markers that are directly related with the lack of therapeutic effectiveness of the applied treatmentsaffecting significantly the hospital cost of CLLU. For example, 8.64% of patients were hospitalized more than once during 2013 and 2014, and 42.0% were hospitalized previous to this study. A second marker was that 71% of patients stayed hospitalized more than 10 daysdue to CLLU complications with an average of 22 days compared to Germany and UK where the mean length of stay was 8.4 days and 12.8 days[11],[24]. Surgical procedures were the third marker. A mean of 0.41 surgeries were performed for each patient, and 25% of these procedures were amputations. Besides, 10.33% of patients were amputated during the study and9.47% previous to this studyshowing a long medical history with low therapeutic effectiveness. Finally, only 19.77% of inpatients received specific treatments for the ulcer, including pro-healing treatments and treatments for infection which could also explain the lack of therapeutic effectiveness comparing to previous studies that focus on specific management of the ulcer[11],[21],[24],[25]. Another hypothesis to this low therapeutic effectiveness is the outpatient ICD-10 code misregistration leading to the use of unspecific or inaccurate treatments protocols for the CLLU healing. The problem of non-healing highlights the importance of effective diagnosis/codification and appropriate treatment[20]. Drew et al. suggest that ensuring effective and timely diagnosis and appropriate treatment is significantly more likely to affect costs[20].
Data on treatment costs for leg ulcers are inconsistent andvary largely depending on disease, health system and evaluation method[7]. For example, in developed countries as US and Germany health system spent annually an average annual cost per patient of US$3846.15 and US$11130, respectively[6],[11].However, in developing countries as Brazil and Peru,DFU costs range from US$400 to US$2700 and US$1022 to US$7360, respectively[13,14]. Our results are consistent to the US costs with an annual average cost of US$3589.24 per outpatient and US$4053.65per inpatient (Table 4).
In several developed countries the estimated costs are based on the full healing of the ulcer[20]and the type of ulcer[4],[14],[21],[26],[27]meanwhile in our study the results shows the annual cost for the management of CLLU. Therefore, we assumed that the healing cost will be higher; this shows the paradox of poverty/excess of expenditure that typically face the health systems of developing countries[28],[29],[30].A major cause is the lack of information in developing countries about the economic burden of CLLU and the lack of evaluation of therapeutic effectiveness that allow optimizing treatments and reducing healing time.
This study had several limitations. Data were obtained from a single hospital. The use of diagnosis codes to identify individuals in our population may not be completely accurate. Individuals may have been misdiagnosed, with some individuals with chronic ulcers coded with a different diagnosis and other individuals without chronic ulcers unintentionally diagnosed as a having an ulcer. In this study, some medical records, classified as CLLU with ICD-10 codification, did not have data on ulcers, therefore information containing in those medical records were eliminated from the analysis. One hypothesis about the misdiagnosis records is that, in 2013 the medical records registration was performed by administrative personnel, not by the medical personnel. In addition the electronic registration system using ICD-10 coding was applied for the first time in 2012, and this could be one of the causes of misregistration. Another limitation could be the prevalence of wound type considering that, in recent years, Padilla Hospital has become in a center for DFU treatment.
CONCLUSION
The costs for the management of chronic wounds in a single public hospital in Argentina amounted to US$ 2951,056.61 in the 2013-2014 period, generating a high economic impact on the public Health System. These costs were mainly associated with wound evolution times, hospitalization times, amputations and ineffective treatments. The results of this study have great implications in the management of public hospitals for the implementation of more efficient data records and adequate follow-up of the patient. Treatment of chronic wounds is time consuming, difficult, and the pathogenesis complicated. The management of chronic wounds in developed and developing countries faces enormous challenges. In this study, despite the underregistration we observed a high cost for the management of outpatient and inpatient CLLU in a single public hospital in Tucumán. Medical records showed an alarming underregistration of CLLU because professionals do not focus on the ulcer healing, but on the treatment of the underlying pathology. This decreases the probability of an accurate calculation of costs and therapeutic effectiveness leading to a vicious circle that involves, underregistration of poor therapeutic effectiveness, maintenance of old therapeutic protocols, with consequent long healing times and associated costs.There is a need to change the form of CLLU registration so that physicians and nurses have a comprehensive assessment and consistent understanding of the wound, leading to the choice of appropriate treatment options for the patient and, for the public Health System to become aware of the problem and take the necessary policies to solve it.
CONFLICT OF INTEREST
All authors declare that they have no conflict of interest.