Services on Demand
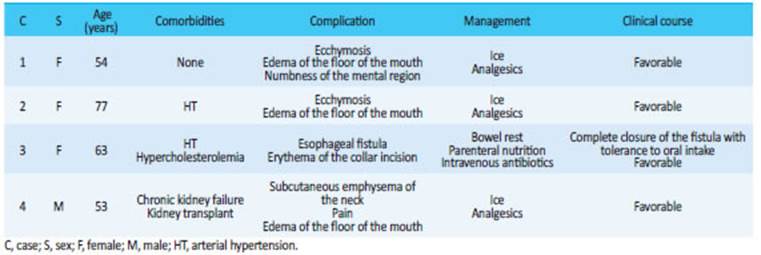
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista argentina de cirugía
Print version ISSN 2250-639XOn-line version ISSN 2250-639X
Rev. argent. cir. vol.113 no.2 Cap. Fed. June 2021
http://dx.doi.org/10.25132/raac.v113.n2.1504.ei
Articles
Transoral endoscopic parathyroidectomy vestibular approach: initial experience in Argentina
1 Servicio de Cirugía de Cabeza y Cuello, División de Cirugía General. Hospital Militar Central. Buenos Aires. Argentina
Introduction
In 1880, Theodor Kocher described the transverse collar incision for conventional thyroidectomy and parathyroidectomy. In those years, the priorities for surgeons were to prevent infection and bleeding1. Over the course of years, the thorough understanding of the anatomy improved the surgical technique, avoiding injury to the recurrent laryngeal nerve and optimizing the management of postoperative hypoparathyroidism.
Nowadays, the cosmetic result is one of the major challenges for the specialized surgeon in an attempt to avoid the stigma of neck scaring.
Natural orifice transluminal endoscopic surgery (NOTES)2 is a procedure with hidden scars. Transoral endoscopic parathyroidectomy vestibular approach (TOEPVA) has so far demonstrated acceptable operative time and reproducibility with excellent cosmetic results3. The aim of this study is to present the first four case series of our experience with this technique in our institution.
Material and methods
This case series corresponds to 4 patients who attended the outpatient clinic of the Head and Neck Surgery Department of Hospital Militar Central between August 2019 and March 2020.
Case report 1: a 54-year-old female patient sought medical advice due to parathormone (PTH) levels of 154 pg/mL (normal value: 15-65 pg/mL) and serum calcium of 12 mg/dL (normal value: 8.2-10.5 mg/ dL). The patient was asymptomatic. Neck ultrasound: solid, hypoechoic nodular image with regular borders, with a size of 14 mm × 4 mm, suggestive of parathyroid adenoma. Parathyroid scintigraphy: solid nodular image 7 mm in size with hypermetabolic activity behind the left thyroid lobe. Diagnosis: primary hyperparathyroidism (PHPT) due to an adenoma of left superior parathyroid gland.
Case report 2: a 77-year-old female patient sought medical advice due PTH levels of 81 pg/mL and serum calcium of 13 mg/dL. The patient was asymptomatic. Neck ultrasound: isoechoic nodule 4 cm × 6 mm in size in the right inferior parathyroid region. Parathyroid scintigraphy: area of increased contrast uptake, with delayed washout suggestive of adenoma. Diagnosis: PHPT due to an adenoma of right inferior parathyroid gland.
In both cases the procedure was performed without complications. Operative time was 150 minutes. Blood loss after vacuum aspiration was 55 mL. Liquid diet was started 7 hours after surgery and soft diet at 14 hours, with adequate tolerance. The laboratory tests performed 6 hours after surgery reported normal serum calcium levels with reduction in PTH levels and the patient was discharged.
Case report 2: a 63 year-old female patient with astenia and adynamia presented elevated PTH levels of 133 pg/mL and serum calcium levels of 12.8 mg/dL. The positron emission tomography (PET) scan showed a hypermetabolic nodular lesion in the left superior paraesophageal space, behind the trachea. Diagnosis: PHPT due to paraesophageal adenoma of the left superior parathyroid gland. During surgery agenesis of the left thyroid lobe was observed and the neck was widely explored. Frozen section examination was performed in multiple samples which were reported as not correlating with parathyroid tissue. An exploratory collar incision was made and the parathyroid adenoma was found in the left superior paraesophageal region. When PTH level decreased by 92.3% (10.3 pg/mL), the surgery was ended. Two drains were placed. The patient presented fever and seropurulent wound drainage 24 hours after surgery. The imaging tests showed a fistula of the upper segment of the esophagus that was treated with bowel rest, parenteral nutrition and intravenous antibiotics for 14 days with the patient still hospitalized. She was followed up at the outpatient clinic and evolved with favorable outcome with spontaneous closure of the fistula on postoperative day 30 (Table 1).
Case report 4: a 53-year-old male patient with a history of chronic kidney failure, right kidney transplant and a diagnosis of tertiary hyperparathyroidism (HPT3) presented with PTH levels of 236 pg/mL and serum calcium levels of 12.2 mg/dL. Parathyroid scintigraphy: focal areas (right superior and inferior parathyroid glands and left inferior parathyroid gland) suggestive of parathyroid hyperplasia. The patient underwent bilateral exploration with subtotal parathyroidectomy; operative time was 270 minutes. The procedure was well tolerated.
In all the cases, PTH levels remained low since the intraoperative measurement and serum calcium remained within normal limits, with no evidence of any increase during follow-up at the outpatient clinic within 6 months after surgery. The result of the pathology report was parathyroid adenoma in the first three cases and parathyroid hyperplasia in case 4.
Surgical technique
Patient positioning, the laparoscopic instruments used and the surgical approach are similar to those described in our previous publication of transoral endoscopic thyroidectomy by vestibular approach (TOETVA)4.
A blood sample should be drawn during induction of anesthesia to determine baseline PTH levels5. Cephalotin 1g was used for antibiotic prophylaxis.
We decided to insert a central 5-mm trocar via a transverse incision and two lateral 5-mm trocars, using a laparoscopic 5-mm optical trocar to enlarge the surgical field and extract the surgical specimen through that port (Fig. 1 A-B).
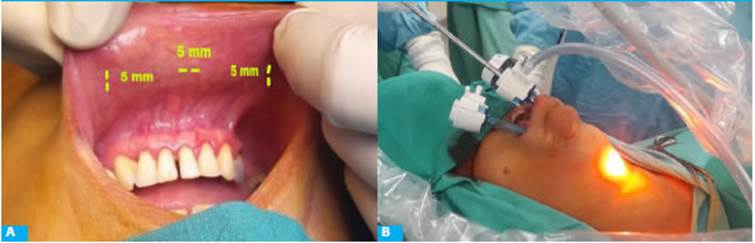
Figure 1 A. Delimitation of the incisions for the inferior vestibular approach. B. Patient positioning and placement of trocars
After inserting the trocars, CO2 is insufflated at a pressure of 6 mm Hg. A traction suture is made in the anterior neck skin6.
The subcutaneous tissue is dissected with electrocautery above the strap muscles7.
The midline raphe is opened with electrocautery and a silk suture is passed from the skin into the strap muscles to retract it laterally from outside8. A blunt dissection is performed to access the tracheoesophageal space and expose the carotid sheath. As dissection continues, the parathyroid glands are visualized are released from the thyroid pole. The recurrent laryngeal nerve is identified by using intraoperative neural monitoring. The affected parathyroid gland, usually enlarged, is identified, resected using high-frequency energy clamps and extracted through the working port or with an endobag if the gland is large (Fig. 2). The surgical specimen is sent for frozen section examination. Fifteen minutes after parathyroidectomy, PTH levels are measured to verify a reduction of 50% below the preoperative baseline level. In case of parathyroid hyperplasia, exploration should be bilateral using the same technique on the contralateral site. Adequate hemostasis is checked. The mucous surface is sutured with separate stitches using Vicryl®.
Discussion
We understood the need to explain this new technique to the patient, with its advantages and possible complications.
We noticed that patients with single parathyroid adenomas undergoing a unilateral approach had shorter operative time, with a more favorable postoperative course than those who required bilateral exploration due to parathyroid hyperplasia.
An unnoticed injury of the gastrointestinal tract should be suspected in any patient with fever or saliva drainage from the surgical site. The diagnosis will be confirmed with imaging tests and managed medically to achieve spontaneous closure. If the clinical course is unfavorable, it may be necessary to explore the surgical site.
So far, there is little information about the indication for transoral surgeries for ectopic parathyroid glands.
Conclusions
TOEPVA requires a long learning curve but could be a safe and reproducible method with favorable cosmetic results9. We believe that it should be implemented in selected cases with favorable anatomy for the vestibular approach and with parathyroid glands in the normal location. The presence of ectopic glands is the main limitation.
Further investigations with a greater number of patients and long-term results will be needed to assess cost-effectiveness, particular situations and management of possible complications.
Acknowledgments:
we are grateful to Servicio de Endocrinología, Anatomía patológica, Bioquímica y Residencia de Cirugía General del Hospital Militar Central 601, Cir. My. Dr. Cosme Argerich, for their par ticipation in the paper and data collection
REFERENCES
1. Russell J, Clark J, Noureldine S, Anuwong A, Al Khadem MG, Kim HY, et al. Transoral thyroidectomy and parathyroidectomy-a North American series of robotic and endoscopic transoral approaches to the central neck. Oral Oncol. 2017; 71:75-80. [ Links ]
2. Witzel K, von Rahden BHA, Kaminski C, Stein HJ. Transoral access for endoscopic thyroid resection. Surg Endosc. 2008; 22:1871-5. [ Links ]
3. Sasanakietkul T, Jitpratoom P, Anuwong A. Transoral endosco pic parathyroidectomy vestibular approach: a novel scarless pa rathyroidsurgery. Surg Endosc. 2017; 31:3755-63. [ Links ]
4. Zalazar A y col. Tiroidectomía transoral endoscópica por abordaje vestibular. Rev Argent Cirug. 2020; 112(2):185-8. [ Links ]
5. Obiols G, Catalán R, Alasa C. Utilidad de la determinación in traoperatoria de parathormona en el tratamiento quirúrgico del hiperparatiroidismo primario por adenoma de paratiroides. Rev Medicina Clínica (Elsevier). 2003; 121(8): 287-91. [ Links ]
6. Dionigi G, Chai YJ, Tufano RP, et al. Transoral endoscopic thyroidec tomy via a vestibular approach: why and how?. Endocrine. 2018; 59;275-9. https://doi.org/10.1007/s12020-017-1451-x [ Links ]
7. Bhargav PRK. Applicability of transoral endoscopic parathyroi dectomy through vestibular route for primary sporadic hyperpa rathyroidism: A South Indian experience. J Minim Access Surg. 2019; 15(2):119-23. [ Links ]
8. Cabane T, Gac Espinoza P, Rappoport Wurgaft D, Rodríguez More no F, Ulloa Suárez J. Paratiroidectomía transoral endoscópica por acceso vestibular oral. Cirugía de paratiroides sin cicatriz. Primer caso realizado en Sudamérica. Rev Cirugía. 2018;70(6). [ Links ]











 text in
text in