Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista argentina de cirugía
Print version ISSN 2250-639XOn-line version ISSN 2250-639X
Rev. argent. cir. vol.115 no.1 Cap. Fed. May 2023
http://dx.doi.org/10.25132/raac.v115.n1.1674
Articles
Effect of the COVID-19 pandemic on non-COVID-19 patients admitted from the emergency department to the surgical ward during the strict phase of the pandemic in Buenos Aires. A cohort study
1 Departamento de Cirugía General, Hospital Italiano de Buenos Aires. Buenos Aires. Argentina.
Introduction
As young health care workers, we have never before seen the spread of such a devastating and contagious disease as COVID-191,2. Initially reported in Wuhan, China, in December 2019, SARS-CoV-2 spread rapidly worldwide. Most countries imposed mandatory lockdowns that were rapidly lifted. However, Argentina holds the record for having one of the world’s longest lockdowns, with social isolation measures including stay-at-home orders except for essential workers, school closures and a ban on gatherings of more than 10 people implemented on March 20 and partially lifted by September 2020.
In surgery, advanced measures as contingency plans to deal with the pandemic always included rescheduling non-urgent consultations and procedures3,4. As in any other catastrophe, some patients with usual surgical conditions still demand care. Therefore, many specialized societies have published their recommendations on deferring elective care. However, emergency conditions require rapid solution5,6.
The evidence from other countries7 suggests reducing elective surgeries and visits to emergency departments, because health care facilities are considered places of high risk of transmission. However, along with the decrease in the number of scheduled consultations, we perceived an increase in emergency cases; in addition, we also noticed that patients seemed to seek medical care at more advanced stages of the disease, thus requiring more invasive procedures than in the pre-COVID-19 era.
Therefore, the primary objective of this study was to compare variations in admissions, type and severity of the disease, and surgical outcomes in non- COVID-19 emergency admissions to our department of surgery between patients admitted during the strict lockdown phase of the pandemic versus the pre-pandemic phase. As secondary objectives, we performed a sub-analysis of common surgical conditions, as appendicitis, biliary disease, diverticulitis and complicated tumors.
Material and Methods
We conducted an observational, ambispective study, including all patients >18 years who consulted the department of emergency surgery of Hospital Italiano de Buenos Aires, required hospitalization, and tested negative for COVID-19 on admission between March 20 and July 31, 2020 (pandemic group, PG). These patients were compared with a cohort admitted during the same period in 2019 (control group, CG). All the patients were followedup for 30 days to evaluate short-term outcomes. Demographics and clinical data were retrieved from the electronic medical records: age, sex, body mass index (BMI), comorbidities, diagnosis after admission, delay from onset of symptoms to consultation in hours, need for emergency surgery, delay from diagnosis to surgery in hours, operative time in minutes, postoperative complications according to the Dindo Clavien (DC) classification8 and length of hospital stay.
Disease severity on presentation was classified into 3 clinical stages based on the National Early Warning Score (NEWS)29: patients with organ/ system failure were included in the severe stage, those presenting with fever >38°C, white blood cell count >12 000 or <4000, tachycardia or tachypnea were included in the moderate stage, and stable patients who did not meet the criteria for moderate or severe stage were considered in the mild stage.
Quantitative variables are presented as mean and standard deviation, or median and interquartile range, according to their distribution, and were compared using the chi-square test. Categorical variables are expressed as absolute and relative frequencies in percentage and were compared using the Mann- Whitney test or t test, according to the distribution observed. A p value < 0.05 was considered statistically significant. A multiple stepwise logistic regression model including potential confounders was performed to evaluate the surgery group (PG or CG) as an independent factor of morbidity.
All the statistical calculations were performed using STATA 13.0 software package. This investigation was prospectively approved by the institutional review board (number 5684). The study was reported following the STROCSS guideline10.
Results
A total of 651 patients were admitted from the emergency area to the Department of General Surgery during the study periods. The number of patients admitted from the emergency department and the percentage of those who underwent surgery was 346 and 80% for the PG, respectively, and 305 and 76% for the CG, respectively (p = 0.157).
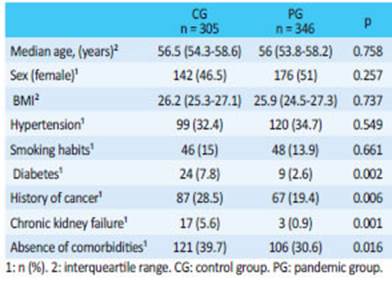
The demographic and clinical characteristics are summarized in Table 1. There were no significant differences in age, sex and BMI. However, there was a significant reduction in patients with comorbidities in the PG compared with the CG: history of cancer, diabetes and chronic renal disease.
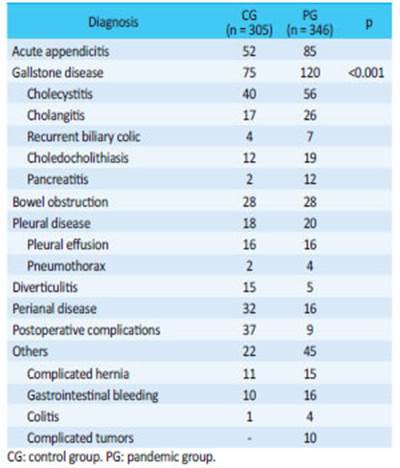
There was a marked reduction in common complaints as perianal abscess and mild diverticulitis (n = 16 vs. n = 32, p < 0.001) and a marked increase in admissions of patients with gallstone disease when comparing both groups (n = 120 vs. n = 75, p < 0.001) for GP vs. CG). Of interest, 10 patients in the PG were admitted with diagnosis of complicated tumor (bleeding tumor and occlusion of the gastrointestinal tract), which had not been observed during the CG. The rest of the distribution of patients in both cohorts are shown in Table 2.
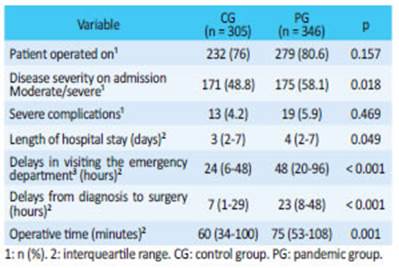
In the PG, more patients attended the emergency department with moderate or severe disease compared with patients in the CG. In addition, mean hospital length of stay was longer in the PG. During the pandemic, there was a global significant delay in time from symptom onset to consultation and in time from diagnosis to surgery. In addition, mean operative time increased (Table 3).
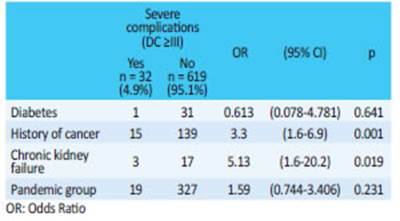
There were no significant differences in major complications (DC) ≥ grade 3), 5.49% for the PG and 4.2% for the CG (p = 0.469). On multivariate analysis, only chronic renal failure and a history of cancer were independent factors for morbidity (Table 4).
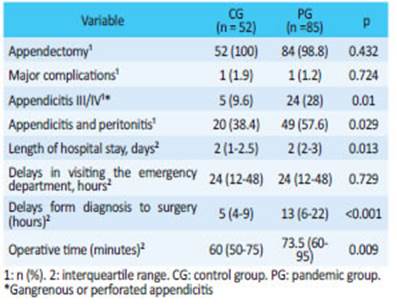
None of the patients of this study died during follow-up. In the PG, time from diagnosis to surgery was significantly delayed in patients with appendicitis, they presented with more severe condition, had associated peritonitis and underwent longer procedures. However, this did not affect major postoperative complications (DC ≥ grade 3) (Table 5).
A similar pattern was observed when we analyzed patients with diverticulitis, with a delay from diagnosis to surgery during the pandemic (39.5 hours, IQR 14-77 vs. 0 hours, IQR 0-3.5; p = 0.003, PG vs. CG) and a longer length of hospital stay (7 days, IQR 6-25 vs. 4 days, IQR 2-8, p = 0.028, PG vs. CG). There were no differences in the rate of diverticulitis stage III or IV of the Hinchey classification (60% vs. 20%, p = 0.091, PG vs. CG) or major postoperative complications (DC ≥ grade 3) (n = 1, 20% vs. n = 0; 0%, p = 0.07, PG vs. CG).
Discussion
Several papers on SARS-CoV-2 and COVID-19 have been published since the outbreak. But other prevalent diseases still occur, and many articles have reported that patients are delaying or avoiding medical care because they are afraid of becoming infected with COVID-1911. The effect of the COVID-19 quarantine in patients without COVID-19 in the Department of Emergency Surgery is a real problem, and its actual extent has not been fully determined yet. Our findings show that, unlike the common trend in most countries worldwide as Italy, Scotland, New Zealand and South Africa,12,13 we did not observe a decrease in Emergency Department admissions, but rather quite the contrary. This could be due to the long mandatory quarantine in our community.
Of note, unlike other studies,14 patients in the CG were frailer than those admitted during the pandemic (Table 1) and had more comorbidities (including diabetes, cancer, or a history of chronic kidney disease). We admitted more patients with complicated benign diseases as inflammatory biliary tract conditions, i.e., cholangitis and pancreatitis, probably because all scheduled non-urgent surgeries such as laparoscopic cholecystectomy were canceled, which resulted in a higher incidence of patients with complicated gallstones, as Cano-Valderrama et al. reported9.
In addition, we admitted patients with complicated neoplasms, possibly due to less outpatient consultations and less screening endoscopies or deferred consultations for fear of infection. In agreement with our findings, a prospective-retrospective observational study15 concluded that fear of infection with COVID-19 may result in a clear reduction in hospital visits and, for the time being, with an unknown impact on missed or late diagnoses. This may be reflected in the significant decline in detecting gastrointestinal cancer worldwide, and a concomitant increase in the number of cancer presentations at more advanced stages11.
As in other studies16-18 the overall analysis showed a marked difference in surgical patients with acute disease, delays from symptom onset to consultation, delays from diagnosis to surgery and longer operative time. However, we did not find an increase in Clavien-Dindo complications ≥ grade 3, as in the publication by Angeramo et al.19-21 who reported a high rate of complications including intra-abdominal abscesses and need for repeated surgery in a series of patients with appendicitis during 30-day follow-up. It is noteworthy that the fact waiting for the results of swabs to detect SARS-CoV-2 was the cause of the delay from admission to surgery, unless the consultant in charge considered surgery an emergency; in this case, the surgeons used level 3 personal protective equipment22-24.
We believe that the results of our study reflect appropriate patient management and outcomes while maintaining our high level of care, always protecting our staff by implementing all the safety protocols recommended by the international scientific societies1,2,4.
The limitations of our study are due to its retrospective methodological design. The lack of randomization could have introduced confounder factors that could have biased the results. However, the surgical team, the procedural techniques, the materials used and the perioperative management did not change during the period covered in the study.
Conclusion
During the pandemic we observed an increase in urgent surgical procedures, particularly in those diseases in which scheduled surgeries were postponed. In our institution, we observed an increase in the number of admissions for gallstone disease and complicated gastrointestinal tumors. The patients consulted with more advanced stages of disease, but this had no impact on postoperative morbidity or mortality, demonstrating that it was possible to maintain surgical outcomes despite delayed consultation.
Referencias bibliográficas /References
1. COVID-19 and Surgery. [cited 5 Mar 2021]. Available: Available: https://www.facs.org/COVID-19 [ Links ]
2. COVID-19: Recommendations for Management of Elective Surgical Procedures. [cited 5 Mar 2021]. Available: Available: https://www.facs.org/COVID-19/clinical-guidance/elective-surgery [ Links ]
3. Sulime Diseño de Soluciones SLU. Inicio. [cited 5 Mar 2021]. Available: Available: https://www.aegastro.es/ [ Links ]
4. McGuinness MJ, Harmston C. The effect of national public health interventions for COVID-19 on emergency general surgery in Northland, New Zealand. ANZ J Surg. 2021. doi:10.1111/ans.16562 [ Links ]
5. COVID-19 and Surgery. [cited 5 Mar 2021]. Available: Available: https://www.facs.org/COVID-19 [ Links ]
6. COVID-19: Recommendations for Management of Elective Surgical Procedures. [cited 5 Mar 2021]. Available: Available: https://www.facs.org/COVID-19/clinical-guidance/elective-surgery [ Links ]
7. Søreide K, Hallet J, Matthews JB, Schnitzbauer AA, Line PD, Lai PBS, et al. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg. 2020; 107:1250-61. [ Links ]
8. Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240: 205- 13. [ Links ]
9. National Early Warning Score (NEWS) 2. 19 Dec 2017 [cited 5 Apr 2021]. Available: Available: https://www.rcplondon.ac.uk/projects/outputs/national-early-warning-score-news-2 [ Links ]
10. Agha R, Abdall-Razak A, Crossley E, Dowlut N, Iosifidis C, Mathew G. STROCSS 2019 Guideline: Strengthening the reporting of cohort studies in surgery. Int J Surg. 2019;72. doi: 10.1016/j.ijsu.2019.11.002 [ Links ]
11. Mitchell EP. Declines in Cancer Screening During COVID-19 Pandemic. J Natl Med Assoc. 2020;112: 563-4. [ Links ]
12. Surgical emergencies during SARS-CoV-2 pandemic lockdown: what happened? 27 Nov 2020 [cited 5 Mar 2021]. Available: Available: https://www.europeanreview.org/article/23851 [ Links ]
13. Dick L, Green J, Brown J, Kennedy E, Cassidy R, Othman S, et al. Changes in Emergency General Surgery During COVID-19 in Scotland: A Prospective Cohort Study. World J Surg. 2020;44(1):3590-4. [ Links ]
14. Cano-Valderrama O, Morales X, Ferrigni CJ, Martín-Antona E, Turrado V, García A, et al. Acute Care Surgery during the COVID-19 pandemic in Spain: Changes in volume, causes and complications. A multicentre retrospective cohort study. Int J Surg. 2020; 80:157-61. [ Links ]
15. Franchini S, Spessot M, Landoni G, Piani C, Cappelletti C, Mariani F, et al. Stranger Months: How SARS-CoV-2, Fear of Contagion, and Lockdown Measures Impacted Attendance and Clinical Activity During February and March 2020 at an Urban Emergency Department in Milan. Disaster Med Public Health Prep. 2020;15(5):1-23. [ Links ]
16. Kelly ME, Murphy E, Bolger JC, Cahill RA. COVID-19 and the treatment of acute appendicitis in Ireland: a new era or shortterm pivot? Colorectal Dis. 2020;22: 648-9. [ Links ]
17. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020;4:e10-e11. [ Links ]
18. Patel R, Hainsworth AJ, Devlin K, Patel JH, Karim A. Frequency and severity of general surgical emergencies during the COVID-19 pandemic: single-centre experience from a large metropolitan teaching hospital. Ann R Coll Surg Engl. 2020; 102(6):1-6. [ Links ]
19. Angeramo CA, Dreifuss NH, Schlottmann F, Rotholtz NA. More Severe Presentations of Acute Appendicitis During COVID-19. J Gastrointest Surg. 2021;25(7):1902-4. doi:10.1007/s11605-020-04892-0 [ Links ]
20. Dreifuss NH, Schlottmann F, Sadava EE, Rotholtz NA. Acute appendicitis does not quarantine: surgical outcomes of laparoscopic appendectomy in COVID-19 times. Br J Surg. 2020; 107: e368-e369. [ Links ]
21. Barreiro MC y cols. COVID-19: tratamiento quirúrgico de la apendicitis aguda. Rev Argent Cirug. 2020;112(4):450-8. [ Links ]
22. Ortiz E y col. Recomendaciones COVID-19: generales. Rev Argent Cirug. 2020;112(3):228-33. [ Links ]
23. Seretis C, Archer L, Lalou L, Yahia S, Katz C, Parwaiz I, et al. Minimal impact of COVID-19 outbreak on the postoperative morbidity and mortality following emergency general surgery procedures: results from a 3-month observational period. Med Glas. 2020; 17:275-8. [ Links ]
24. Stewart CL, Thornblade LW, Diamond DJ, Fong Y, Melstrom LG. Personal Protective Equipment and COVID-19: A Review for Surgeons. Ann Surg. 2020;272: e132-e138. [ Links ]
Received: February 03, 2022; Accepted: May 10, 2022











 text in
text in