Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista argentina de cirugía
Print version ISSN 2250-639XOn-line version ISSN 2250-639X
Rev. argent. cir. vol.115 no.1 Cap. Fed. May 2023
http://dx.doi.org/10.25132/raac.v115.n1.1599
Articles
Multisystem inflammatory syndrome post-COVID as acute abdominal pain in pediatrics
Coronavirus disease 2019 (COVID-19) has impacted on health systems worldwide. Since its onset in China, the virus has spread around the world and has infected 46 806 000 people and killed more than 1 204 0001,2. Although at the beginning of the pandemic children and adolescents were considered to be carriers of the virus or to have only mild disease a multisystem hyperinflammatory state with multiple organ failure has been occurring since May 2020, which can even mimic an abdominal surgical emergency due to right iliac fossa pain3,4.
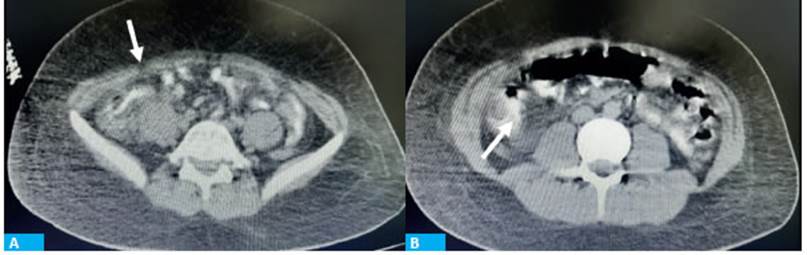
A 15-year-old otherwise healthy male patient was admitted to the emergency department due to fever associated with diffuse abdominal pain and diarrhea that started one week before. He sought medical care 72 hours before admission due to fever and headache; a nasopharyngeal swab was obtained in the setting of the pandemic and the RT-PCR was negative for SARSCoV- 2. On physical examination the patient presented hypotension and fever. The abdomen was soft, diffusely tender, with no guarding or rebound tenderness. The laboratory test showed 17 900 white blood cells associated with acute kidney failure (creatinine level 2.6 mg/dL). The abdominal ultrasound showed multiple enlarged mesenteric lymph nodes in the right iliac fossa and retroperitoneum measuring 4 mm, with increased echogenicity. A CT scan showed pulmonary infiltrates in both lung bases, inflammation and thickening of the terminal ileum and ascending colon, with rarefaction of adjacent planes. The vermiform appendix was identified slightly enlarged.
As the patient evolved in the emergency department with sustained hypotension refractory to fluid resuscitation and hemodynamic instability, he was transferred to the intensive care unit (ICU) where therapy with pressor agents was initiated. The complementary tests revealed significant increase in inflammatory markers: D-dimer 4746 mg/mL, procalcitonin 101.53 mg/mL, NT-proBNP > 25 000 pg/ mL, ultrasensitive troponin 452.1 ng/L and positive COVID-19 test by ELISA method with IgG antibodies titer of 4.59. The echocardiogram reported moderate left ventricular dysfunction, global hypokinesia and a small thrombus attached to the apex without impairing contractility. Surgical management was postponed and medical treatment was initiated with intravenous immunoglobulin associated with corticosteroids for 3 days and anticoagulation, with favorable response. The patient evolved with improved clinical status, absence of abdominal pain and normal organ function, and was transferred to the general pediatric ward 72 hours later. Multisystem inflammatory syndrome in children and adolescents is defined by the World Health Organization (WHO) and the Center for Disease Control and Prevention (CDC) on the basis of 5 elements: patient’s age, persistent fever, elevated markers of inflammation by laboratory tests, manifestation of organ failure and absence of other probable diagnoses. Most cases present with persistent fever lasting more than 4 days associated with diffuse abdominal pain and diarrhea and sometimes cutaneous involvement. The differential diagnoses include Kawasaki’s disease, toxic shock syndrome as acute abdomen due to a nonsurgical condition (systemic involvement), and acute appendicitis as an abdominal surgical emergency3,5. The complementary tests findings include high white cell count with predominantly elevated neutrophils and lymphocytopenia, and elevated markers of inflammation such as C-reactive protein, procalcitonin and D-dimer6.
The imaging tests reveal multiple enlarged mesenteric lymph nodes on ultrasound examination, inflammation and increased thickness of the terminal ileum and colon, with a preserved vermiform appendix. We should also mention cardiac involvement characterized by decreased left ventricular ejection fraction in association with significant elevation of specific markers as troponins and proBNP. This life-threatening condition should be rapidly recognized and suspected due to its rapid progression to shock with multiple organ failure, sustained hypotension refractory to fluid resuscitation with requirement of pressor agents and need for intensive care. The recommended treatment according to the current experience is based on hyperimmune globulins associated with corticosteroids.
Our experience with the patient helps to document and contribute to scientific knowledge about this new disease, especially for pediatricians and surgeons, who in times of pandemic must deal with patients with abdominal pain and fever with suspected appendicitis. Although thorough physical examination and clinical findings should guide diagnosis and treatment, as the nature of the clinical findings resemble acute appendicitis in pediatric patients with COVID-19, we emphasize the importance of ruling out such diagnosis by complementary imaging tests as ultrasound, computed tomography scan or both. Also, nasopharyngeal swab or serological test for COVID-19 should be performed in the context of this pandemic.
Referencias bibliográficas /References
1. World Health Organization. Multisystem inflammatory syndrome in children and adolescents with COVID-19. Published May 15, 2020. [ Links ]
2. Centers for Disease Control and Prevention. Emergency preparedness and response: multisystem inflammatory syndrome in children (MIS-C) associated with coronavirus disease 2019 (COVID-19). [ Links ]
3. Feldstein LR, Rose EB, Horwitz SM, et al. Multisystem inflammatory syndrome in U.S. children and adolescents. N Engl J Med. 2020; (NEJMoa2021680). https://doi.org/10.1056/NEJMoa2021680 [ Links ]
4. Mubbasheer A, Shailesh A, Moreira A, et al. Multisystem inflammatory syndrome in children: A systematic review. EClinicalMedicine. 2020; 26: 100527; https://doi.org/10.1016/j.eclinm.2020.100527 [ Links ]
5. Abrams J.Y., Godfred-Cato S.E., Oster M.E., Chow E.J., Koumans E.H., Bryant B. Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with SARS-CoV-2: A Systematic Review. J Pediatr. 2020;226:45-54. [ Links ]
6. Hameed S, Elbaaly H, Reid CE, Santos RM, Shivamurthy V, Wong J, et al. Spectrum of imaging findings on chest radiographs, US, CT, and MRI images in multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19. Radiology. 2020;298(1). [ Links ]
Received: March 25, 2021; Accepted: August 19, 2021











 text in
text in