Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Acta Odontológica Latinoamericana
versión On-line ISSN 1852-4834
Acta odontol. latinoam. vol.22 no.1 Buenos Aires abr. 2009
ARTÍCULOS ORIGINALES
Clinical evaluation of the use of three anestheticsin endodontics
Cláudio Maniglia-Ferreira1, Fábio Almeida-Gomes1,2, Bruno Carvalho-Sousa2, Antonio V. H. Barbosa2, Carla C. S. A. Lins2, Fabrício D. Souza2, Roberto A. Santos2
1 Department of Endodontics, University of Fortaleza.
2 Department of Endodontics, University of Pernambuco.
CORRESPONDENCE Fabio de Almeida Gomes Rua Arquiteto Reginaldo Rangel, 155, ap. 1403 Papicu, Fortaleza, CE, Brazil, CEP: 60191-250. E-mail: fabiogomesce@yahoo.com.br
ABSTRACT
This study compared three anesthetics widely used in endodontics and analyzed the following variables: amount necessary to achieve adequate anesthesia; anesthetic efficacy, defined as no sensation during endodontic treatment; anesthetic duration; and cost-benefit. Sixty patients diagnosed with irreversible pulpitis of a mandibular molar were selected at the Dental Emergency Center of Universidade de Fortaleza, Brazil. Patients were randomly divided into three groups of 20 and were administered one of three anesthetic solutions for conventional regional block: 2% lidocaine with 1:2,500 phenylephrine; 2% mepivacaine with 1:100,000 adrenaline and 4% articaine with 1:100,000 epinephrine. The following variables were studied: number of cartridges necessary to obtain anesthetic success; anesthetic efficacy, defined as no sensation during endodontic procedures; anesthetic duration; cost-benefit ratio for each anesthetic. Mean number of cartridges necessary to obtain anesthetic success was 2.76, and there was no statistically significant difference between the anesthetics used. Lidocaine had the best costbenefit ratio. All anesthetics used were clinically efficient and had equivalent results for endodontic treatment.
Key words: Anesthesiology; Pulpitis; Endodontics.
RESUMO
Avaliação clínica do uso de três bases anestésicas utilizadas em endodontia
Foram selecionados, do servico de urgencia odontologica da Universidade de Fortaleza, sessenta pacientes que apresentaram diagnostico clinico de pulpite irreversivel em molares inferiores. Os pacientes foram distribuidos aleatoriamente em tres grupos de 20, sendo que para cada grupo utilizou-se um tipo de anestesico. A tecnica de bloqueio regional foi utilizada para todos os casos. No grupo I foi utilizado o anestesico Lidocaina 2% com fenilefrina (1:2.500) (Novocol 100, SSWhite, Brasil), no grupo II a Mepivacaina 2% com adrenalina (1:100.000) (Mepiadre, DFL, Brasil), e no grupo III a Articaina 4% com epinefrina (1:100.000) (Dentsply Pharmaceutical, Brasil). Foram observados: a) quantidade de tubetes necessarios para se ter uma condicao adequada de analgesia, b) eficacia do anestesico em funcao da ausencia de sensibilidade oferecida no momento do tratamento endodontico, c) tempo de trabalho, d) relacao custo-beneficio para cada anestesico. A analise da dor foi mensurada com auxilio da escala VAS. Todos os dentes tiveram os tratamentos endodonticos finalizados na mesma sessao. A media geral de tubetes necessarios para se obter condicao de anestesia adequada foi de 2,76 tubetes, sendo que nao foi encontrada diferenca estatisticamente significante entre os anestesicos utilizados (p=0,8219). A comparacao entre as relacoes de custo beneficio mostrou-se favoravel para a lidocaina (p=0,0001), seguida pela mepivacaina e articaina. Pode-se concluir que todos os anestesicos utilizados mostraram-se clinicamente eficientes e iguais diante do tratamento endodontico.
Palavras chaves: Anestesiologia; Pulpite; Endodontia.
INTRODUCTION
The management of pain and anxiety in the dental office is a very important factor in gaining a patient’s trust1. Over 50% of Americans avoid dental treatments because of fear of pain2-6, and similar findings have been reported in Brazilian studies7. Interviews with patients revealed that dental appointments are associated with pain6. Pain and anxiety are different but closely related problems. Pain due to dental treatments can be controlled with carefully performed local anesthetic techniques. Anxiety can also be managed and reduced3,7. To gain a patient’s trust, dentists should identify the origin of anxiety and deal with its causes3. In most areas of dentistry, anxiety is associated with pain during or after a treatment. Therefore, when pain is controlled, anxiety may also be controlled. Pain control is a major concern in endodontics because patients usually associate endodontic treatments with appointments full of pain and anxiety5. Satisfactory answers for both the endodontist and the patient depend on careful preparation of the area to be treated before endodontic access. To ensure patient comfort, the tooth should be completely anesthetized and isolated with a rubber dam8,9. Local anesthetics are drugs that block nerve impulse generation and conduction and act primarily on neuronal cell membranes10,11.
In some areas of the mouth, anesthetic success can only be achieved with the use of a regional block. The prevent the transmission of afferent impulses; the anesthetic agent should be delivered as close as possible to the point where the nerve is attached to bone1,9. A regional block is also often used when anesthetic infiltration fails because of inflammation or infections, which reduce the pH in the area. In such cases, anesthesia delivered at a distant site is indicated1,8,12,13. Inferior alveolar nerve block is the technique most often used in endodontic treatments6. However, the pulp of mandibular teeth is not always successfully anesthetized: failure rates range from 10% to 39%14,15.
Inferior alveolar nerve block is used for the endodontic treatment of mandibular molars6,11,16. The penetration of the needle should be accurate, and the anesthetic should be injected as close as possible to the mandibular foramen17. According to Kaufman et al.18 (1984), 90% of the dental surgeons in the United States reported local anesthesia failures, 88% of which were associated with the difficulty in performing an inferior alveolar nerve block. Allergic reactions to local anesthetics are found in only 1% of the cases19. Most reactions of patients that underwent dental treatments were caused by anxiety rather than anesthetic toxicity20. The use of articaine is contraindicated for patients that are hypersensitive to drugs that contain sulfur21. According to the literature, lidocaine, mepivacaine and articaine are anesthetic agents that efficiently control pain during endodontic procedures10-13,19,22.
They are frequently used with vasoconstrictors, such as adrenaline, noradrenaline or phenylephrine, in concentrations of 1:50,000 to 1:100,000 (noradrenaline and adrenaline) or 1:2,500 (phenylephrine)17,23. In patients with systemic diseases, anesthetics should be used without vasoconstrictors20. The best anesthetic agent for these patients is mepivacaine because of its vasodilating action. Mepivacaine provides greater safety because of its low absorption, which reduces the risk of high blood concentrations and overdoses10,23. Such effect is observed clinically: mepivacaine without a vasoconstrictor provides 20 to 40 minutes of pulp anesthesia, whereas lidocaine provides less than 5 minutes10.
Maniglia-Ferreira et al.24 (2002) found that lidocaine with adrenaline or noradrenaline had the best costbenefit ratio of all local anesthetic and vasoconstrictor combinations that they evaluated, and that they were as efficient as mepivacaine with other vasoconstrictors. Claffey et al.6 (2004) compared the efficacy of lidocaine and articaine, both with 1:100,000 adrenaline, and did not find statistically significant differences between them. They discussed the importance of adequate administration techniques, particularly for an inferior alveolar nerve block, a recommendation also made by Mikessel et al.22 (2005). Moreover, the use of lidocaine with 1:100,000 adrenaline is largely accepted for the treatment of patients with diabetes, hypertension or cardiopathy, as well as for pregnant women11,22. This study compared three anesthetic agents widely used in endodontics and analyzed the following variables: amount necessary to achieve adequate anesthesia; anesthetic efficacy, defined as no sensation during endodontic treatment; anesthetic duration; and cost-benefit ratio.
MATERIAL AND METHODS
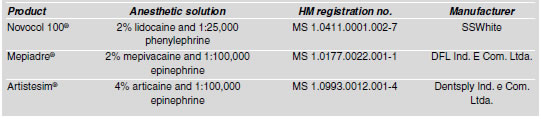
This quantitative clinical cross-sectional study analyzed the efficacy of three Brazilian anesthetics (Table 1) used for inferior alveolar nerve block in patients with irreversible pulpitis. These anesthetic agents, approved by the Brazilian Ministry of Health, are currently used in Dentistry. Therefore, patients were not exposed to any type of discomfort or risk. The Fortaleza University has a contract with the Anjos do Resgate Company, which provides paramedic assistance and patient transportation to hospitals. This study was approved by the Ethics Committee of Fortaleza University (Coetica, UNIFOR), under number 088/2007.
Table 1: Commercial names, anesthetic agent, manufacturer and Brazilian Health Ministry (HM) registration number of the products used in this study
Study groups: Sixty healthy volunteers of both sexes aged 21 to 48 years were selected at the emergency service of the School of Dentistry of Fortaleza University. All patients had irreversible pulpitis of a mandibular molar and had to undergo inferior alveolar nerve block. All teeth were treated endodontically according to the norms and procedures of the Endodontics Department of the University where the study was conducted. Before starting the treatment, patients answered a questionnaire about symptoms and general and oral health. The following data were collected: diagnosis, dental history, allergies and systemic diseases. Patients that were hypersensitive to any of the anesthetics used in the study or had any systemic disease (hypertension or cardiopathy) were excluded from the study25. All patients received information about the study and signed an informed consent form. All anesthetics are approved by the Brazilian Health Ministry for use in dentistry although few studies have compared them or investigated their use in cases of irreversible pulpitis.
Methods: Before the beginning of endodontic treatment, all patients underwent inferior alveolar nerve block with one of the anesthetics under study. All teeth were vital and had to undergo endodontic treatment because of irreversible pulpitis. All blocks were performed a single operator. The patients were randomly allocated to three groups of 20 participants each. In group I, the anesthetic used was 2% lidocaine with 1:25,000 phenylephrine (Novocol 100, SSWhite, Brazil); in group II, 2% mepivacaine with 1:100,000 adrenaline (Mepiadre, DFL, Brazil); and in group III, 4% articaine with 1:100,000 epinephrine (Dentsply Pharmaceutical, Brazil). The technique used was the inferior alveolar nerve block, and one cartridge of each anesthetic was used initially. If anesthesia was not achieved and there were no other signs of inferior alveolar nerve block (lower lip or tip of the tongue numbness), another half cartridge was administered 5 minutes after the first injection, and the same procedure was repeated until anesthetic success was achieved. The same procedure was followed if the patient reported any sensation during clinical procedures. The following parameters were analyzed: (a) number of cartridges necessary to achieve anesthesia; (b) anesthetic efficacy, defined as no sensation during endodontic treatment; (c) anesthetic duration; (d) cost-benefit. All data were collected on a table for later analysis. The results were classified into four categories according to scores: no pain = zero (0); minor pain (includes very weak and weak pain) = 9 to 54; moderate = 54 to 114; and intense > 114.
The pulps of all teeth were removed, the canals were cleaned and shaped, and the foramina were debrided. After cleaning and shaping, the teeth were filled with gutta-percha cones (Konne, Belo Horizonte, MG, Brazil) and Grossman cement (Endofil, Dentsply, Petropolis, RJ, Brazil). Statistical analysis of results: All results were collected on a table and analyzed statistically using the BioEstat for Windows 2.0 software. The Mann-Whitney test was used for the statistical analysis of data.
RESULTS
Pain was assessed with a visual analog scale (VAS)6 (Table 2), and the results of this study are shown in Table 3. Overall mean number of cartridges to achieve anesthesia was 2.76, and there was no statistically significant difference between anesthetics (p=0.8219).
Table 2: Visual analog scale (mm) to assess pain
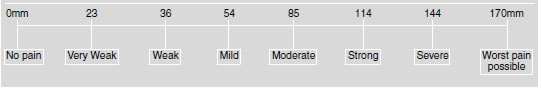
Table 3: Mean values of data analyzed after the use of different anesthetic agents
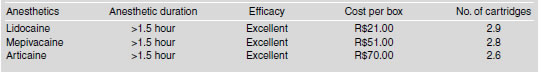
Lidocaine had the best cost-benefit ratio; its cost was significantly lower than that of the other anesthetics (p=0.0001). Similarly, the comparison between mepivacaine and articaine showed that the cost of articaine was significantly higher (p=0.0001). This significant difference is particularly important because all the anesthetics under study had equal clinical results in the analysis of the other variables. Therefore, cost becomes a differential factor in determining which anesthetic to use. In this study, lidocaine (SSWhite) had the best results. No clinical differences were found in the analysis of anesthetic duration or efficacy.
DISCUSSION
Pain is essentially an abnormal emotional state that results from pathologic activity of a specific sensory system. Although difficult to define and investigate, pain is known to be associated with a specific network of nerve fibers23. Lidocaine and mepivacaine have been used efficiently for local anesthesia in dentistry. In April 2000, articaine was introduced in the United States as a superior analgesic drug26. However, one of its possible disadvantages is the use of a methylparaben preservative, which may cause contact dermatitis and hypersensitivity21.
Lidocaine is the anesthetic most often used and studied for local anesthesia in dentistry. However, after the development of new anesthetic drugs, several studies have compared them and investigated their efficacy25. Cohen et al.12 found that 3% mepivacaine could be used without a vasoconstrictor for local anesthesia and was as efficient as 2% lidocaine with 1:100,000 epinephrine for inferior alveolar nerve block. According to some authors, failure of inferior alveolar block is usually assigned to technical errors or to the ramifications of nerve branches15, and not to the fact that vasoconstrictors are used in combination with anesthetics or not20, because the number of failures remains stable despite the evolution of anesthetics27. However, the combination of vasoconstrictors and anesthetics is very important in endodontic treatments because appointments are relatively long. We believe that vasoconstrictors should be used for all endodontic treatments. According to Malamed28 (1993), the adrenal cortex releases about 280 mg/min adrenaline and 56 mg/min noradrenaline in stressful situations, whereas a vasoconstrictor at 1:50,000 releases 1 mg/min. This is in agreement with the results reported by Weine8 (1989) and Mees et al.29 (1997), who found that it is better to use anesthetics with a vasoconstrictor in patients with systemic diseases than to run the risk of exposing patients to stressful situations caused by pain during the procedures and, therefore, risk the release of a larger amount of vasoconstrictors from their own organism, which may affect their health.
Anesthetic duration and amount of anesthetics necessary to achieve ideal working conditions in our study are in agreement with findings reported by Wallace et al.16 (1985). Those authors showed that the amount of anesthetics required for molars with pulpitis was greater than that required for a healthy tooth. Hinkley et al.23 (1991) achieved anesthetic success in a healthy tooth using smaller amounts of anesthetics than in our study, in which teeth had pulpitis. Bigby et al.27 (2006) conducted a similar study and suggested that complementary anesthetic techniques should be used in case an inferior alveolar nerve block was necessary. Similar situations are routinely observed in the dental emergency service at Fortaleza University. In our study, regardless of the anesthetic used, 10% of the patients reported sensation during treatment. This percentage should not be classified as a technical error, but rather as a consequence of parallel innervations of the buccal nerve, a fact that was also reported in other recent studies14,15.
Stress and anxiety due to pain may make the patient more sensitive to endodontic treatment, and the dentist may, therefore, use a greater amount of anesthetics for local anesthesia25. Such situation was observed during this study, in which all patients had intense pain due to acute pulpitis. The use of anesthetics sold in cartridges adds safety to the measurement of doses during injection. It is known that healthy patients weighing 50 kg to 70 kg may need up to 300 mg of lidocaine, whereas the amount for mepivacaine and articaine is 400 mg when combined with a vasoconstrictor. Therefore, 5.5 cartridges of any of the anesthetics in this study can be safely used19. Such findings suggest that higher doses can be safely, but not indiscriminately, used when necessary. Our study demonstrated that the anesthetics under study did not achieve adequate inferior alveolar nerve block in patients with irreversible pulpitis when the mean amount injected was less than 2.6 cartridges, an amount that is safe. This study also contributed to the general knowledge about local anesthesia. Clinical dentists often cannot perform an endodontic or urgent procedure because of anesthetic failures, a situation that may result in pain and stress for the patient30. Local anesthetics do not act only in the tissue where they are injected, but also affect other organs that function according to the conduction or transmission of nerve impulses, such as the central nervous system, the cardiovascular system, and all types of muscle fibers6.
CONCLUSIONS
Anesthesia is one of the occurrences of current dental treatments, but the comparison of 3 anesthetic agents in this study revealed that:
There were no statistically significant differences in efficacy, anesthetic duration, or amount necessary to achieve anesthesia;
10% of the patients, regardless of type of anesthetic used, reported sensation during procedures, which suggests that complementary techniques should be used to achieve anesthetic success; Lidocaine had the best cost-benefit ratio (p=0.0001), followed by mepivacaine and articaine.
1. Cohen S, Burns RC. Pathways of the pulp. 7th ed. Saint Louis: Mosby 2004. [ Links ]
2. Kegeles SS. Some motives for seeking preventive dental care. J Am Dent Assoc 1963;67:90-98. [ Links ]
3. Scott DS, Hirschman R. Psychological aspects of dental anxiety in adults. J Am Dent Assoc 1982;104:27-31. [ Links ]
4. Gatchel RJ, Ingersoll BD, Bowman L, Robertson MC,. Walter C. The prevalence of dental fear and avoidance: a recent survey study. J Am Dent Assoc 1983;107:609-610. [ Links ]
5. Peretz B, Moshonov J. Dental anxiety among patients undergoing endodontic treatment. J Endod 1998;24:435-437. [ Links ]
6. Claffey E, Reader A, Nusstein J, Beck M, Weaver J. Anesthetic efficacy of articaine for inferior alveolar nerve blocks in patient with irreversible pulpitis. J Endod 2004;30:568-571. [ Links ]
7. Rosa AL, Ferreira CM. Ansiedade odontologica: nivel de ansiedade, prevalencia e comportamento dos individuos ansiosos. Rev Bras Odont 1997;54:171-174. [ Links ]
8. Weine FS. Endodontic Therapy. 5th ed. Saint Louis: Mosby; 1989. [ Links ]
9. Saxen MA, Newton CW. Anesthesia for endodontic practice. Dent Clin North Am 1999;43:247-261. [ Links ]
10. Tortamano N, Soares MS. Alopatia. Prevencao e controle da dor usando os medicamentos genericos na Clinica Odontologica. In: Feller C, Gorab R. Atualizacao na Clinica Odontologica. 2nd vol. Sao Paulo: Artes Medicas 2000. p. 525-554 [ Links ]
11. Andrade ED, Ranali J, Volpato MC. Mecanismo de acao dos anestesicos locais. In: Endodontia. Biologia e tecnica. 2nd ed. Rio de Janeiro: Guanabara Koogan 2004. p. 174. [ Links ]
12. Cohen HP, Cha BY, Spangberg LS. Endodontic anesthesia in mandibular molars: a clinical study. J Endod 1993; 19:370-373. [ Links ]
13. Roberts DH, Sowray JH. Analgesia local em Odontologia. 3rd ed. Sao Paulo: Ed. Santos; 1995. [ Links ]
14. Fernandez C, Beck M, Nusstein J. A prospective, randomized, double-blind comparison of bupivacaine and lidocaine for inferior alveolar nerve blocks. J Endod 2005;31:499-503. [ Links ]
15. Kanaa MD, Meechan JG, Corbett IP, Whitworth JM. Speed in injection influences efficacy of inferior alveolar nerveblocks: a double-blind randomized controlled trial in volunteers. J Endod 2006;32:919-923. [ Links ]
16. Wallace AJ, Michanowicz AE, Mundell RD, Wilson EG. A pilot study of clinical problem of regionally anesthetising the pulp of an acutely inflamed mandibular molar. Oral Surg Oral Med Oral Pathol 1985;59:517-521. [ Links ]
17. Beer R, Baumann MA, Kim S. Color Atlas of Dental Medicine. Endodontology. Sttutgart: Thieme; 2000. p. 310. [ Links ]
18. Kaufman E, Weinstein P, Milgrom P. Difficulties in achieving local anesthesia. J Am Dent Assoc 1984;108:205-208. [ Links ]
19. Walton RE, Torabinejad M. Managing local anesthesia problems in the endodontic patient. J Am Dent Assoc 1992; 123:97-102. [ Links ]
20. Ayoub ST, Coleman AE. A review of local anesthetics. Gen Dent 2003;40:285-7,289-290. [ Links ]
21. Melo LL, Sidney RB, Sydney GB. Articaina – uma nova opcao em anesthesia odontologica. JBE 2000;1:79-87.
22. Mikesell P, Nusstein J, Reader A, Beck M, Weaver J. A comparison of articaine and lidocaine for inferior alveolar nerve blocks. J Endod 2005;31:265-270. [ Links ]
23. Hinkley SA, Reader A, Bech M, Meyers WJ. An evaluation of 4% prilocaine with 1:200.000 epinephrine and 2% mepivacaine with 1:20.000 levonordefrin compared with 2% lidocaine with 1:100.000 epinephrine for inferior alveolar nerve block. Anesth Prog 1991;38:84-89. [ Links ]
24. Maniglia-Ferreira C, Gurgel Filho ED, Moura EH, Valverde GB, De Deus G, Coutinho Filho T. Avaliacao clinica do uso de dois sais anestesicos em endodontia. Stoma 2002;14:34-38. [ Links ]
25. Potocnik I, Bajrovic F. Failure of inferior alveolar nerve block in endodontics. Endod Dent Traumatol 1999;15:247-251. [ Links ]
26. Malamed SF, Gagnon S, Leblanc D. Articaine hydrochloride: a study of the safety of a new amide local anesthetic. J Am Dent Assoc 2001;132:177-185. [ Links ]
27. Bigby J, Reader A, Nusstein J, Beck M, Weaver J. Articaine for supplemental intraosseous anesthesia in patients with irreversible pulpitis. J Endod 2006;32:1044-1047. [ Links ]
28. Malamed SF. Medical emergencies in the dental office. 4th ed. St. Louis: Mosby; 1993. [ Links ]
29. Mees ML, Portela IC, Carlini JL. Uso dos anestesicos locais em Odontologia. Rev Bras Odont 1997;54:273-276. [ Links ]
30. Maniglia-Ferreira C, Gurgel Filho ED. Urgencias em Endodontia. In: Figueiredo IMB, Aguiar ASW. Situacoes emergenciais no consultorio odontologico. 1st ed. Sao Paulo: Editora Santos; 2007. Chap. 4. [ Links ]














