Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Acta Odontológica Latinoamericana
versión On-line ISSN 1852-4834
Acta odontol. latinoam. vol.22 no.3 Buenos Aires dic. 2009
ARTÍCULOS ORIGINALES
A comparison of the film thickness of two adhesive luting agents and the effect of thermocycling on their μTBS to feldspathic ceramic
Priscilla C. Pereira1, Anderson A. Castilho1, Rodrigo O. A. Souza2, Sheila P. Passos1, Fernando E. Takahashi1, Marco A. Bottino1
1São José dos Campos Dental School, São Paulo State University, São José dos Campos, Brazil
2Federal University of Paraíba (UFPB), Department of Restorative Dentistry, Division of Prosthodontics, João Pessoa, Brazil.
CORRESPONDENCE Dr. Rodrigo O. A. Souza Federal University of Paraiba Department of Restorative Dentistry Rua Praia de Guajiru, 9215 Ponta Negra, Natal/RN Brazil, Zip Code: 59.092-220 e-mail: roasouza@yahoo.com.br
ABSTRACT
The aim of the present study was to evaluate the effect of thermocycling (TC) on the microtensile bond strength (μTBS) of two luting agents to feldspathic ceramic and to measure their film thickness (FT). For the μTBS test, sixteen blocks (6.4 x 6.4 x 4.8 mm) were fabricated using a feldspathic ceramic, etched with 10% hydrofluoric acid, rinsed and treated with the silane agent. The ceramic blocks were divided into two groups (n= 8): Gr1: dual-cured resin cement and Gr2: flowable resin. The luting agents were applied on the treated surfaces. Microsticks (1 ± 0.1mm2) were prepared and stored under two conditions: dry, specimens immediately submitted to the μTBS test, and TC (6,000 cycles; 5°C-55°C). The μTBS was evaluated using a universal testing machine (1 mm/min). The μTBS data (MPa) were submitted to two-way ANOVA and Tukey’s test (5%). For the FT test (ISO 4049), 0.05 ml of each luting agent (n=8) was pressed between two Mylar-covered glass plates (150 N) for 180 seconds and light polymerized. FT was measured using a digital paquimeter (Model 727-2001). The data (mm) were submitted to one-way ANOVA. The luting cement did not influence the μTBS results (p=0.4467). Higher microtensile bond values were found after TC (20.5 ± 8.6 MPa) compared to the dry condition (13.9 ± 4.7 MPa), for both luting agents. The luting agents presented similar film thicknesses: Gr1- 0.052 ± 0.016 mm; Gr2- 0.041 ± 0.003 mm. The luting agents presented similar film thickness and μTBS values, in dry and TC conditions and TC increased the bond strength regardless of the luting agent.
Key words: Adhesion; Surface treatment; Thermocycling; Film thickness; Luting agents; Ceramic.
RESUMO
Comparacao da espessura da pelicula de dois agentes cimentantes e o efeito da ciclagem termica na resistencia de uniao a microtracao a uma ceramica feldspatica
Avaliar o efeito da termociclagem (TC) na resistencia de uniao a microtracao (μTBS) de dois agentes cimentantes a uma ceramica feldspatica e mensurar a espessura da pelicula (FT) desses agentes cimentantes. Para o ensaio de μTBS, dezesseis blocos (6,4 x 6,4 x 4,8 mm) foram fabricados utilizando uma ceramica feldspatica, condicionados com acido fluoridrico 10%, lavados, secos e aplicado o agente silano na superficie.Os blocos ceramicos foram divididos em dois grupos (n=8): Gr1: cimento resinoso de polimerizacao dual e Gr2: resina flow. Os dois agentes cimentantes foram entao aplicados sobre as superficies tratadas. Os palitos (1 ± 0.1mm2) foram confeccionados e divididos de acordo com duas condicoes de armazenagem: seco, as amostras foram imediatamente submetidas ao teste de μTBS, e TC (6.000 ciclos; 5°C-55°C). The μTBS was evaluated using a universal testing machine (1 mm/min). Os dados de μTBS (MPa) foram submetidos a Analise de Variancia (ANOVA) dois fatores e ao teste de Tukey (5%). Para o teste FT (ISO 4049), 0,05 ml de cada agente cimentante (n=8) foi prensado entre duas placas de vcidro (Mylar) (15kg) durante 180 segundos, fotopolimerizadas e a FT foi mensurada utilizando um paquimetro digital (Modelo 727-2001). Os dados (mm) foram submetidos a Analise de Variancia (ANOVA) um fator. O agente cimentante nao influenciou os resultados de resistencia de uniao a microtracao (p=0,4467). Os maiores valores de resistencia de uniao for a encontrados apos a TC (20,5±8,6 MPa) comparado com a condicao sem TC (13,9±4,7 MPa), para ambos os agentes cimentantes. Os agentes cimentantes apresentaram espessuras de pelicula similares: Gr1- 0,052±0,016 mm; Gr2- 0,041±0,003 mm). Os agentes cimentantes apresentaram espessura de pelicula e valores de μTBS, em condicao com e sem TC, e que a TC aumentou a resistencia de uniao, independente do agente cimentante utilizado.
Palavras chave: Adesao; Tratamento de superficie; Termociclagem; Espessura da pelicula; Agente cimentante; Ceramica.
INTRODUCTION
All-ceramic restorations have been used for a long time, mainly due to their excellent esthetic appearance and the excellent mechanical strength of the ceramic systems. However, many factors can affect the longevity of ceramic restorations; such as the type of ceramic1, surface treatment2,3, luting agent, quality and amount of the remaining dental tissue4, adhesive system, thermocycling5,6 and mechanical cycling. The main failure found in this type of restoring treatment was debonding. The attachment of ceramic materials to dental tissue is obtained by a chemical and/or mechanical union of these structures to the luting agents and is considered an important factor for the clinical success of these restorations. Depending on the microstructure of the ceramic material used, bonding of these restorations can be done using the adhesive technique associated with diverse surface treatments7,8. However, glass ceramics (feldspathic, fluorapatite and lithium dissilicate) have been widely used for producing partial veneer crowns (inlay, onlay, overlay and veneers) and complete crowns, either using the stratification, pressed, or CAD/CAM techniques9,10. The surface treatment of glass ceramic for adhesive bonding is well established in the literature. Hydrofluoric acid is used to attack the glass phase, producing a retentive surface for micromechanical bonding, maximizing the bond strength between etched ceramic and resin cements. The etched ceramic surface must be coated with a suitable silane1,7,12, which promotes the chemical bond between the silica of the ceramic and the methacrylate groups of the resin luting cements13,14. This process also promotes the wettability of the ceramic surface, enhancing the contact with resin cements15.
Flowable composites have been available for a relatively short time, yet many possible uses have been recommended by the manufacturers. However, there has been limited testing in laboratory or clinical settings of the efficacy of these suggested uses. These composites have lower viscosity, increased wettability, and when polymerized, have increased elasticity when compared to traditional composite resins17. They are often used in direct resin restorations18 19, adhesive restorations associated with fibers20, marginal repair and sealants21. Additionally, flowable composites have been proposed for luting ceramic restorations as inlays and veneers in a few studies11; this material also has a variety of shades and a lower price than resin cements, which represents an advantage in clinical practice. However, the bond strength durability of the flowable resin/ceramic interface is not well established. Considering that the bond strength test has crucial importance when evaluating the behavior and longevity of the resin/ceramic interface, the aim of the current study was to evaluate the film thickness and bond durability of two luting agents (resin cement and flowable resin) to a feldspathic ceramic. The null hypotheses were that (1) the microtensile bond strength is not influenced by the thermocycling and (2) the different luting cements do not have different film thicknesses.
MATERIALS AND METHODS
The brand names, material types, main compositions, manufacturers and batch numbers of the products used in the current study are presented in Table 1.
Table 1: Brand names, material types, main components, manufacturers and batch numbers of the products used for the experiments.
With the assistance of a silicon mold, sixteen blocks (6.4 x 6.4 x 4.8 mm) of feldspathic ceramic (VITA VM7, Dentin 2M1, VITA Zanhfabrik) were produced, according to the manufacturer’s instructions. The cementation surface of each ceramic block was leveled and polished in a machine using silicone carbide papers in sequence (600, 800 and 1200 grit) under water cooling (3M ESPE, St. Paul, USA). Impressions were made from each ceramic block after polishing using addition silicone putty (Elite HD, Zhermach, Badia Polesine, Italia, Batch#: 18443). The block was pushed into the silicone to leave 3 mm between the upper portion of the mold and the surface of the block. Thereafter, the cement was injected into this space (thickness: 3 mm) (Figures 1a-b).
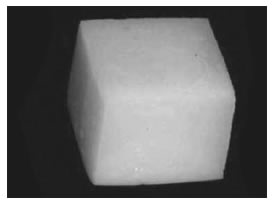
Fig. 1a: Ceramic block after polishing.
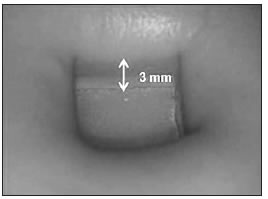
Fig. 1b: Ceramic block positioned inside the silicon mold prior to insertion of the luting agent.
Prior to surface conditioning, all blocks were ultrasonically cleaned (Vitasonic, Vita Zanhfabrik, Germany) for 5 minutes using distilled water. The ceramic surfaces were etched with 10% HF acid gel (Dentsply, Petropolis, Brazil) for 60 seconds, rinsed with air-water spray for 60 seconds and air-dried. The ceramics were ultrasonically cleaned in distilled water for 5 minutes. The silane coupling agent was then applied (Monobond-S; Ivoclar Vivadent) with a clean brush in one layer and allowed to sit for 5 minutes. The ceramic blocks were then randomly divided into two groups (n=8) according to the luting agent to be used: Gr1- Variolink II (Ivoclar-Vivadent) and Gr2- Filtek Z350 Flow (3M ESPE). Each block was placed in its silicone mold with the treated surface exposed. The luting agents were bonded to the ceramic surface, following the manufacturer’s instructions, and injected into the mold on the treated surface of the ceramic block, using a centrix syringe (DFL, Rio de Janeiro, Brazil). The cement in the mold was light-activated (XL 3000, 3M ESPE, MN, USA; light output: 500 mW/cm2) for 40 seconds on the upper side of the specimen (incremental technique: 1.5 mm of thickness from each increment). The intensity of the light was verified to be no lower than 500 mW/cm2 using a radiometer (Demetron LC, Kerr) before starting light polymerization in each group. After 10 minutes, the ceramic block-resin cement assembly was removed from the mold and the cement was submitted to light polymerization from the five aspects of the block (upper and laterals) for 40 seconds per side.
Specimen Preparation for the Microtensile Bond Strength Test (μTBS)
Ceramic-cement blocks were sectioned using a diamond disc (Microdont, Sao Paulo, Brazil, no. 34570) at low-speed, under water cooling, in a sectioning machine (LabCut 1010, Extec, Enfield, CT, USA). Initially, the cemented blocks were attached to a metallic base that was attached to the sectioning machine using cyanoacrylate adhesive gel (Super Bonder Gel, Loctite Ltd, Sao Paulo, Brazil). The blocks were positioned as perpendicularly as possible in relation to the diamond disc of the machine. The first section, measuring approximately 1 mm, was discarded due to the possibility of an excess or absence of cement at the interface that might alter the results. Thereafter, three sections measuring 1.0 ± 0.1 mm in thickness were prepared. Each section was rotated 90° and once again attached to the metallic base. The first microstick was discarded (1 ± 0.1 mm) due to the aforementioned reasons. Subsequently, four additional microsticks were prepared, also measuring 1.0 ± 0.1 mm in thickness. This process was followed for the other two sections; therefore, only the central microsticks were used for the experiments22. About ten specimens were obtained from each block. The beam specimens had non-machined (non-trimmed) bonding areas with a bonded area measuring approximately 1.0 ± 0.1 mm2 and a length of 8 mm. The 10 specimens obtained from each ceramic block were randomly divided into 2 testing conditions. In the dry condition (Dry), specimens were immediately submitted to microtensile testing after sectioning. In the aged condition (TC), specimens were submitted to thermal cycling (6,000 cycles; 5°C-55°C, dwelling time: 30 s, transfer time: 2 s) (Nova Etica, Sao Paulo, Brazil) and then submitted to testing. Thus, 4 groups were obtained, considering the “luting agent” (2 levels) and “thermocycling” (2 levels).
Microtensile Bond Strength Test (μTBST)
Each specimen was attached with cyanoacrylate gel (Super Bonder Gel, Loctite Ltd, Sao Paulo, Brazil) to the rods of a device adapted for this test, keeping the adhesive zone free. The specimens were positioned parallel to the long axis of the device, in order to reduce the bending stresses. The device was used in a universal testing machine (EMIC DL- 1000, EMIC, Sao Jose dos Pinhais, Brazil) and testing was performed at a cross-head speed of 1 mm/min22 (Figures 2a-c). The bond strength was calculated using the formula: R=F/A, where “R” is the strength (MPa), “F” is the load required for rupture of the specimen (N) and “A” is the interface area of the specimen (mm2), measured with a digital caliper before the test.
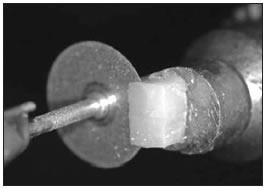
Fig. 2a: Luting agent applied on ceramic block and attached to the metal base for producing the sections.
Fig. 2b: Production of microsticks from the sections.
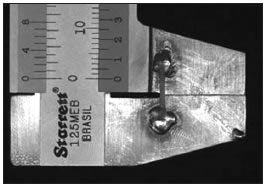
Fig. 2c: Sample positioned on the paquimeter prior to the μTBST.
Fracture analysis
The specimens were analyzed under a stereomicroscope (Stemi 2000-C, Carl Zeiss, Gottingen, Germany) at a magnification of 30x, and the image was digitally recorded with a camera (Cybershot, Model DSC S85, Sony, Tokyo, Japan) connected to the microscope to characterize the ceramic surfaces and the failure modes. The failure types were classified according to the following criteria: A) adhesive fracture along the interfacial region between the luting agent and ceramic, B) cohesive fracture along the luting agent C) cohesive fracture along the ceramic and D) mixed fracture (adhesive failure between the luting agent and ceramic coupled to cohesive fracture of the luting agent).
Film Thickness Sample fabrication and thickness measurement
According to ISO Specification No. 4049 23, 0.05 ml of each luting agent (n=8) was extruded from 1.0- ml tuberculine syringes onto a Mylar sheet (Type D, 0.08 inch; DuPont, Wilmington, Del) and placed on the surface of a 3/4-inch-thick polished glass slab. Another piece of Mylar was placed on top of this composite resin, and a similar glass slab was placed on top. Immediately, a vertical load of 150 N was applied to the top glass plate for a period of 180 seconds in a Universal Testing-machine (EMIC DL-1000, EMIC, Sao Jose dos Pinhais, Brazil). The top glass plate was then removed and the composite resin specimen was light polymerized (XL 3000, 3M ESPE, MN, USA; light output: 500 mW/cm2) for 40 seconds at 500 mw/cm2 through the Mylar strip to provide a solid disc for thickness measurement. The film thickness was measured with a digital paquimeter (Model 727-2001), precise to 0.1 mm. Three individual thickness measurements were made for each polymerized specimen and the mean was obtained from these values.
Statistical analysis
Statistical analysis of the film thickness was performed using one-way ANOVA. For the microtensile bond strength test, two-way ANOVA was used and multiple comparisons were made with Tukey`s adjustment test, considering the luting agent and thermocycling. P values less than 0.05 were considered to be statistically significant in all tests.
RESULTS
Two-way ANOVA revealed that the microtensile bond strength was significantly affected by thermocycling (p=0.0001<0.05) (Table 2). The luting agents presented similar μTBS values in the dry (Gr1: 15.0 ± 4.3 MPa; Gr2: 13.1 ± 5.5 MPa) and aged conditions (Gr1: 21.2 ± 9.3 MPa; Gr2: 20.7 ± 7.2 MPa). However, when the dry and TC conditions were compared for each luting agent, the TC condition presented μTBS values that were significantly higher than in the dry condition, regardless of the luting agent (Table 3). All groups presented premature debonding during specimen preparation, but the flowable resin presented a higher incidence than the resin cement (Table 4). The film thickness did not differ between the luting agents (p=0.1203>0.05): Gr1- 0.041 ± 0.003 mm and Gr2- 0.052 ± 0.016 mm (Figure 3).
Table 2: Results of 2-way analysis of variance for thermocycling, luting agent and the interaction terms for μTBS data (*p<0.05).
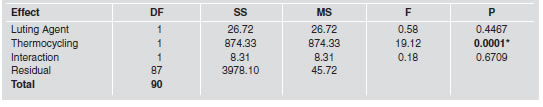
Table 3: Mean (±SD) of μTBST values (MPa) for luting agent/ceramic combinations with and without thermo cycling conditions. *The same superscript letters indicate no significant differences (Tukey’s test, α=0.05).
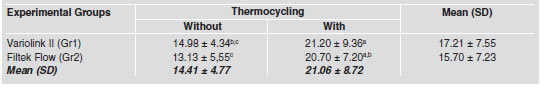
Table 4: Number (No) of specimens (sp) produced, and percentage (%) of pre-test failures (PTF) during cutting and thermocycling (TC) and total number of sp prior to μTBST.
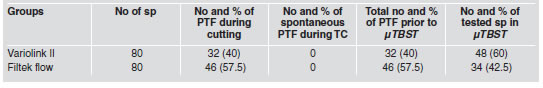
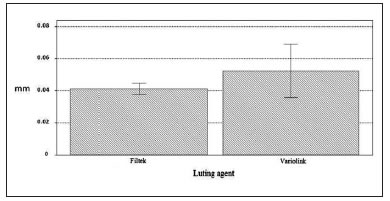
Fig. 3: Graphic representation (mean and SD) of film thickness results for the different luting agents tested.
The fracture analysis of the specimens revealed different fracture patterns: adhesive failure along the interfacial region between the luting agent and the feldspathic ceramic (Score A); cohesive fracture in the ceramic (Score B); cohesive fracture in the luting agent (Score C) and mixed failure (cohesive fracture of the luting agent combined with the adhesive failure) (Score D), with and without thermocycling. The percentages of the types of fractures are presented in Table 5 and a representative micrograph of a mixed fracture is presented in Figure 4. The pattern of failure was very similar in all groups and the failures were predominantly mixed (Score D). The null hypotheses were partially accepted.
Table 5: Incidence of failure types (%) after the μTBST. A: Adhesive failure along the interfacial region between the luting agent and the feldspathic ceramic; B: cohesive fracture in the feldspathic ceramic, C: cohesive fracture in the luting cement and D: mixed failure (cohesive fracture of the cement combined with the adhesive failure).
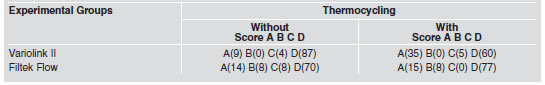
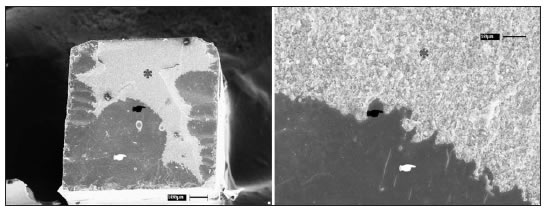
Fig. 4: Representative micrographs of a mixture fracture (Score D) between ceramic and cement layer of a specimen from group 2: a- 75x and b- x200. Asterisk * = resin cement; ☛ = rupture of the ceramic-resin cement interface; ☛ = ceramic.
DISCUSSION
Several in vitro methods for measuring the resinceramic bond strength have been described, including many microtensile24,25 and shear bond strength tests26. Della Bona et al.27 found that the shear bond strength test created arch-shaped cohesive fractures in all samples. These failures occur because of the highly non-uniform tension distribution on the interface of the materials. Therefore, the microtensile bond strength test is considered appropriate for in vitro assessment of resin composites bonded to ceramic, as failure occurs at the adhesive interface and not in the substrate13. For this reason, this test was chosen for the current study. This laboratory study was designed to investigate the influence of a dual-cure luting agent (Variolink II) and flowable composite resin (Filtek Z350 Flow) on the microtensile bond strength to feldspathic ceramic (VITA VM7). The bond strength was similar between the cements (mean range: 13.13 to 21.20 MPa), in dry and aged conditions. Similar results were found by Zohairy et al.25, who observed that there were no significant differences in microtensile bond strength between a flowable resin (Tetric Flow) and resin cements (Nexus 2 and Rely X) when bonded to a ceramic or resin CAD/CAM block.
When the silica-based ceramic is etched with hydrofluoric acid (5-10%), the glassy matrix of the ceramic is dissolved from the surface to a depth of a few microns. This treatment changes significantly the surface morphology, where the pores created on the surface are the most important descriptive pattern for the ceramic treated with hydrofluoric acid. This increase of the surface area favors the infiltration and retention of adhesive materials and makes the ceramic surface more retentive1,8. Saracoglu et al.40 evaluated the influence of different etching protocols on a silica based ceramic and their effect on the bond strength to resin cement. The scanning electron microscopy evaluation revealed that the hydrofluoric acid (5-10%) produced pores as the most important descriptive pattern for this treatment, whereas the orthophosphoric acid (40%) did not change the ceramic surface morphology. Furthermore, the hydrofluoric acid treatment increased the shear bond strength between ceramic and resin cement. Another important aspect of resin bond to silicabased ceramics is the application of a silane coupling agent. The silane agent is a bifunctional molecule that promotes the chemical bonding with organic surfaces such as resin materials and polymers and inorganic surfaces, such as silica-based ceramics41. This agent reacts with the silica oxide present in feldspathic ceramics or with oxides artificially deposited on alumina and zirconia based ceramics, creating a favorable bonding2,42. On the other hand, the silane agent increases the wettability of the luting agents on the ceramic surface, optimizing the bond strength results. Thus, hydrofluoric acid conditioning followed by the application of the silane agent on the ceramic promote conditions that favor the chemical bonding between the ceramic and flowable resin.
Barceleiro et al.28 analyzed the shear bond strength of feldspathic ceramic to bovine enamel luted with dual-cured resin cement and light-cured flowable composite. They verified that both luting agents presented similar results and that flowable composites are a suitable alternative when used for porcelain laminate veneer bonding, since these veneers are generally slim (less than 2 mm) and light polymerized luting agents can be light cured, providing satisfactory bond strength to these substrates29,30. Other authors also agree with the statement that a flowable composite can be used to lute indirect composite31 and ceramic restorations30, since this material has excellent characteristics, such as sufficient wear resistance17, greater fluidity and approximately 80% of the flexural strength of regular composites32, viscoelasticity33 and thin film thickness21. Thermocycling is a method frequently used for simulating intra-oral aging, combining hydrolytic and thermal degradation. In this study, half of the specimens from each group were subjected to 6,000 thermal cycles. The results revealed that thermocycling increased the μTBS for both luting agents. Although the cycle number used in this study was above the recommended number of cycles by ISO Specification No 1047734 (500 cycles), one limitation of this study could still be the short-term water storage and reduced thermal cycling in comparison to other studies, making it difficult to predict the long-term durability of the tested bonding methods2,22,24. Generally, thermocycling influences the bond strength results. The bond durability between the ceramic surface and the resin luting agent decreases with water storage and thermocycling2. During thermocycling, the soluble components of the resinous materials are removed and the water is absorbed to replace them. Additionally, water causes hydrolysis of the interface matrix and can cause fissures in the polymer matrix, both of which contribute to the reduction of resin properties35,36. This fact may also be responsible for the degree of degradation of the bond strength between the ceramic-resin interface during water storage, and this degradation is proportional to the time of storage37,38. However, the results of the current study showed that the μTBS was significantly higher for all luting agents after thermocycling (Gr1: from 14.98 ± 4.34 MPa to 21.20 ± 9.36 MPa; Gr2: from 13.13 ± 5.55 MPa to 20.70 ± 7.20 MPa). These results can be explained by the short-term water storage associated with the temperature of thermocycling (550C), which increased the degree of conversion for the luting agents, improving the bond strength of these materials to ceramic39. Pre-testing failures were experienced in this study (Table 4), similarly to other micro-tensile bond strength studies that showed debonding during the cutting procedure to make the microbars3,13,25, but in contrast to the study of Peumans et al.6. The analysis of the fractured surfaces by light microscopy and SEM showed that most of the failures were mixed (Figs 4a-b), similarly to the studies of El Zohairy et al.25 and Meyer Filho et al.3, who also evaluated the bond between glass ceramics and resin cement (Table 5). The film thickness analysis showed that Filtek Z350 Flow (0.041 ± 0.003 mm) was similar to the resin cement, Variolink (0.052 ± 0.016 mm). This property is related with the percentage of inorganic filler of the materials. According to the manufacturers of these composites, they have a similar quantity of inorganic fillers: Filtek flow (55% vol.) and Variolink II (43.6% vol.), making them of similar viscosity. The film thickness revealed that the standard-deviation of flowable resin composite was smaller than for the resin cement. This can be explained by the single component of the flowable resin composite. Resin cements are composed of base and catalyst pastes, which have different compositions and might not be mixed exactly in the same amount. Similar studies21,32,43 observed thickness values ranging from 0.003 to 0.06 for different flowable composites and resin cements, which makes a flowable resin similar to the resin composite in terms of the marginal discrepancy of indirect restorations luted with these materials.
Finally, the findings of the current study seem to have an important clinical relevance for adhesive luting of indirect restorations. Thus, the use of a flowable resin to lute indirect ceramic or resin restorations can yield similar results when compared to the resin cement25,28. However, this would occur only in those cases where the restorations have a thickness of less than 2 mm since the flowable resin needs a good intensity of light to provide satisfactory bond strength to the enamel/dentin/ ceramic substrates29,30 and acceptable film thickness21,32,43. So, according to the literature and to the findings of this study, the flowable resin is indicated for luting glass ceramic restorations and indirect resin restoration as veneer and inlay. Further long-term in vitro and prospective clinical studies using mechanical fatigue tests must be conducted for confirmation of the clinical argument.
CONCLUSION
Based on the results, thermocycling increased the bond strength between ceramic-resin regardless of the luting agent. The flowable composite resin and the resin cement have similar film thicknesses.
1. Spohr AM, Sobrinho LC, Consani S, et al. Influence of surface conditions and silane agent on the bond of resin to IPS Empress 2 ceramic. Int J Prosthodont 2003;16:277-282. [ Links ]
2. Ozcan M, Vallittu PK. Effect of surface conditioning methods on the bond strength of luting cement to ceramics. Dent Mater 2003;19:725-731. [ Links ]
3. Meyer Filho JA, Viera LCC, Araujo E, Monteiro Junior S. Effect of different ceramic surface treatments on resin microtensile bond strength. Int J Prosthodont 2004;13: 28-35. [ Links ]
4. Hayashi M, Tsuchitani Y, Kawamura Y, Miura M, Takeshige F, Ebisu S. Eight-year clinical evaluation of fired ceramic inlays. Oper Dent 2000;25:473-481. [ Links ]
5. Andreatta Filho OD, Galhano G, Bottino MA, Camargo FP, Valandro LF, Nishioka RS. Avaliacao da resistencia adesiva entre uma ceramica aluminizada e um cimento resinoso submetidos a ciclagem termica. Cienc Odontol Bras 2003 jul./set.;6:32-39. [ Links ]
6. Peumans M, Hikita K, Munck J, Van Landuyt K, Poitevin A, Lambrechts P, Van Meerbeek B. Effects of ceramic surface treatments on the bond strength of an adhesive luting agent to CAD-CAM ceramic. J Dent 2007;35:282-288. [ Links ]
7. Roulet JF, Soderholm KJ, Longmate J. Effects of treatment and storage conditions on ceramic/composite bond strength. J Dent Res 1995;74:381-7. [ Links ]
8. Brentel A, Ozcan M, Valandro LF, Alarca LG, Amaral R, Bottino MA. Microtensile bond strength of a resin cement to feldspathic ceramic after different etching and silanization regimens in dry and aged conditions. Dent Mater 2007;23:1323-1331. [ Links ]
9. Chang JC, Hart DA, Estey AW, Tensile bond strengths of five luting agents to two CAD-CAM restorative materials and enamel. J Prosthet Dent 2003;90:18-23. [ Links ]
10. Liu P, Isenberg BP, Leinfelder KF. Evaluating CAD-CAM generated ceramic veneers. J Am Dent Assoc 1993;124:59-63. [ Links ]
11. Peumans M, Van Meerbeek B, Lambrechts P, Vanherle G. Porcelain veneers: a review of the literature. J Dent 2000;28:163-77. [ Links ]
12. Aida M, Hayakawa T, Mizukawa K. Adhesion of composite to porcelain with various surface conditions. J Prosthet Dent 1995;73:464-470. [ Links ]
13. Della Bona A, Anusavice KJ, Shen C. Microtensile strength of composite bonded to hot-pressed ceramics. J Adhes Dent 2000;2:305-313. [ Links ]
14. Della Bona A, Shen C, Anusavice KJ. Work of adhesion of resin on treated lithia disilicate-based ceramic. Dent Mater 2004;20:338-344. [ Links ]
15. Matinlinna JP, Lassila LVJ, Ozcan M, Antti Y, Vallittu PK. An introduction to silanes and their clinical applications in dentistry. Int J Prosthodont 2004;17:155-164. [ Links ]
16. Kern M, Thompson VP. Bonding to glass infiltrated alumina ceramic: adhesive methods and their durability. J Prosthet Dent 1995;73:240-249. [ Links ]
17. Bayne SC, Thompson JY, Swift EJ Jr, Stamatiades P, Wilkerson M, A characterization of first-generation flowable composites. J Am Dent Assoc 1998;129:567-577. [ Links ]
18. Erfes B, Dorter C, Gormec Y, Koray F. Two year clinical evaluation of ormocer and nanofill composite with and without a flowable liner. J Adhes Dent 2006;8:119-126. [ Links ]
19. Korkmaz Y, Ozel E, Attar N. Effect of flowable composite lining on microleakage and internal voids in class II composite restorations. J Adhes Dent 2007;9:189-194. [ Links ]
20. Belli S, Orucoglu H, Yildirim C, Gurcan E. The effect of fiber placement or a flowable resin lining on microleakage in class II adhesive restorations J Adhes Dent 2007; 9:185-181. [ Links ]
21. Moon PC, Tabassian MS, Culbreath TE. Flow characteristics and film thickness of flowable resin composites. Oper Dent 2002;27:248-253. [ Links ]
22. Foxton RM, Pereira PNR, Nakajima M, Junji T, Hiroyuki M. Durability of the dual-cure resin cement / ceramic bond with different curing strategies. J Adhes Dent 2002;4:49-59. [ Links ]
23. International Organization for Standardization. ISO 4049. Dentistry - polymer-based filling, restorative and luting materials; 2000. [ Links ]
24. Hooshmand T, van Noort R, Keshvad A. Bond durability of the resin-bonded and silane treated ceramic surface. Dent Mater 2002;18:179-188. [ Links ]
25. El Zohairy AA, De Gee AJ, Mohsen MM, Feilzer AJ. Microtensile bond strength testing of luting cements to prefabricated CAD/CAM ceramic and composite blocks. Dent Mater 2003;19:575-583. [ Links ]
26. Sorensen JA, Engelman MJ, Torres TJ, Avera SP. Shear bond strength of composite resin to porcelain. Int J Prosthodont 1991;4:17-23. [ Links ]
27. Della Bona A, van Noort R. Shear vs. tensile bond strength of resin composite bonded to ceramic. J Dent Res 1995; 74(9):1591-1596. [ Links ]
28. Barceleiro M de O, De Miranda MS, Dias KR, Sekito T Jr. Shear bond strength of porcelain laminate veneer bonded with flowable composite. Oper Dent, 2003;28(4):423-428. [ Links ]
29. Akgungor G, Akkayan B, Gaucher H. Influence of ceramic thickness and polymerization mode of a resin luting agent on early bond strength and durability with a lithium dissilicate–based ceramic system. J Prosthet Dent 2005; 94:234-241.
30. Bitter K, Paris S, Hartwig C, Neumann K, Kielbassa AM. Shear Bond strength of different substrates bonded to lithium dissilicate ceramics. Dent Mat J 2006;23(3):493-502. [ Links ]
31. Okuda M, Nikaido T, Maruoka R, Foxton RM, Junji T. Microtensile bond strengths to cavity floor dentin in indirect composite restorations using resin coating. J Esthet Restor Dent 2007;19(1):38-46; discussion 47-8. [ Links ]
32. Attar N, Tam L, McCom D. Flow, strength, stiffness and radiopacity of flowable resin composites. J Can Dent Assoc 2003;69(8):516-521. [ Links ]
33. Lee IB, Son HH, Um CM. Rheologic properties of flowable, conventional hybrid, and condensable composite resins. Dent Mater 2003 Jun;19(4):298-307. [ Links ]
34. International Organization for Standardization. ISO 10477 Polymer-based, Crown and Bridge Materials, Amendment 1; 1998. [ Links ]
35. Ferracane JL, Hopkin JK, Condon JR. Properties of heattreated composites after aging in water. Dent Mater 1995; 11:354-358. [ Links ]
36. Umemoto K, Kurata S. Effects of mixed silane coupling agent on porcelain tooth material and various dental alloys. Dent Mater 1995;14:135-142. [ Links ]
37. Drummond JL, Novickas D, Lenke JW. Physiological aging of an all-ceramic restorative material. Dent Mater 1991; 7:133-137. [ Links ]
38. Ortengren U, Wellendorf H, Karlsson S, Ruyter IE. Water sorption and solubility of dental composites and identification of monomers released in an aqueous environment. J Oral Rehabil 2001;28:1106-1115. [ Links ]
39. Ferracane JL, Berge HX, Condon JR. In vitro aging of dental composites in water-effect of degree of conversion, filler volume, and filler/matrix coupling. J Biomed Mater Res 1998;42:465-472. [ Links ]
40. Saracoglu A, Cura C, Cotert HS. Effect of various surface treatment methods on the bond strength of the heat-pressed ceramic samples. J Oral Rehab 2004;31:790-797. [ Links ]
41. Jardel V, Degrange M, Picard B, Derrien G: Correlation of topography to bond strength of etched ceramic. Int J Prosthodont 1999;12:59-64. [ Links ]
42. Soderholm KJM, Shang SW. Molecular orientation of silane at the surface of colloidal silica. J Dent Res 1993; 72:1050-1054. [ Links ]
43. Blalock J, Holmes R, Rueggeberg F. Effect of temperature on unpolymerized composite resin film thickness. J Prosthet Dent 2006;96:424-432. [ Links ]














