Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Acta Odontológica Latinoamericana
versión On-line ISSN 1852-4834
Acta odontol. latinoam. vol.24 no.2 Buenos Aires set. 2011
ARTÍCULOS ORIGINALES
Susceptibility of candida albicans to photodynamic therapy using methylene blue and toluidine blue as photosensitizing dyes
Yasmine M. Pupo, Giovana M. Gomes, Elizabete B. Santos, Luzia Chaves, Milton D. Michel, Vitoldo A. Kozlowski Jr, Osnara M. M. Gomes, Joao Carlos Gomes
Dentistry School, State University of Ponta Grossa (UEPG), Ponta Grossa, Parana, Brazil
CORRESPONDENCE Yasmine Mendes Pupo Rua: Jaime Pinto Rosas, 180 – Jardim Carvalho 84015-600 Ponta Grossa, Paran., Brasil E-mail: yasminemendes@hotmail.com
ABSTRACT
The increased resistance of Candida albicans to antibiotic therapy indicates the need for alternative treatments for oral candidiasis. Photodynamic therapy (PDT) has been researched as an alternative tool to inactivate pathogenic microorganisms. It uses a combination of a photosensitizer and a visible light source. This study evaluated the susceptibility of C. albicans to PDT and compared the efficacy of 100 μg/mL methylene blue (MB) and toluidine blue (TB) as photosensitizers. The light source was Indium-Gallium-Aluminum Phosphide (InGaAlP) laser at 53 J/cm2. Suspensions of 108 cells/mL of C. albicans were subject to PDT for 5 minutes in 96-well plates, then decimal dilutions were plated on Sabouraud Dextrose agar. After 48h incubation at 37°C, the number of CFU/mL were obtained and submitted to statistical analysis using Kolmogorov- Smirnov, ANOVA (p<0.0001) and Tukey tests. The results showed that MB or laser irradiation alone did not have statistically significant antifungal activity compared to the positive control group (p>0.05). Conversely, the number of viable C. albicans cells was reduced significantly after PDT using MB or mainly TB associated to diode laser irradiation. The data proved the efficacy of PDT against C. albicans cells, regardless of the photosensitizer used.
Key words: Methylene blue; Photochemotherapy; Candida albicans.
RESUMO
Suscetibilidade da candida albicans a terapia fotodinâmica utilizando azul de metileno e azul de toluidina como fotossensibilizadores
O aumento da resistencia de Candida albicans a antibioticoterapia indica a necessidade de tratamentos alternativos para a candidiase oral. A terapia fotodinamica (PDT) tem sido investigado como uma ferramenta alternativa para inativacao de microrganismos patogenicos, em que uma combinacao de um fotossensibilizador e uma fonte de luz visivel e utilizada neste processo. Este estudo avaliou a suscetibilidade de C. albicans a PDT e comparou a eficacia do azul de metileno (MB) e azul de toluidina (TB), na concentracao de 100 mg/mL como fotossensibilizadores. A fonte de luz era indio-galio-aluminio Phosphide laser (InGaAlP) a 53 J/cm2. Suspensoes de 108 celulas/ mL de C. albicans foram submetidos ao PDT por 5 minutos em placas de 96 pocos, e diluicoes decimais foram semeadas em agar Sabouraud Dextrose. Apos 48h de incubacao a 37°C, o numero de UFC/mL foram obtidos e submetidos a analise estatistica usando Kolmogorov-Smirnov, ANOVA (p <0,0001) e teste de Tukey. Os resultados mostraram que separadamente, MB ou irradiacao do laser nao apresentaram atividade antifungica significativa, em comparacao ao grupo controle positivo (p> 0,05). Por outro lado, o numero de celulas viaveis de C. albicans reduziu significativamente apos PDT, utilizando MB ou principalmente TB associado a irradiacao do laser de diodo. Os dados demonstraram a eficacia da PDT em C. Albicans, independente do fotossensibilizador utilizado.
Palavras-chave: Azul de metileno; Fotoquimioterapia; Candida albicans.
INTRODUCTION
The increased resistance of Candida species to antibiotic therapy has been widely demonstrated and indicates the need for alternative treatment of candidiasis1-3. Susceptible patients, such as those with leukemia, immunosuppressed, corticosteroid users and HIV-infected patients4,5, or patients with other debilitating conditions may develop more severe, extensive and difficult to treat systemic and/or local infections. Photodynamic therapy (PDT) has been investigated as a potential antimicrobial therapy6,7 and an alternative tool against some infectious diseases8. The process combines light and a photosensitizing drug, promoting a phototoxic response of the treated cells, usually via oxidative damage6-8. The transfer of the energy from the reaction between the activated photosensitizer and the available oxygen results in the formation of toxic oxygen species and free radicals9. As most microbial species do not have endogenous photosensitive components, it is important to use a photosensitizer capable of attracting light and initiating the formation of free radicals10. The action of various photosensitizers, especially phenothiazine dyes, porphyrins and phthalocyanines, has been studied. The photosensitizing drug acts as an agent of optical absorption or chromophore, which produces fluorescence after irradiation, causing citotoxicity in the medium.
In vitro studies have shown the use of a laser associated to a photosensitizer is very efficient against bacteria, yeasts, viruses and parasites11-13. However, a great number of variables can influence the number of microorganisms affected by this technique, including the type and concentration of the photosensitizer, the physiological phase of the microorganism, the incubation period of the photosensitizer before the irradiation, the exposure period and laser output intensity10. The aim of this study was to evaluate C. albicans susceptibility to PDT and compare the efficacy of methylene blue (MB) and toluidine blue (TB) as photosensitizers.
METHODS
Preparation of the C. albicans suspension
A standard suspension of C. albicans (ATCC 10231) was prepared in 5 ml of sterile saline solution, from a 24-hour growth, and standardized using the 0.5 tube of the McFarland scale.
Photosensitizers and laser source
Methylene blue (MB) or toluidine blue (TB) were used as photosensitizers, at a concentration of 100 μg/mL. They were stored and manipulated in the absence of light. The irradiation was performed using an InGaAlP diode laser (Whitening Lase II, DMC, S.o Carlos, Brazil). This device emitted electromagnetic irradiation with 630 to 690nm wavelengths and maximum absorbance peak of 660nm, which is coincident with the dye absorbance range. The energy dose was set at 53 J/cm², an output intensity of 40mW and an irradiation time of 5 minutes. The area was 0.38 cm2, which corresponds to a single orifice of a sterile 96-orifice microdilution plate used in the experiment.
In vitro photosensitization
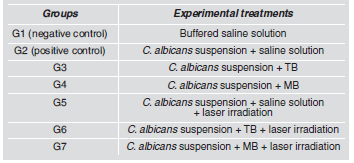
Table 1 shows the experimental groups. Each orifice of a 96-well plate was filled with 0.1 mL of C. albicans suspension and one of the photosensitizing agents MB or TB, and incubated at 37°C for 5 minutes. After incubation, laser irradiation was applied for 5 minutes. The tests were performed 5 times for each group. Serial dilutions up to 10-2 were obtained from each sample and aliquots of 0.1 mL were plated in duplicate on Sabouraud Dextrose Agar (ASD). After incubation at 37°C for 48 h, the number of colony-forming units (CFU/mL) was obtained and submitted to statistical analysis. Control groups received saline solution instead of MB or TB.
Table 1. Experimental treatments according to the groups.
Statistical analysis
Data were submitted to Kolmogorov Smirnov normality test. Means and standard deviations of CFU/mL were calculated in logarithm for the studied groups. Data were subjected to ANOVA and Tukey’s test (p<0.05). Percent reduction of each photosensitizer was calculated whether the diode laser was associated or not.
Scanning electron microscopy (SEM)
One specimen from each group was prepared for SEM observation (SSX-550, Shimadzu, Tokyo, Japan) after fixing with 2.5% glutaraldehyde for 10 minutes on a glass slide. The samples were dehydrated with colloidal silica, stored in a dry heat oven for 48 hours at 37°C, sputter coated and then examined under SEM (2400 X magnification). Each sample was qualitatively analyzed to establish the shape and integrity of the fungal cells.
RESULTS
Data analysis indicated the normality of the values (p>0.10). The groups which were irradiated in the presence of a photosensitizer agent (G6 and G7) had lower mean values for CFU/mL than the groups using only MB, TB or laser irradiation (Table 2).
Table 2. Mean values and standard deviations of colony forming units (CFU /mL) and logarithm (CFU/mL) recovered from five samples of each experimental group.
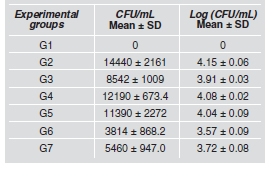
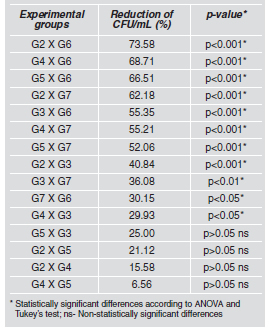
On the other hand, no difference was observed between groups G6 and G7 (p>0.05) where there was a 73.58% and 62.18% reduction in C. albicans cells, respectively compared to the control group (Table 3).
Table 3. Percent reduction of viable C. albicans cells exposed to different experimental conditions as compared between the groups and their respective significance levels.
Scanning electron microscopy was performed to visualize the effect of PDT on C. albicans cells compared to the controls. Roughness of cells surfaces was observed, mostly in G7, followed by G6. In group G7, parts of the cell walls seemed to have been removed. When TB and MB were used alone, no change was observed on the surface of the yeasts cells (Fig. 1).
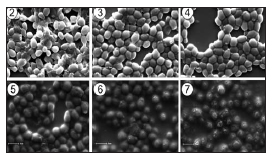
Fig. 1: SEM image of Candida albicans cells surfaces for each Tukey’s test; ns- Non-statistically significant differences experimental condition.
DISCUSSION
Studies have been reported on the use of PDT for elimination of fungi and bacteria from the oral cavity. Souza et al.14 used a red laser (685nm, 28 J/cm2) in the presence of MB (100 μg/mL) and found that the CFU/mL counts were reduced by 88.6% for C. albicans, 84.8% for C. dubliniensis, 91.6% for C. krusei and 82.3% for C. tropicalis. Light-activation of MB by the red laser had fungicidal effect on all the Candida species, but laser irradiation or methylene blue alone did not significantly reduce the number of CFU/mL of Candida samples, except for C. tropicalis. Our results showed a 62.18% reduction using methylene blue in the same concentration. It could be explained by differences in strain sensibility, exposition period, and laser irradiation. Giroldo et al.15 suggest that after irradiation, MB can lead to the production of cytotoxic singlet oxygen and other reactive oxygen species, which can damage the cell membrane and consequently promote cell death. In our study, the reduction of the CFU/mL of C. albicans using TB was greater than when methylene blue was used (p<0.05) (Tables 2 and 3). Our results support the findings of O’Neill et al.16, which observed a 97.4% reduction in the microorganisms found in dental biofilm when toluidine blue and He-Ne laser (632.8 nm) were applied. Sarkar et al.17 also observed a significant reduction of aerobic and anaerobic bacteria (lethal percent of 91.6% and 96.6%, respectively) found subgingivally, using toluidine blue (50 μg/mL) and He-Ne laser (7.3 mW for 30s).
The MB absorption spectrum ranges from 620 to 700 nm, with optimal penetration of the tissues and maximum absorption at 665 nm in aqueous solution18. It has been reported that the maximum absorption for TB was found to be 636 nm15. According to Teichert et al.19. MB is the ideal photosensitizer for antifungal therapy due to its low toxicity, wide acceptance for medical applications, and light-active antimicrobial potential. In our study, the photosensitization of MB and TB (100 μg/mL concentration) using laser irradiation (660 nm and 53 J/cm2) reduced C. albicans CFU/mL counts (62.18% and 73.58%, respectively) (Table 3). In contrast, Wilson and Mia10 reported a 42% reduction in C.albicans CFU/mL counts when methylene blue (100 μg/mL) and a 660 nm laser irradiation (2.04 J/cm2 energy dose) were used. These differences could probably be attributed to different parameters of the laser sources. Our findings support the studies of Carvalho et al.7 and Usacheva et al.20, which reported antimicrobial activity of the association between laser and a photosensitizer for PDT. Souza et al.15 suggest that the solubility of toluidine blue should be higher in the hydrophobic region of the membrane, thus, toluidine blue could interact more easily than methylene blue with the bacterial membrane. As a result, the concentration of toluidine blue within the microorganism cell should be significantly higher than that of methylene blue. However, in our study, greater microbial reduction was observed (p<0.05) when the laser was associated to TB than when it was associated to MB (73.58% and 62.18%, respectively). Scanning electron microscopy showed that the appearance of the surface of yeasts cells in groups 2, 3 and 4 was similar (Fig. 1), suggesting that any alterations of the cells in these groups, if present, are not clearly seen on their surfaces. In groups 5, 6 and 7, alterations such as roughness or loss of cell wall were observed, and were most noticeable in group 7. These alterations on yeasts cell surfaces may represent cell destruction by PDT.
In spite of the encouraging results of the association of laser and TB or MB, further studies are required to confirm the efficacy of the photosensitizers to make their clinical application affordable and to standardize the doses of low-power lasers. This encourages further in vivo studies to be conducted in order to allow the use of this therapy in prevention of a number of oral pathologies and to explore PDT potential for treating immunocompromised patients. Moreover, the concentration, incubation time and type of photosensitizer, as well as the physiological state of microorganisms, exposure time and laser energy density may also influence the PDT results19.
CONCLUSIONS
1. C.albicans was susceptible to PDT, using either methilene blue or toluidine blue as photosensitizers.
2. The number of C. albicans CFU/mL was lower when TB was used.
1. Cannon RD, Lamping E, Holmes AR, Niimi k, Tanabe K, Niimi M, Monk C. Candida albicans drug resistance another way to cope with stress. Microbiology 2007;153:3211-3217. [ Links ]
2. Niimi M, Firth NA, Cannon RD. Antifungal resistance of oral fungi. Odontology 2010;98:15-25. [ Links ]
3. Herrera DR, Tay LY, Rezende, EC, Kozlowski Jr, VA, Santos, EB. In vitro antimicrobial activity of phytotherapic Uncaria tomentosa against endodontic pathogens. J Oral Sci 2010;52:473-476. [ Links ]
4. Resende JC, Resende MA. In vitro susceptibility of clinical isolates of Candida spp. from hospitalized patients. Mycoses 1999;42:641-644. [ Links ]
5. Teichert MC, Jones JW, Usacheva MN, Biel MA. Treatment of oral candidiasis with methylene blue-mediated photodynamic therapy in an immunodeficient murine model. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;93:155-160. [ Links ]
6. MacRobert AJ, Bown SG, Phillips D. What are the ideal properties of a photosensitizer? In: Photosensitizing Compounds: Their Chemistry, Biology and Clinical Use 1989;4-16. [ Links ]
7. Carvalho GG, Felipe MP, Costa MS. The photodynamic effect of methylene blue and toluidine blue on Candida albicans is dependent on medium conditions. J Microbiol 2009; 47:619-623. [ Links ]
8. Jori G. Photodynamic therapy of microbial infections: state of the art and perspectives. J Environ Pathol Toxicol Oncol 2006;25:505-519. [ Links ]
9. Garcez AS, Souza FR, Nuñes SC, Karher JM, Ribeiro MS. Terapia Fotodinâmica em Odontologia - Laser de Baixa Potência para Reduçao Microbiana. Rev APCD 2003;57: 223-226. [ Links ]
10. Wilson M, Mia N. Sensitization of Candida albicans to killing by low-power laser light. J Oral Pathol Med 1993; 22:354-357. [ Links ]
11. Resende JC, Resende MA. In vitro susceptibility of clinical isolates of Candida spp. from hospitalized patients. Mycoses 1999;42:641-644. [ Links ]
12. Wilson M, Burns T, Pratten J, Pearson GJ. Bacteria in supragingival plaque samples can be killed by low-power laser light in the presence of a photosensitizer. J Appl Bacteriol 1995;78:569-574. [ Links ]
13. Sennhenn-Kirchner S, Schwarz P, Schliephake H, Konietschke F, Brunner E, Borg-von Zepelin M. Decontamination efficacy of erbium:yttrium–aluminium-garnet and diode laser light on oral Candida albicans isolates of a 5-day in vitro biofilm model. Lasers Med Sci 2009;24:313-320.
14. Souza SC de, Junqueira JC, Balducci I, Koga-Ito CY, Munin E, Jorge AOC. Photosensitization of different Candida species by low power laser light. J Photochem Photobiol B 2006;83:34-38. [ Links ]
15. Giroldo LM, Felipe MP, de Oliveira MA, Munin E, Alves LP, Costa MS. Photodynamic antimicrobial chemotherapy (PACT) with methylene blue increases membrane permeability in Candida albicans. Lasers Med Sci 2009;24: 109-112. [ Links ]
16. O’Neill JF, Hope CK, Wilson M. Oral bacteria in multispecies biofilms can be killed by red light in the presence of toluidine blue. Lasers Surg Med 2002;31:86-90.
17. Sarkar S, Wilson M. Lethal photosensitization of bacteria in subgingival plaque from patients with chronic periodontitis. J Periodont Res 1993;28:204-210. [ Links ]
18. Fernandez JM, Bilgin MD, Grossweiner LI. Singlet oxygen generation by photodynamic agents. J Photochem Photobiol B 1997;37:131-140. [ Links ]
19. Teichert MC, Jones JW, Usacheva MN, Biel MA. Treatment of oral candidiasis with methylene blue-mediated photodynamic therapy in an immunodeficient murine model. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;93: 155-160. [ Links ]
20. Usacheva MN, Teichert MC, Biel MA. Comparison of the methylene blue and toluidine blue photobactericidal efficacy against gram-positive and gram-negative microorganisms. Laser Surg Med 2001;29:165-173. [ Links ]














