Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista argentina de cirugía
versión impresa ISSN 2250-639Xversión On-line ISSN 2250-639X
Rev. argent. cir. vol.114 no.2 Cap. Fed. jun. 2022
http://dx.doi.org/10.25132/raac.v114.n2.1613
Articles
Chronic suppuration or infected pseudocyst? A complication of incisional hernia repair with mesh
1 Servicio de Cirugía General. Sanatorio Dr. Julio Méndez. Buenos Aires. Argentina
2 Servicio de Ecografía. Sanatorio Dr. Julio Méndez. Buenos Aires. Argentina
3 División Emergencias. Sanatorio Dr. Julio Méndez. Buenos Aires. Argentina
The use of meshes for abdominal wall repair dramatically reduces the recurrence rate but can lead to complications such as chronic suppuration and pseudocysts.
Chronic suppurations usually present as collections that involve the mesh surrounded by “biofilm” and without tissue integration, which explains the failure of antibiotic therapy and the frequent need to remove the prostheses.
On the other hand, pseudocysts are collections of sterile serous fluid with a thick fibrotic wall that must be excised to ensure healing1.
Both conditions are characterized by the presence of an encapsulated collection resulting from excessive fibrosis due to the inflammatory reaction triggered by the presence of the prosthesis2.
We report the case of a 75-year-old female patient with a history of COPD and hysterectomy for uterine cancer at the age of 45, who sought medical advice due to a painful abdominal mass which appeared 6 months before consultation associated with asthenia, hyporexia and unquantified weight loss.
Thirteen years before, she had undergone Dixon surgery with protective colostomy due to tumor recurrence in another institution. After the intestinal continuity was restored, an incisional hernia developed and was repaired with a polypropylene mesh. During the postoperative period, a surgical site infection required debridement and antibiotics.
Clinical examination revealed an irreducible rounded tumor of approximately 12 cm in diameter below the scar.
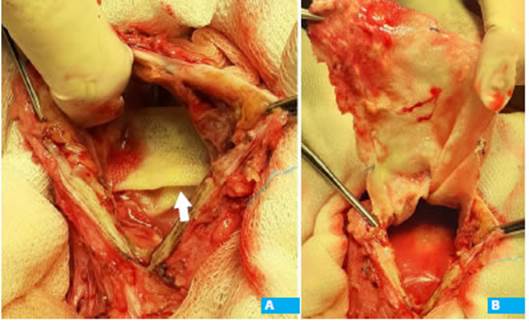
The laboratory tests were normal. The soft tissue mass ultrasound showed an encapsulated fluid collection in the parietal plane surrounding a solid mass that was interpreted as prosthetic material. A computed tomography (CT) scan confirmed the presence of the fluid collection but did not provide further information on the solid mass (Fig. 1).
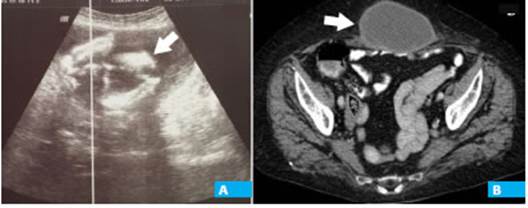
Figure 1 A: Ultrasound showing a superficial fluid collection with a solid component inside (arrow). B: Abdominal computed tomography scan with oral contrast (cross section): large thick-walled fluid collection of the abdominal wall (arrow).
The mass was approached through a lozenge-shaped skin incision including the scar; the anterior leaflet of the rectus sheath was markedly thickened, and the rectus muscles seemed atrophic. The sheath was incised and 150 mL of cloudy, amber-colored fluid were evacuated. A sample of this fluid was sent for bacteriological examination.
The mesh was folded and free in the preperitoneal plane and could be easily removed (Fig. 2). The bed was flushed and curetted to remove biofilm debris and a catheter was placed for drainage. The edges of the aponeurosis were sutured with 1.0 polypropylene.
The postoperative period evolved uneventful, and the catheter was removed 6 days later.
The culture was positive for Staphylococcus aureus sensitive to trimethoprim-sufamethoxazole, and the patient received oral treatment for 8 weeks.
She had favorable outcome and gained weight. An ultrasound scan performed six months later showed the integrity of the abdominal wall and scarce preperitoneal laminar fluid.
In open incisional hernia repairs, a wide dissection of the subcutaneous plane is usually necessary, resulting in an extended and prolonged healing process due to the sustained production of inflammatory mediators as a response to the heterologous material. Sometimes, the result is the production of fluid and dense fibrosis that prevents its reabsorption2. These fluid collections can evolve in the following different ways:
Spontaneous resorption.
Capsule formation and persistence as pseudocysts or chronic seromas1.
Acute infection, which usually responds to drainage associated with antibiotic treatment.
Subclinical infection with slow progression that hin ders mesh from tissue integration and, months or years later, manifests as a fluid collection around the prosthesis3-5.
We believe that most chronic infections originate from acute complications of the surgical site. In a series of 32 meshes removed due to infection, 16 patients had developed seromas or apparently mild postoperative infections that were managed with empirical antibiotic therapy for short periods of time5. Other authors have reported similar cases of chronic infection in meshes with no tissue integration. Aravind and Cook3 published a giant infected seroma after laparoscopic bilateral inguinal hernia repair with preperitoneal location and absence of capsule like in our case and, as in the report by Gukas and Massouh4, with the mesh “floating” in the collection.
In pseudocysts, meshes integrate with the native tissue, except for the case of Mantelou et al.6, who completely excised the pseudocyst wall en bloc with the mesh.
In the case presented, the imaging tests suggested a pseudocyst of the abdominal wall but, unlike most publications, the collection occupied the preperitoneal space instead of the supraaponeurotic space and lacked an own wall, since the “capsule” depended on the aponeurosis of the rectus muscles.
Our patient had presented general symptoms that could be attributed to chronic infection, as they resolved after surgery and antibiotic treatment. If the diagnosis had been suspected, we would have indicated percutaneous evacuation of the collection and antibiotic treatment guided by bacteriological culture before surgery. Probably, surgery would have been necessary due to the lack of tissue integration.
The CT scan provided information on the dimensions of the collection and its superficial location, but the ultrasound scan suggested the presence of the mesh folded inside the collection.
In agreement with Mayagoitía et al.1, we believe that both methods are complementary and should not be excluded, since the preoperative identification of the mesh without tissue integration could help to distinguish between pseudocysts and chronic infections with insidious course and to plan surgery with greater accuracy.
Referencias bibliográficas /References
1. Mayagoitía JC, Almaraz A, Díaz C. Two cases of cystic seroma following mesh incisional hernia repair. Hernia. 2006;10:83-6. [ Links ]
2. Klosterhalfen B, Junge K, Hermanns B, Klinge U. Influence of implantation interval on the long-term biocompatibility of surgical mesh. Br J Surg. 2002; 89:1043-8. [ Links ]
3. Aravind B, Cook A. Intra-abdominal giant infected seroma following laparoscopic inguinal hernia repair. Hernia. 2015;19:795-7. [ Links ]
4. Gukas ID, Massouh F. Serious life-threatening complication 5 years after laparoscopic totally extraperitoneal hernia repair: case report and discussion of the literature. Hernia. 2011;15:459-62. [ Links ]
5. Tolino MJ, Tripoloni DE, Ratto R, Garcia MI. Infections associated with prosthetic repairs of abdominal wall hernias: pathology, management and results. Hernia. 2009;13:631-7. [ Links ]
6. Mantelou AG, Georgiou GK, Harissis HV. Giant pseudocyst of the anterior abdominal wall after incisional hernia mesh repair: a rare case report. Hernia. 2014;18:141-4. [ Links ]
Received: February 08, 2021; Accepted: May 04, 2021











 texto en
texto en