Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista argentina de cirugía
versión impresa ISSN 2250-639Xversión On-line ISSN 2250-639X
Rev. argent. cir. vol.116 no.1 Cap. Fed. mar. 2024 Epub 26-Feb-2024
http://dx.doi.org/10.25132/raac.v116.n1.1722
Scientific letter
Splenectomy for sclerosing extramedullary hematopoietic tumor of the spleen
1Clínica Quirúrgica 3. Facultad de Medicina. UdelaR. Hospital Maciel. Montevideo. Uruguay.
Extramedullary hematopoietic tumors are rare and characterized by the presence of hematopoietic elements at various stages of maturity, atypical megakaryocytes, and fibroblastic proliferation.
We report the case of a patient with sclerosing extramedullary hematopoietic tumor of the spleen.The patient was 71-year-old man with a history of hypertension, diabetes, and hepatitis C virus infection. Multiple spleen lesions were identified in imaging tests during workup due to abdominal discomfort. Although a vascular tumor was suspected, laparoscopic splenectomy was decided after considering other possible causes. The pathology examination revealed a sclerosing extramedullary hematopoietic tumor of the spleen, which was confirmed by immunohistochemical tests. These tumors are usually single or, less frequently, multiple lesions affecting different organs and are associated with chronic myeloproliferative syndromes. The histologic confirmation is mandatory due to their similarity to malignant tumors. Extramedullary hematopoietic tumors are rare, and there is little scientific clinical evidence regarding their diagnosis and management. The histological confirmation is mandatory due to their similarity to malignant tumors.
Keywords: extramedullary hematopoietic tumor; myeloproliferative syndrome; extramedullary hematopoiesis
Extramedullary hematopoietic tumors are rare and characterized by the presence of hematopoietic elements at various stages of maturity, atypical megakaryocytes, and abundant fibroblastic proliferation1),(2.
These tumors were first described by Remstein in 2000, but their incidence is unknown as there are only reports of clinical cases in the current literature1),(2),(3),(4),(5.
We report the case of a patient with sclerosing extramedullary hematopoietic tumor of the spleen.
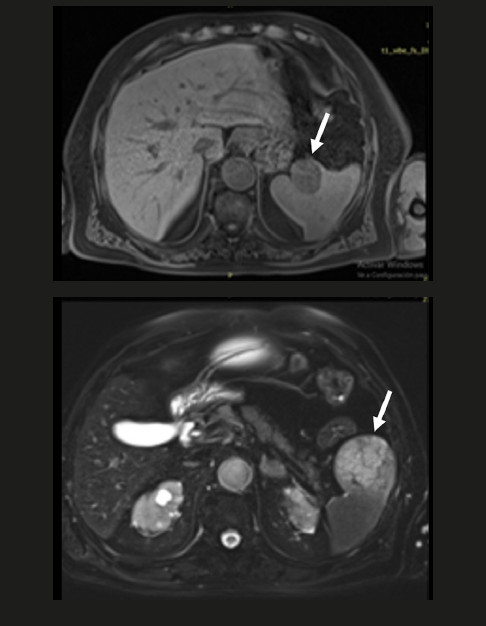
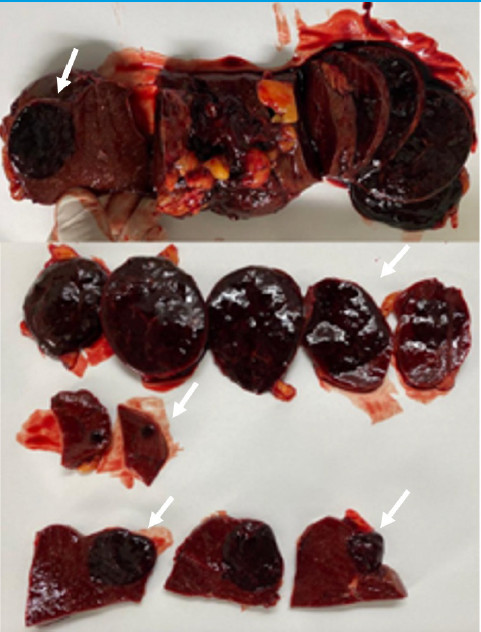
The patient was 71-year-old man with a history of hypertension, diabetes, prostate cancer 10 years before presentation, and hepatitis C virus infection who was being evaluated for abdominal discomfort. An abdominal ultrasound revealed an enlarged spleen with regular and well-circumscribed borders, and round-shaped echogenic lesions measuring between 30 and 45 cm without vascularization. The rest of the parenchyma was homogeneous. The magnetic resonance imaging (MRI) showed three rounded, solid lesions in the spleen, measuring between 5.5 and 3.5 cm, low signal intensity on T1 and T2 images, restricted diffusion, and heterogeneous enhancement in delayed phases (Fig. 1). The patient did not complain of any symptoms related to the spleen. A vascular tumor was suspected, but other possible causes, whether benign or malignant, were also taken into consideration. The patient underwent laparoscopic splenectomy, which was performed without any complications and was discharged on postoperative day 5. The pathology examination reported sclerosing extramedullary hematopoietic tumor of the spleen, which was confirmed by immunohistochemical tests (Fig. 2).
We were unable to conduct a diagnostic assessment of diseases that caused these lesions, such as myeloproliferative syndromes, through a bone marrow biopsy because the patient was infected with COVID-19 which resulted in significant post-COVID-19 complications.
Nevertheless, the diagnosis of sclerosing extramedullary hematopoietic tumor of the spleen was made by pathological anatomy and immunohistochemical tests. Yet, the presence of myeloproliferative syndrome could not be confirmed or ruled out.
The literature does not describe a specific incidence of extramedullary hematopoietic tumors because the majority of the publications are case reports, where this information is not provided, and these tumors are described as rare tumors.
All the cases reviewed had a past medical history of myeloproliferative syndromes1),(2),(3),(4),(5, except for one3 in which, as in our case, a bone marrow biopsy could not be performed, and the presence of hematologic disease could not be confirmed.
These tumors usually present as single or, less frequently, multiple lesions1 and may occur in different organs. The spleen, liver, kidney, lymph nodes and reptroperitoneum are most commonly affected; skin or lung involvement is rare2),(3),(5.
The pathogenesis of these lesions is unknown. Extramedullary hematopoietic tumors are associated with chronic myeloproliferative syndromes, particularly idiopathic myelofibrosis, characterized by clonal proliferation of hematopoietic stem cells1),(2.
Moreover, we did not find any relationship in the literature between the patient’s past medical history and hematopoietic tumors.
From a pathophysiological perspective, inadequate release of growth factors by megakaryocytes and platelets may activate the release of cytokines such as TGF-β, platelet-derived growth factor, epidermal growth factor, and calmodulin. These cytokines stimulate the proliferation of fibroblasts, promote angiogenesis, and facilitate the deposition of extracellular matrix proteins, ultimately favoring the formation of extramedullary hematopoietic tumors5.
Histologically, extramedullary hematopoietic tumors differ from extramedullary hematopoiesis (EMH), which is defined as the presence of hematopoietic elements outside the bone marrow. and can occur in diseases such as severe anemia, thalassemia, and polycythemia vera. It is often difficult to distinguish between both entities, but although EMH can form masses, the hematopoietic elements are observed in different stages of maturity. In addition, EMH is more cellular, less fibrotic and has no atypical megakaryocytes1),(4),(5. Instead, sclerosing extramedullary hematopoietic tumors are rare tumors characterized by the presence of trilineage hematopoietic elements, atypical megakaryocytes, and abundant fibroblastic proliferation. Immunohistochemical staining is typically positive for myeloperoxidase, hemoglobin, antifactor VIII antibodies, CD34+, CD41+, CD61+, CD15 and CD302),(3),(4.
These tumors can be asymptomatic, as in our case, or exhibit symptoms due to involvement of adjacent organs1.
Abdominal pain was the predominant symptom in all the cases reviewed1),(2),(3),(4),(5; other common symptoms include asthenia and weight loss1),(3. Tumors in the right colon may be associated with mucinous bloody stools and diarrhea5.
These lesions should be well characterized to exclude differential diagnoses with malignant tumors such as sclerosing liposarcoma, malignant fibrous histocytoma, Hodking’s disease, and myelolipoma1),(2; therefore, their histopathologic diagnosis is essential because of the therapeutic and prognostic implications of each tumor.
The presence of hematopoietic tumors in myeloproliferative disorders is considered a predictor of adverse outcome, as they usually occur at advanced
Imaging tests may elicit different findings.
Extramedullary hematopoiesis often presents as homogeneous liver and spleen enlargement, but in some cases, such as ours, it presents with masses that make it difficult to differentiate from malignancy.
Lesions are usually multiple, but the characteristics vary according to their age, activity and location.
Newer lesions are more active and appear as hypoechoic masses on ultrasound, hypodense masses compared to the adjacent muscle on computed tomography (CT), and intermediate signal intensity on T1 images and hyperintense signal on T2 images on MRI. Diffusion may be restricted because of the high cellularity of these lesions. Active EMH can show decreased signal intensity in T1-weighted gradientecho sequences.
In chronic lesions, hematopoietic activity decreases and the fibrous component progressively increases, resulting in changes in imaging tests. On ultrasound, masses may appear iso- or hyperechoic. On CT, they may be isodense or hyperdense with minimal contrast enhancement. On MRI, they become hypointense in both T1 and T2 sequences and show little or no restriction in diffusion.
It is not uncommon to see areas of both active and less active hematopoiesis within the same mass6.
The diagnosis of these lesions is often challenging and requires histologic examination through percutaneous biopsy, surgical biopsy or even excision of the lesion or organ involved, depending on each case1),(2),(3),(4),(5. Surgery is necessary to manage complications.
Unlike most case reports, in which patients present with a history of chronic myeloproliferative syndromes, our clinical case constituted an incidentaloma and the diagnosis was made by surgery.
Extramedullary hematopoietic tumors are rare, and there is little scientific clinical evidence regarding their diagnosis and management.
The etiopathogenesis of these tumors is unclear and is associated with chronic myeloproliferative syndromes.
The imaging findings vary according to the age of the lesions and their location and are not easy to categorize.
Distinguishing this condition from other malignancies can be difficult, and surgery is frequently necessary.
Further research studies are needed to make progress in the diagnosis and treatment of these tumors.
Referencias bibliográficas /References
1. Yang X, Bhuiya T, Esposito M. Sclerosing extramedullary hematopoietic tumor. Ann Diagn Pathol. 2002;6(3):183-7. [ Links ]
2. Wang D, Castro E, Rao A, McPhaul CM. Sclerosing Extramedullary Hematopoietic Tumor: A Case Report. J Investig Med High Impact Case Rep. 2020;8:2324709620956463. [ Links ]
3. Dema S, Lazar F, Barna R, Dobrescu A, Dema ALC, Popa O, et al. Sclerosing Extramedullary Hematopoietic Tumor (SEHT) mimicking a malignant bile duct tumor-case report and literature review. Medicina (Kaunas) [Internet]. 2021;57(8):824. [ Links ]
4. Deniz K, Kahriman G, Koçyigit I, Ökten T, Ünal A. Sclerosing Extramedullary Hematopoietic Tumor. Turk J Haematol. 2018;35(3):209-210. [ Links ]
5. Zuo Z, Zhang Q, Wu W, Li X, Zhang L, Wang J, et al. Sclerosing extramedullary hematopoietic tumor of the colon: A case report and literature review. Exp Ther Med [Internet]. 2023;25(3):132. [ Links ]
6. Malla S, Razik A, Das CJ, Naranje P, Kandasamy D, Kumar R. Marrow outside marrow: imaging of extramedullary haematopoiesis. Clin Radiol. 2020;75(8):565-78. [ Links ]
Received: October 21, 2022; Accepted: July 14, 2023











 texto en
texto en