Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista argentina de cirugía
versión impresa ISSN 2250-639Xversión On-line ISSN 2250-639X
Rev. argent. cir. vol.116 no.2 Cap. Fed. jun. 2024 Epub 01-Jun-2024
http://dx.doi.org/10.25132/raac.v116.n2.1763
Original article
Computed tomography scan after major abdominal surgery
1Instituto Médico Platense, La Plata, Buenos Aires, Argentina.
Background:
Major abdominal surgeries may present serious postoperative complications that require early diagnosis.
Objective:
The aim of this study was to determine the usefulness of computed tomography (CT) for the early diagnosis of major abdominal surgery complications.
Material and methods:
We conducted a retrospective, observational and descriptive study using data obtained from the medical records of patients undergoing major abdominal surgery in a private hospital. Patients were divided into two groups according to the presence or absence of symptoms suggesting a postoperative complication. Patients with symptoms were classified into 3 groups: without CT, with CT with positive findings and with CT without abnormal findings.
Results:
A total of 154 patients were analyzed; mean age was 61.3 ± 12.5 years and 83 (54%) were male. Of 48 patients (31%) with symptoms suggestive of complications, 6 had very evident symptoms and were re-operated without CT, 7 had positive findings on CT and CT was negative in 14/41. All the patients had findings that supported the decision to re-operate. There were 27 cases (17.5%) with grade 3b complications of the Clavien-Dindo classification and 3 patients (2%) died.
Conclusion:
Computed tomography was useful to confirm a complication, but not to rule it out. Clinical parameters remain of utmost importance in patients with symptoms and absence of abnormal findings in post-operative CT.
Keywords: general surgery; postoperative complications; computed tomography
Introduction
Major abdominal surgeries, which include gastrointestinal, esophagogastric, hepatobiliary and pancreatic, and colorectal procedures, may present serious postoperative complications. It is important to differentiate these events from the expected postoperative changes in order to detect complications such as bleeding, occlusion, evisceration, and sepsis, and to reduce morbidity and mortality. Various methods have been used to evaluate the postoperative period. These methods are based on clinical, laboratory, and imaging variables.
The Sepsis Related Organ Failure Assessment (SOFA) score and the quick Sequential Organ Failure Assessment (qSOFA) score are commonly used prognostic scales based on clinical variables. While sensitive, they lack specificity. Among laboratory variables, acute phase reactants such as C-reactive protein have recently become more relevant1,2. The imaging tests more commonly used are ultrasound and computed tomography (CT) scan. Ultrasound is a cost-effective and bedside tool, but it lacks specificity and is operator dependent. The sensitivity and specificity of CT scan are higher to detect complications3.
The aim of this study was to determine the usefulness of CT for the early diagnosis of major abdominal surgery complications.
Material and methods
We conducted a retrospective, observational and descriptive study using data obtained from the medical records of patients undergoing major abdominal surgery between March 2022 and May 2023. The identity of the patients was protected.
Inclusion criteria: elective and emergency major abdominal surgery, either open or through laparoscopy, due to inflammatory causes or neoplasms.
Major abdominal surgery was defined as any gastrointestinal resection with anastomosis or ostomy, esophagogastric surgery, hepatobiliary and pancreatic resections and colorectal resections. All the procedures mentioned above are included in one of the levels 5-7-8-9-10 of Asociación Argentina de Cirugía fee schedule4.
Postoperative patient management included intravenous fluid therapy using continuous infusion pump, antiemetic and gastroprotective medications (metoclopramide and omeprazole), analgesia with diclofenac 75 mg every 12 hours for all patients with creatinine levels ≥ 1.2 g/dL. Opioids were indicated as soon as the anesthesiologist removed the epidural catheter placed in the operating room.
The urinary catheter was removed if diuresis was > 50 mL/h at 24 hours postoperatively, and nutrition was initiated according to the ERAS® protocol5,6.
In the postoperative period, re-operations and their causes were analyzed according to the Clavien-Dindo classification7 and distributed as follows: accidental injury, anastomotic fistula, postoperative ileus, subphrenic collection, hemorrhage, and evisceration.
Patients were divided into two groups: one with a favorable postoperative course without symptoms and the other with symptoms suggesting a postoperative complication. In this second group, patients were divided into two subgroups: those who did not undergo CT (T0) and those who did so. Among the patients who underwent CT, those with images suggestive of complications were classified as T+ and those without such images were classified as T-. The CT scans were categorized based on whether they were performed within 48 hours after the operation, between 48 hours and 7 days, or after 7 days. The re-operations and their indications were also analyzed. A descriptive analysis was performed to compare positive findings (T+) with re-operations across all groups. The decision-making process is described in the flowchart in Figure 1.
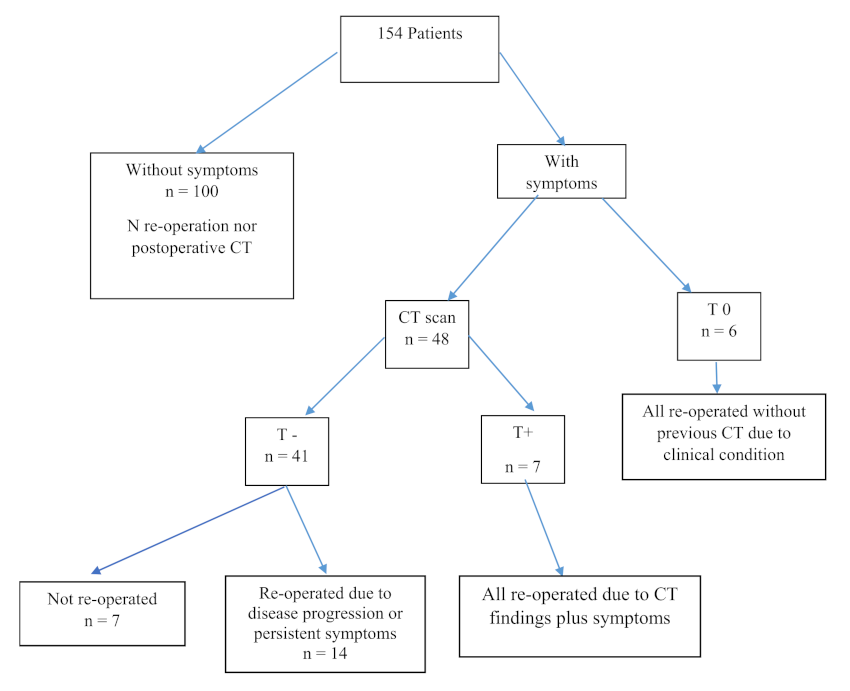
FIGURE 1 Flow diagram of the decision-making process for patients after major abdominal surgery Abbreviations: S+: with symptoms; S-: without symptoms; T0: Without CT; T+: with abnormal CT findings; T-: without abnormal CT findings
S+ was defined in the presence of any of the following: tachycardia (heart rate > 100/min), qSOFA (respiratory rate ≥ 22 breaths/min, altered mental status, systolic blood pressure ≤ 100 mm Hg), fever (axillary temperature > 38°C), postoperative paralytic ileus (absence of bowel sounds or bowel motility 96 hours after surgery or greater)8, pain (reported by the patient with ≥ 6 points on the verbal numeric scale despite receiving the prescribed analgesia), changes in color, odor, or amount of drain output, or evisceration.
T+ was defined as any of the following9:
Seroma: homogeneous, low attenuation (-10 to 20 HU) fluid collection adjacent to the wound, without enhancement.
Hematoma: heterogeneous hyper-attenuating (20 to 60 HU) fluid collection adjacent to the wound, without enhancement.
Wall infection/abscess: heterogeneous fluid collection near the incision.
Low/medium (variable) attenuation fluid collection(s) with irregular borders and increased uptake that may contain fluid-fluid or air-fluid levels.
Dehiscence and incisional hernia: separation of fascial edges beneath skin incision, with or without visceral protrusion.
Organ/space infection: abnormalities of the tissue surrounding the anastomosis, seen on imaging as air with rarefaction of the fat planes or as an abscess close to the anastomosis.
Abnormal portal flow: absence of contrast enhancement in portal venous phase.
T- was defined as10:
Surgical material: metal clips/staples, sutures, drainage catheters, hemostats, prosthesis, etcetera.
Changes in the anterior abdominal wall: alterations in subcutaneous fat tissue attenuation, occasionally accompanied by small amounts of fluid with a laminar distribution and some air bubbles at this level.
Inflammatory changes in intraperitoneal fat: edema surrounding organ/space with increased fat density.
Extraperitoneal gas: particularly after laparoscopic surgery.
Pneumoperitoneum: expected within the first 3 days after laparoscopy and up to 5 days after laparotomy.
Free peritoneal fluid: small amounts within the first 48-72 hours.
Postoperative paralytic ileus: generalized distension of intestinal loops, without abrupt transition point and with presence of air in the rectum.
Pleural effusion: accumulation of fluid in the space between the two layers of the pleura.
All CT scans were performed using a high- resolution Toshiba Aquilion 64 CT scanner. Intravenous contrast agent was used in the absence of kidney failure.
Results
We analyzed the medical records of 154 patients; mean age was 61.3 ± 12.6years and 83 (54%) were men. Fifty-four patients (35%) had symptoms suggestive of complications and 27 of them were re- operated.
Six patients with symptoms, who did not undergo CT scanning (T0), were re-operated due to clinical parameters such as tachycardia, fever, prolonged ileus, or changes in drain output. All of them had positive findings, including hemoperitoneum, evisceration, anastomotic fistula, inadvertent injury, or collection with anastomotic fistula.
The 7 patients with symptoms and suggestive tomographic findings (T+) underwent re-operation. All of them had different findings that supported the surgical management, such as evisceration, hemorrhage, anastomotic fistula, inadvertent lesion, or subphrenic collections.
Of the 41 symptomatic cases without suspicious tomographic findings (T-), 14 were re- operated because their symptoms persisted. In all cases, the surgical findings supported the chosen course of action: anastomotic fistulas, intra-abdominal collections, ureteral injuries, or other types of injuries. The remaining 27 patients did not require re-operation because their clinical condition resolved.
Of the total series of patients who underwent major abdominal surgery, 27 patients (17.5%) had complications requiring general anesthesia or had organ failure (Clavien-Dindo grades 3b and 4). None of the patients were treated with local anesthesia. Mortality rate was 2% (n = 3).
Of the 48 CT scans performed, 12 were conducted within 48 hours after the operation, 25 between 48 hours and 7 days, and 11 after 7 days.
In S+ patients, CT confirmed that 7 patients had true positive results, 27 had true negative results, 14 had false negative results and there were no false positive results.
Most complications occurred between 48 hours and postoperative day 7.
Please refer to tables in the Supplementary Material for further details (Table 1, 2, 3 and 4).
Discussion
The ideal time to perform a post-operative CT scan is still an open question. Some authors suggest early scanning to avoid late re-operations, because of the limited value of physical examination, particularly in patients on mechanical ventilation under the effect of muscle relaxants11. Other authors use a cut-off point of 72 hours12.
The absence of abnormal findings on computed tomography does not rule out the possibility of a postoperative complication13. Tachycardia and a positive qSOFA score were the most useful tools for detecting complications. In the 2018 Annual Report of Surgery, tachycardia was the most commonly observed sign and proved to be a relevant predictor of complications14.
In our study, imaging provided 13% of the information necessary to make the decision to re- operate, which was lower than the 50% reported by the guidelines of the French Society of Anesthesia15,16. It should be noted that in this study, the CT scan was requested after clinical and ultrasound findings with a high suspicion of complication. The 3 deaths occurred in T- patients who underwent late re-operation (after postoperative day 7). These data are consistent with the aforementioned guideline, which states that the identification of a postoperative complication and the decision to immediately perform a new laparotomy reduce multiple organ failure by 60% and improve survival.
Our study has two limitations: the retrospective nature of the sample and the fact that C-reactive protein17 was not measured to detect complications due to limited availability for 24-hour testing. In the PRECious trial PREdiction of Complications, CT was indicated only when CRP levels exceeded a certain value18.
To the best of our knowledge, this is an original work in Argentina. We did not find similar reports in the bibliography.
The decision to re-operate a patient after major abdominal surgery should be made by consensus among the treating physicians. This decision should be based on the evaluation of all available data. No single imaging score or method is sufficient to confirm a complication. Clinical parameters remain of utmost importance.
Based on the presented results, we can conclude that a postoperative CT scan with positive findings after major abdominal surgery supports the decision to re-operate. Nevertheless, the absence of this finding does not exclude this possibility.
REFERENCES
1. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016 Feb 23;315(8):801-10. doi: 10.1001/jama.2016.0287. PMID: 26903338; PMCID: PMC4968574. [ Links ]
2. Neira-Sánchez ER, Málaga G. Sepsis y las nuevas definiciones, ¿es tiempo de abandonar SIRS? Acta Med Peru 2016; 33(3): 217-22. [ Links ]
3. Van Randen A, Laméris W, van Es HW, van Heesewijk HP, van Ramshorst B, Ten Hove W y et al. A comparison of the accuracy of ultrasound and computed tomography in common diagnoses causing acute abdominal pain. Eur Radiol. 2011 Jul;21(7):1535-45. doi: 10.1007/s00330-011-2087-5. [ Links ]
4. Nomenclador Nacional de cirugías por la Asociación Argentina de Cirugía. https://aac.org.ar/imagenes/nomenclador/ nomenclador_ACC-01-06-2023.pdf. Consultado el 21/07/2023 [ Links ]
5. Ljungqvist O. ERAS(r) --enhanced recovery after surgery: moving evidence-based perioperative care to practice. JPEN J Parenter Enteral Nutr. 2014 Jul;38(5):559-66. doi: 10.1177/0148607114523451. Epub 2014 Feb 24. PMID: 24567343. [ Links ]
6. Barbero M, García J, Alonso I, Alonso L, San Antonio-San Román B, Molnar V,y col. ERAS(r) protocol compliance impact on functional recovery in colorectal surgery. Cir Esp (Engl Ed). 2021 Feb;99(2):108-114. English, Spanish. doi: 10.1016/j.ciresp.2020.05.010. Epub 2020 Jun 18. PMID: 32564875. [ Links ]
7. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009 Aug;250(2):187-96. doi: 10.1097/SLA.0b013e3181b13ca2. PMID: 19638912. [ Links ]
8. O'Malley RB, Revels JW. Imaging of Abdominal Postoperative Complications. Radiol Clin North Am. 2020 Jan;58(1):73-91. doi: 10.1016/j.rcl.2019.08.007. Epub 2019 Oct 21. PMID: 31731904. [ Links ]
9. de Araújo Matins-Romeo D, Rivera Domínguez A. Complications after abdominal surgery. Radiologia (Engl Ed) 2023 Mar:65 Suppl 1:S99-S108.spaña. doi: 10.1016/j.rxeng.2022.09.012. PMID:37024236. [ Links ]
10. González López A, Ballesteros Gomiz E, Sola` García M, Rivera Valladares L, Cheranovskiy V, Prieto Del Rey MJ. Revisión de los hallazgos radiológicos normales después de las principales cirugías abdominales. seram [Internet]. 22 de noviembre de 2018 [citado 29 de octubre de 2023];. Disponible en: https://piper.espacio-seram.com/index.php/seram/article/view/346 [ Links ]
11. Bader FG, Schröder M, Kujath P, Muhl E, Bruch HP, Eckmann C. Diffuse postoperative peritonitis -value of diagnostic parameters and impact of early indication for relaparotomy. Eur J Med Res. 2009 Nov 3;14(11):491-6. doi: 10.1186/2047-783x-14-11-491. PMID: 19948445; PMCID: PMC3352290. [ Links ]
12. Wagner M, Zappa M, Maggiori L, Bretagnol F, Vilgrain V, Panis Y. Can postoperative complications be predicted by a routine CT scan on day 5? A study of 78 laparoscopic colorectal resections. Tech Coloproctol. 2014 Mar;18(3):239-45. doi: 10.1007/s10151-013-1047-2. Epub 2013 Jul 17. PMID: 23860629. [ Links ]
13. Kornmann VNN, van Ramshorst B, Smits AB et al. Beware of false-negative CT scan for anastomotic leakage after colonic surgery. Int J Colorectal Dis 29, 445-451 (2014). https://doi.org/10.1007/s00384-013-1815-5 [ Links ]
14. Canullán CM, Zandalazini HI. Complicaciones posoperatorias de la cirugía laparoscópica. Rev Argent Cirug 2021; 110 (SUPLEMENTO 1): S13-S185. Retrieved from https://revista.aac.org.ar/index.php/RevArgentCirug/article/view/269 [ Links ]
15. Perrone G, Sartelli M, Mario G, Chichom-Mefire A, Labricciosa FM, Abu-Zidan FM, Ansaloni L, et al. Management of intra-abdominal-infections: 2017 World Society of Emergency Surgery guidelines summary focused on remote areas and low-income nations. Int J Infect Dis. 2020 Oct;99: 140-148. doi: 10.1016/j.ijid.2020.07.046. Epub 2020 Jul 31. PMID: 32739433. [ Links ]
16. Hutchins RR, Gunning MP, Lucas DN, Allen-Mersh TG, Soni NC. Relaparotomy for suspected intraperitoneal sepsis after abdominal surgery. World J Surg. 2004 Feb;28(2):137-41. doi: 10.1007/s00268-003-7067-8. Epub 2004 Jan 8. PMID: 14708056. [ Links ]
17. Straatman J, Cuesta MA, Gisbertz SS, Van der Peet DL. Value of a step-up diagnosis plan: CRP and CT-scan to diagnose and manage postoperative complications after major abdominal surgery. Rev Esp Enferm Dig. 2014 Dec;106(8):515-21. PMID: 25544408. [ Links ]
18. Straatman J, Cuesta MA, Hermien Schreurs WH, Boudewijn J. Dwars BJ, Cense HA, et al. The PRECious trial PREdiction of Complications, a step-up approach, CRP first followed by CT-scan imaging to ensure quality control after major abdominal surgery: study protocol for a stepped-wedge trial. Trials 2015 Aug; 28: 16:382. PMID:26314740 DOI:10.1186/s13063-015-0903-y [ Links ]
ADDENDUM
TABLE 1 Surgeries performed and results of postoperative CT
| Surgery | Total Patients n=154º | CT scan= 48 | T+ n= 7 | T0 = 6 | T-Late re-operation n=14 | |
|---|---|---|---|---|---|---|
| Colon and rectal surgery | Hartmann | 9 | 5 | 0 | 1 | 2 |
| Right hemicolectomy | 20 | 6 | 1 | 1 | 1 | |
| Left hemicolectomy | 36 | 11 | 0 | 1 | 5 | |
| Total colectomy | 1 | 1 | 0 | 0 | 0 | |
| Dixon’s procedure | 7. | 2 | 0 | 0 | 1 | |
| Pancreatectomy and splenectomy | 5 | 0 | 0 | 1 | 0 | |
| Pancreaticoduodenectomy | 6 | 4 | 0 | 1 | 1 | |
| Liver resections | 12 | 5 | 1 | 0 | 1 | |
| Gastrectomies | 15 | 2 | 1 | 0 | 0 | |
| Esophagectomies | 1 | 1 | 0 | 0 | 0 | |
| Enterectomies | APA | 4 | 1 | 1 | 0 | 1 |
| AAI | 4 | 3 | 0 | 0 | 1 | |
| AOA | 11 | 2 | 2 | 0 | 1 | |
| Hepaticojejunostomy | 1 | 0 | 0 | 0 | 0 | |
| Restoration of intestinal continuity | 18 | 4 | 1 | 1 | 0 | |
| Retroperitoneal tumor | 3 | 0 | 0 | 0 | 0 | |
| Cystogastrostomy | 1 | 1 | 0 | 0 | 0 | |
Abbreviations: AAI: acute abdominal inflammation; AOA: acute occlusive abdomen; APA: acute perforated abdomen
TABLE 2 Patients with symptoms and abnormal CT findings (S+ T+).
| Surgery | Symptoms | CT scan (T+) | Time to CT | Finding on re- operation | Time to re-operation |
|---|---|---|---|---|---|
| Enterectomy with ilesotomy | Ileus, Tachycardia Pain | Evisceration | 72 h | Evisceration | 72 h |
| Total gastrectomy | Hypotension Tachycardia Aphagia | Free peritoneal fluid | 72 h | Bleeding events | 72 h |
| Laparoscopic right portal vein embolization for ALPPS | qSOFA 3/3 Tachycardia | Portal vein thrombosis | 30 h | Portal vein thrombosis | 30 h |
| RIC | Changes in drain output Fever | Subphrenic collection | 5 days | Subphrenic collection | 5 days |
| Enterectomy with enteroenterostomy due to AOA | Fever Abdominal pain | Subphrenic collection | 11 days | Subphrenic collection | 12 days |
| Laparoscopic right hemicolectomy | Fever | Organ/space infection | 72 h | Anastomotic fistula | 72 h |
| Enterectomy with enteroenterostomy due to AOA | Fever | Organ/space infection | 10 days | Inadvertent injury | 10 days |
Abbreviations: AOA: acute occlusive abdomen; RIC: restoration of intestinal continuity
TABLE 3 Patients re-operated due to clinical condition without abnormal CT findings
| Surgery | Symptoms | CT findings (T-) and time | 2nd (S+) Time | Time to re-operation | Finding |
|---|---|---|---|---|---|
| Hartmann’s procedure | Thick drain output | Free peritoneal fluid Ileus Day 6 | Day 8 qSOFA 2/3 Tachycardia | 9 days | Distal stump opening |
| PD | Abdominal pain Tachycardia | Free peritoneal fluid Ileus Day 6 | Tachycardia qSOFA 2/3 Day 8 | 8 days | Fistula of the bottom end of the Roux-en-Y anastomosis Death |
| Left hemicolectomy | Fever | Collection measuring 2x3 cm 48 h | Fever Tachycardia Persistent Day 5 | 6 days | Collection puncture |
| Left hemicolectomy | Fever Vomiting | Pleural effusion Free peritoneal fluid Day 8 | Fecal and sanguineous drain output Day 10 | 10 days | Small bowel fistula |
| Laparoscopic Dixon’s procedure | Ileus Tachycardia Serous drain output | 48 h DT urogram free fluid | Increased drain output Day 4 | 4 days | Right ureter injury |
| Rectum suture due to APA | Ileus Pain Tachycardia | 24 h Ileus | Fecal drain output Day 3 | 3 days | Inadvertent injury |
| Right hemicolectomy | Tachycardia Fever Abdominal pain | 72 h pop Ileus pneumoperitoneum | qSOFA 2/3 Tachycardia Day 10 | 10 days | Anastomotic fistula |
| Enterectomy with enteroenterostomy due to AAI | Pain Ileus | Day 6 Ileus | Tachycardia, pain tachypnea Day 8 | 8 days | Anastomotic fistula |
| Left hemicolectomy | Ileus Tachycardia | Pop day 4 Ileus | Abdominal pain qSOFA 2/3 Tachycardia Day 6 | 7 days | Anastomotic fistula Death |
| Enterectomy with enteroenterostomy due to AOA | Ileus Fever | Pop day 7 Ileus | qSOFA 2/3 Day 9 | 9 days | Collecyion + percutaneous Fistula Death |
| Left hemicolectomy | Pain tachypnea | 24 h pop Ileus-pneumoperitoneum | qSOFA 2/3 Tachycardia 72 h | 4 days | Anastomotic fistula |
| Hartmann + hysterectomy | Pain Ileus Fever | Day 7 Organ/space edema | qSOFA + Tachycardia Day 9 | 9 days | Pelvic collection |
| Left hemicolectomy | Pain Ileus | Day 6 Ileus | qSOFA + Day 9 Tachycardia | 9 days | Anastomotic fistula |
| Liver lobectomy | Pain Fever | 24 h pop Pneumoperitoneum Free peritoneal fluid | Day 7 Fever Tachycardia | 7 days | Liver collection |
TABLE 5 Patients re-operated without previous CT
| Surgery | Symptoms | Finding on re-operation | Time to re-operation |
|---|---|---|---|
| Pancreatectomy and splenectomy due to tumor in the pancreas tail | Tachycardia Sanguineous drain output | HemoperitoFneum | < 24 h |
| Right hemicolectomy with ileostomy and mucous fistula due to tumor of the cecum | Tachycardia Thick drain output | Inadvertent injury | 3 days |
| Hartmann’s procedure due to deverticular tumor | Evisceration | Aponeurosis opening | 7 days |
| Left hemicolectomy with anastomosis due to tumor in the sigmoid colon | Tachycardia Evisceration | Organ/space collection with anastomotic fistula | 10 days |
| Hartmann’s reconstruction | Tachycardia Fecal drain output | Anastomotic fistula | 5 days |
| PD due to tumor in the head of pancreas | qSOFA 2/3 | Hemoperitoneum | 7 days |
Received: July 21, 2023; Accepted: January 19, 2024











 texto en
texto en 



