Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista argentina de cirugía
versión impresa ISSN 2250-639Xversión On-line ISSN 2250-639X
Rev. argent. cir. vol.116 no.2 Cap. Fed. jun. 2024 Epub 01-Jun-2024
http://dx.doi.org/10.25132/raac.v116.n2.1721
Scientific letter
From a neuropsychiatric disorder to the correct diagnosis of insulinoma resolved by major pancreatic resection
1Servicio de Cirugía General, sector Hepatobiliopancreática, Hospital Escuela Gral. José F. de San Martin, Corrientes, Argentina. Grupo Quirúrgico HPB NEA.
2Servicio de Clínica Médica, Hospital Escuela Gral. José F. de San Martin, Corrientes, Argentina.
3Servicio de Anatomía Patológica, Hospital Escuela Gral. José F. de San Martin, Corrientes, Argentina.
Insulinomas are rare pancreatic tumors usually benign with an incidence of 0.4%. They are more common in women with a female-to-male ratio of 2:1. It is the most common functioning neuroendocrine tumor of the pancreas and is responsible for 70-75% of hyperinsulinemia in clinical practice1. The diagnosis is often a challenge, and a delay in diagnosis can have serious consequences for the patient. Surgical treatment is curative in more than 90% of cases, and the conservative approach is the treatment of choice whenever possible. We report the case of a cephalic pancreaticoduodenectomy (CPD) due to an insulinoma in a male patient with a previous misdiagnosis of a neuropsychiatric disorder treated with anticonvulsants.
Keywords: insulinoma; cephalic pancreaticoduodenectomy; hyperinsulinism; anticonvulsants; medical error
Insulinomas, although rare, are by far the most common pancreatic endocrine tumors. Most insulinomas (90%) are benign and solitary tumors, with a diameter < 2 cm and uniform distribution throughout the gland. This tumor may be a part of the multiple endocrine neoplasia type 1 (MEN-1) syndrome, in which case the tumors are almost always multiple.
The clinical picture includes non-specific adrenergic symptoms such as anxiety, sweating, and palpitations. There are also sporadic manifestations of true organic endogenous hyperinsulinism, which are characterized by neuroglycopenic symptoms such as confusion, amnesia, visual disturbances, seizures, and coma.
It is recommended that the presence of neuroglycopenic symptoms prompt a systematic workup. However, this is not always the case, as the clinical presentation can vary considerably, from a seizure to a car accident with episodic amnesia. Therefore, the diagnosis requires high level of suspicion2. We report the case of a cephalic pancreaticoduodenectomy (CPD) due to an insulinoma in a male patient with a previous diagnosis of a neuropsychiatric disorder performed 14 months after the onset of symptoms and treated with anticonvulsants for eight months before consulting our institution.
In March 2021, a 49-year-old otherwise healthy male patient presented profuse sweating, predominantly at night, and episodes of syncope, predominantly in the morning with amnesia of the episode. He was transferred to the nearest emergency department where a diagnosis of dehydration was made. However, he continued to experience sweating, asthenia, and dizziness, particularly in the morning. After six months, the condition worsened with a new episode of syncope associated with hypoglycemia. The patient underwent Doppler echocardiography and carotid artery ultrasound which showed mild, non-significant carotid artery stenosis. Insulin levels were within normal ranges (29 uU/mL). He was evaluated by psychiatrists who made the diagnosis of a neuropsychiatric disorder and was medicated with levetiracetam 1000 mg/day.
Fourteen months later, he presented a new episode of syncope while working and was transferred to the emergency department of Hospital José F. de San Martín. On admission, as his blood glucose level was 27 mg/dL, he was admitted to the internal medicine ward.
The laboratory tests showed hypoglycemia between 35 and 51 mg/dL in the morning (6 am to 8 am) with a trend toward normalization after meals and normal values during the rest of the day.
During an episode of hypoglycemia of 37 mg/ dL, the baseline insulin level was 59 uU/mL. Other laboratory tests included C-peptide of 6.3 ng/dL (reference values 1.1-5.0), ACTH of 35 pg/mL (reference values 9-46), and morning cortisol levels of 16 μg/dL (reference values 5-25).
A computed tomography (CT) scan of the abdomen and pelvis did not show relevant abnormalities. The magnetic resonance imaging (MRI) revealed a rounded 15-mm image in the head of the pancreas, slightly heterogeneous on T2 sequence and hyperintense on T1 sequence with homogeneous enhancement after the administration of intravenous contrast agent, consistent with an insulinoma (Fig. 1).
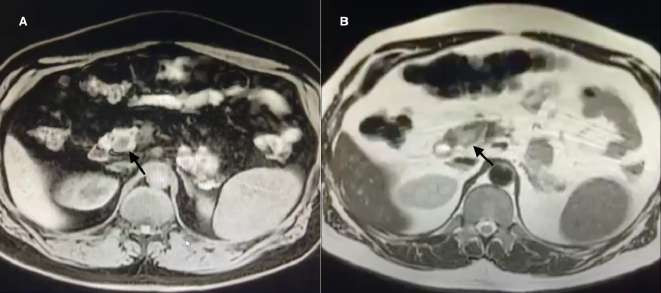
FIGURE 1 Magnetic resonance imaging with gadolinium-based contrast agent. Arrow: insulinoma. A: Axial section. Hypointense nodular image on T1-weighted fat suppressed images. B: Axial section. Hyperintense nodular image on T2 sequence.
He was evaluated by the department of hepatobiliary and pancreatic surgery, who decided surgical management, either laparoscopic enucleation vs. CPD. The procedure started with the patient placed in the Lloyd Davies position, in reverse Trendelenburg at a 45-degree tilt in left semi-lateral decubitus. The surgeon stood between both patient’s legs, the first assistant on the surgeon’s right and the second assistant on his/her left. The closed technique was used for creating pneumoperitoneum set at a pressure of 12 mm Hg. Laparocopic exploration was performed through an umbilical trocar. The peritoneum and the other organs had no lesions. Two 5-mm trocars were inserted in the epigastrium and right hypochondriac region in the mid-clavicular line, and one 10-mm trocar was inserted in the left hypochondriac region and midclavicular line. After performing the Vautrin-Kocher maneuver, the omentum was divided using LigaSure™ sealing device and the omental bursa was explored. An intraoperative ultrasound of the entire pancreas was performed through a small subcostal incision. The examination revealed a single 2-cm lesion in the head of the pancreas in contact with the main pancreatic duct. As enucleation was not possible, conversion to open surgery was decided to perform CDP. Laparotomy was performed with an extended right subcostal incision. The gastrocolic ligament was released and the right gastroepiploic vessels were identified and dissected. The bile duct was dissected, a tape was placed as hallmark, and the gastroduodenal artery (GAD) was identified. After the superior mesenteric vein (SMV) was identified, blunt dissection of the pancreatic neck was performed from the posterior surface to the superior edge. Then, the GDA was ligated and sectioned; CPD was completed with pylorus preservation, resection of the surgical specimen, Roux-en-Y reconstruction in a trans-mesocolonic loop, pancreaticojejunostomy with duct-to-mucosa anastomosis using Prolene® 6-0, hepaticojejunostomy with Prolene® 5-0 and gastrojejunostomy with Prolene® 3-0. Two drains were placed, one posteriorly and another anteriorly at the biliary anastomosis and pancreatic anastomosis.
The patient was admitted to the intensive care unit alert and extubated, with an epidural catheter for analgesia control. Sixteen hours later he was transferred to the general ward. Oral feeding was started at 48 hours. On postoperative day 3, a small biliary fistula was noted, which was completely drained by the tube placed posterior to the anastomosis. On postoperative day 4 the patient presented fever, dyspnea and desaturation. A CT scan of the thorax and abdomen only revealed bilateral pneumonia. Blood cultures were collected and treatment with piperacillin-tazobactam 4.5 g every 6 hours was indicated for 14 days. The anterior drain tube was removed on postoperative day 10 after 48 hours without drainage output. The patient was discharged once antibiotic treatment ended. The posterior drain was removed on postoperative day 24 due to absence of drainage output. The pathology examination reported the presence of a well-differentiated insulinoma of 1.5 cm in size with a minimal resection margin of 2 cm (Fig. 2). The symptoms disappeared completely, and the results of the laboratory tests remained normal for 4 months after surgery.
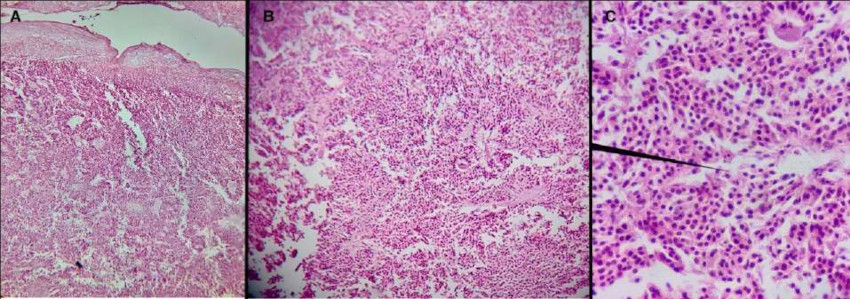
FIGURE 2 Insulinoma. Microspcopic examination (Magnification A: 4×; B: 10×; C: 40×). Section stained with hematoxylin and eosin. Small cells with uniform and cuboidal nuclei, granular eosinophilic cytoplasm in a solid and trabecular pattern and deposits of amyloid.
The presence of the Whipple triad (hypoglycemia, neuroglycopenic symptoms, and symptomatic relief after glucose administration) leads to the diagnosis of endogenous hyperinsulinism. The results of laboratory tests including low blood glucose, elevated levels of insulin, proinsulin, and C-peptide will help to approach the diagnosis of insulinoma, and imaging methods will confirm the diagnosis and localization of the tumor3.
These tumors usually present with neuroglycopenic symptoms such as confusion, amnesia, visual impairment and seizures that may be misdiagnosed as epilepsy, even on the basis of electroencephalographic and imaging features. Misdiagnosis delays treatment and increases the risk of permanent neurological deficits and even coma followed by death.
The diagnosis of insulinoma requires a high level of suspicion and is usually delayed because symptoms are usually avoided with frequent ingestion. Boukhman et al. reported that the duration of symptoms before diagnosis in a series of 60 patients ranged from one hour in a newborn to 34 years (mean 3.8 years). During this period, at least six patients had been under psychiatric treatment4.
In 1929, Roscoe Graham reported a major pancreatic surgery with subsequent cure5. Conservative surgery has gradually become the treatment of choice by reducing the risk of diabetes mellitus, complicated fistulas and reoperation, as well as length of hospital stay and mortality2,6.
We report the case of a patient with a delayed diagnosis of insulinoma, confirmed by MRI, 14 months after the onset of symptoms, which was treated as a neuropsychiatric disorder. After the correct diagnosis was made, the patient underwent major pancreatic resection with complete resolution of symptoms.
Referencias bibliográficas /References
1. Rostambeigi N, Thompson GB. What should be done in an operating room when an insulinoma cannot be found? Clin Endocrinol (Oxf). 2009;70(4):512-5. [ Links ]
2. Grant CS. Insulinoma. Best Pract Res Clin Gastroenterol. 2005;19(5):783-98. [ Links ]
3. Mehrabi A, Fischer L, Hafezi M, Dirlewanger A, Grenacher L, Diener MK, et al. A systematic review of localization, surgical treatment options, and outcome of insulinoma. Pancreas. 2014;43(5):675-86. [ Links ]
4. Boukhman MP, Karam JH, Shaver J, Siperstein AE, Duh QY, Clark OH. Insulinoma-experience from 1950 to 1995. West J Med. 1998;169(2):98-104. [ Links ]
5. Howland G, Compbell WR, Maltby EJ, Robinson WL. Dysinsulinism: Convulsions and, due to islet cell tumor of the pancreas, with operation and cure. JAMA. 1929; 93:674. [ Links ]
6. Hackert T, Hinz U, Fritz S, Strobel O, Schneider L, Hartwig W, et al. Enucleation in pancreatic surgery: indications, technique, and outcome compared to standard pancreatic resections. Langenbecks Arch Surg. 2011; 396:1197-203. [ Links ]
Received: April 25, 2023; Accepted: June 22, 2023











 texto en
texto en 



