Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista argentina de cirugía
versión impresa ISSN 2250-639Xversión On-line ISSN 2250-639X
Rev. argent. cir. vol.116 no.2 Cap. Fed. jun. 2024 Epub 01-Jun-2024
http://dx.doi.org/10.25132/raac.v116.n2.1768
Scientific letter
Liver resection in monolobar Caroli’s disease
1Unidad de Cirugía Hepatobiliar Compleja, Pancreática y Trasplante Hepático. Hospital de Alta Complejidad El Cruce. Buenos Aires. Argentina
Caroli’s disease is a congenital disorder caused by a defect of the ductal plate. The clinical picture includes intrahepatic duct lithiasis and recurrent cholangitis usually in young people. The imaging tests reveal the presence of multifocal and segmental dilatation of the intrahepatic bile ducts. Cholangiocarcinoma can develop as a long-term complication of chronic bile duct inflammation and should always be considered as a differential diagnosis. We describe a rare case of a 52-year-old woman who presented with bile duct obstruction after laparoscopic cholecystectomy and required resection of liver segments II and III due to Caroli’s disease with a favorable outcome.
Keywords: liver; Caroli disease; liver resection
Caroli’s disease is a rare congenital disorder caused by a defect of the ductal plate. The estimated incidence of Caroli’s disease is 1 in 1 000 000 population and most cases occur in persons < 30 years1. It is characterized by multifocal segmental saccular dilatation of the intrahepatic bile ducts, involving the entire liver, a lobe or a single segment2. This results in biliary ectasia, which increases the likelihood of developing intrahepatic duct lithiasis and recurrent cholangitis, the most common form of the disease3. Two types have been described: pure Caroli’s disease and Caroli’s syndrome, which is associated with congenital hepatic fibrosis and has long-term manifestations secondary to portal hypertension1. Magnetic resonance cholangiopancreatography is the recommended diagnostic tool for the diagnosis of this condition, which shows dilatation of the intrahepatic bile ducts in communication with the main biliary tree4. Cholangiocarcinoma is a differential diagnosis and can develop as a long-term complication of chronic bile duct inflammation3,4. Treatment must be individualized and ranges from conservative management to surgery and liver transplantation.
We report the case of a 52-year-old female patient with a history of significant tobacco use and chronic obstructive pulmonary disease (COPD) who was referred to out center two months after undergoing laparoscopic cholecystectomy. Before surgery, she had presented jaundice, choluria and acholia. The surgical team reported that during the procedure they discovered a main bile duct stricture likely caused by a tumor, so they placed a left-sided internal-external percutaneous biliary drainage catheter. During history taking, the patient reported unspecific and abdominal discomfort from time to time. On physical examination, the performance status was good and she presented jaundice and scleral icterus. The percutaneous drainage was patent and draining bile. The laboratory tests indicated the following results: alkaline phosphatase of 587 IU/L, aspartate aminotransferase of 120 IU/L, alanine aminotransferase of 87 IU/L, total bilirubin of 8.13 mg/dL with direct bilirubin predominance, and tumor markers within normal values. The patient underwent multislice computed tomography of the chest, abdomen, and pelvis, and magnetic resonance cholangiopancreatography, which revealed stricture of the common hepatic duct and left hepatic duct; the left intrahepatic bile duct was dilated (Fig. 1a, black arrow) and there was atrophy of the corresponding parenchyma (Fig. 1b, black arrowhead). The right hepatic duct was normal. A diagnosis of possible perihilar cholangiocarcinoma was made and surgery was decided using a conventional approach.
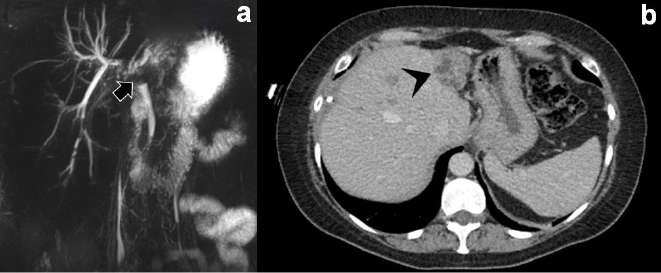
FIGURE 1 A: Magnetic resonance cholangiopancreatography showing stricture of the common hepatic duct and left hepatic duct. B: Computed tomography section showing atrophy of the left liver lobe.
A supra-umbilical midline incision was made and extended transversely to the right. On surgical exploration there was a significant atrophy of liver segments II and III and were therefore resected (Fig. 2a, white arrow). The intraoperative cholangiogram evidenced multiple stones in the right biliary tree (Fig. 2b, white arrowhead) that had not been identified previously and could be due to prolonged biliary ectasia. The common bile duct was explored via choledochotomy, and the stones were removed using Dormia baskets and flushing. The common bile duct was closed by primary suture. The patient evolved with favorable outcome and was discharged on postoperative day 5. The pathology report described absence of neoplasm, saccular dilatation of the bile ducts surrounded by mononuclear cell infiltration and peribiliary connective tissue, consistent with Caroli’s disease. The patient is still monitored on an outpatient basis. One and a half years after the procedure she is asymptomatic with no changes in the laboratory parameters or imaging tests.
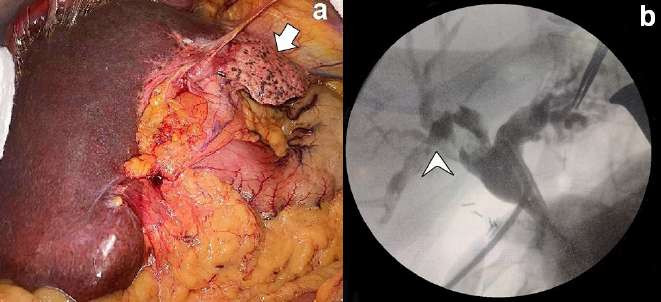
FIGURE 2 A: Surgical exploration with significant atrophy of liver segments II and III. B: Intraoperative cholangiogram with negative images in the right biliary tree suggestive of lithiasis
Our case highlights the importance of high index of suspicion in clinical practice. We believe that the difficulty in diagnosing this disease lies in several aspects. First, the unusual age of onset of the disease, which usually occurs in young people1. Second, at the time of diagnosis, patients have already had several episodes of recurrent cholangitis, whereas the course of the disease was indolent for many years in our patient. Third, the intraoperative findings do not align with those of magnetic resonance cholangiopancreatography, which did not clearly indicate multiple cholelithiasis as the cause of obstruction. Finally, the prolonged bile duct obstruction resulted in significant left lobar atrophy, which made it challenging to interpret the computed tomography scan images. This made it difficult to clearly distinguish the typical pattern of saccular dilatation in the intrahepatic bile duct. The atrophy-hypertrophy complex has been extensively studied and refers to the restorative hyperplasia in response to a liver disease that causes segmental liver atrophy. It may be due to different types of injury (toxins, ischemia, and partial hepatectomy) or occur by liver injury that impedes bile flow and portal venous inflow and outflow. This is a common finding in neoplasms with ipsilateral vascular involvement5 and was our first diagnosis. Yet, atrophy was caused by bile duct obstruction. Moreover, in retrospect, we think that the degree of atrophy observed necessarily implied a long-time course, more consistent with a benign condition.
The treatment of Caroli’s disease should be tailored to the type of presentation and associated complications. Ursodeoxycholic acid is used to prevent gallstone formation. Endoscopic and percutaneous approaches may be useful for treating cholangitis due to intraductal obstruction and liver abscesses3. In symptomatic cases where conservative management has been unsuccessful or intrahepatic duct lithiasis is present, hepatectomy offers excellent results. Finally, in cases of diffuse involvement with recurrent episodes of cholangitis that are difficult to control or complications secondary to portal hypertension, liver transplantation is indicated6. While the treatment plan was appropriate and the patient’s outcome was favorable, we believe that less common differential diagnoses should be considered before planning surgical treatment. We hope that this case will serve to raise awareness of Caroli’s disease and that it will be considered when evaluating a patient with cholangitis.
Referencias bibliográficas /References
1. Yonem O, Bayraktar Y. Clinical characteristics of Caroli's disease. World J Gastroenterol. 2007; 13:1930-3. [ Links ]
2. Wang Z-X, Li Y-G, Wang R-L, Li YW, Li ZY, Wang LF, et al. Clinical classification of Caroli's disease: an analysis of 30 patients. HPB. 2015; 17:278-83. [ Links ]
3. Menon S, Holt A. Large-duct cholangiopathies: aetiology, diagnosis and treatment. Frontline Gastroenterol. 2019; 10:284-91. [ Links ]
4. Cannella R, Giambelluca D, Diamarco M, Caruana G, Cutaia G, Midiri M, et al. Congenital Cystic Lesions of the Bile Ducts: Imaging-Based Diagnosis. Curr Probl Diagn Radiol. 2020;49:285-93. [ Links ]
5. Kim RD, Kim JS, Watanabe G, Mohuczy D, Behrns KE. Liver regeneration and the atrophy-hypertrophy complex. Semin Intervent Radiol. 2008;25:92-103. [ Links ]
6. Mabrut J-Y, Kianmanesh R, Nuzzo G, Castaing D, Boudjema K, Létoublon C, et al. Surgical management of congenital intrahepatic bile duct dilatation, Caroli's disease and syndrome: long-term results of the French Association of Surgery Multicenter Study. Ann Surg. 2013;258:713-21; discussion 721. [ Links ]
Received: August 14, 2023; Accepted: February 20, 2024











 texto en
texto en 



