Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista argentina de cirugía
versión impresa ISSN 2250-639Xversión On-line ISSN 2250-639X
Rev. argent. cir. vol.116 no.2 Cap. Fed. jun. 2024 Epub 01-Jun-2024
http://dx.doi.org/10.25132/raac.v116.n2.1742
Scientific letter
Isolated splenic hydatid disease
1Servicio de Cirugía General Hospital Cosme Argerich. Ciudad de Buenos Aires. Argentina
Hydatid disease is an endemic parasitosis in Argentina. The liver and lungs are the organs more commonly affected, but isolated splenic involvement is rare. The aim of this study is to report two cases of isolated splenic hydatid disease. The diagnosis was suspected by epidemiology and imaging tests. The serologic tests were negative in both cases. Surgical management was decided and both patients underwent laparoscopic total splenectomy. This disease should be suspected in endemic areas in the presence of splenic cysts despite negative serologic tests. Total splenectomy prevents local recurrence and complications associated with the residual cavity. The laparoscopic approach is preferred as it results in a shorter length of hospital stay and fewer abdominal wall complications.
Keywords: hydatid cyst; splenectomy; laparoscopy
Hydatid disease is an endemic parasitosis in Argentina. Humans are infected through ingestion of parasite eggs in contaminated food. In the organism, the disease is caused by the larval stage of Echinococcus granulosus which predominantly develops in the liver (50-80%) and lungs (25%). Splenic involvement is seen in endemic areas and accounts for 50-80% of all splenic cysts. Primary extrahepatic hydatid cysts are rare, and among these, isolated splenic hydatid disease account for 2 to 3.5%1.
The aim of this study is to report two cases of isolated splenic hydatid disease.
Case 1
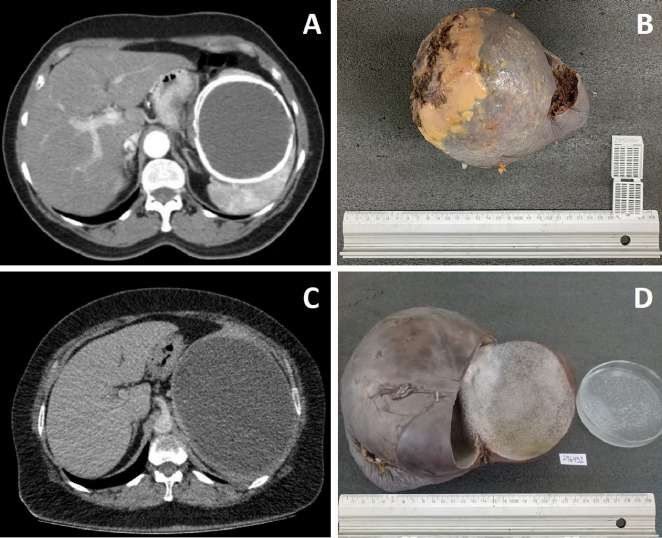
A 60-year-old female patient with a body mass index (BMI) of 35 kg/m2 who lived in a rural area sought medical advice due to abdominal pain in the left hypochondriac region associated with vomiting and weight loss (11 kg within a month). The abdominal ultrasound showed a 15-mm rounded hypoechoic image (Gharbi type V). The computed tomography (CT) scan of the abdomen with intravenous contrast agent revealed the presence of a calcified cyst in contact with the diaphragm and stomach (Fig. 1A). Serologic tests were performed by ELISA and Western blot technique and the results were negative for hydatid disease. Surgical management was decided, and the patient underwent laparoscopic splenectomy. She evolved with favorable outcome and was discharged on postoperative day 3. The pathological examination reported a 15×13×11 cm mass weighing 895 grams with findings consistent with hydatid cyst (Fig. 1B).
Case 2
A 41-year-old female patient with a body mass index (BMI) of 37 kg/m2 who lived in a rural sought medical advice due to pain in the left hypochondriac region. The ultrasound showed a splenic cyst with a size of 20×16 cm (Gharbi type 1). The patient underwent a CT scan of the abdomen (Fig. 1C) and serologic tests by ELISA and Western blot techniques which were negative for hydatid disease. Surgical management was decided, and the patient underwent laparoscopic splenectomy. She evolved with favorable outcome and was discharged on postoperative day 4. The pathological examination reported a 20×16×10 cm mass weighing 2410 grams with morphologic and histopathologic findings consistent with hydatid cyst with presence of viable microorganisms (Fig. 1D).
Both patients received the same treatment in their different stages. Perioperative treatment consisted of vaccination against encapsulated bacteria and treatment with albenzadole at a dose of 15 mg/ kg/day for 30 days prior to surgery and 90 days after surgery. Both patients underwent laparoscopic total splenectomy via an anterior approach in the right lateral decubitus position, with hemostatic control of the short vessels with a harmonic scalpel and of the splenic hilum with hemostatic (Hem-o-lok®) clips. A scolicidal solution was prepared in case a cystic rupture occurred, and total splenectomy was performed without rupture. The specimen was extracted through a Pfannestiel incision with protection of the operative field with hypertonic saline at 20%. Both patients completed the postoperative antiparasitic treatment for 3 months. There were no complications or recurrences after a follow-up period of 20 and 36 weeks in each case.
Spleen involvement in hydatid disease without hepatic or pulmonary cysts is exceptional and nonspecific. However, it should be considered as a differential diagnosis in endemic areas when splenic cysts are present (Table 1).
TABLE 1 Classification of non-parasitic splenic cysts
| Congenital | Epithelial lining. Epidermoid lining. Mesothelial lining. Lack of demonstrable cellular lining |
| Neoplastic | Neoplasms of endothelial origin Lymphangioma Hemangioma Cystified primary or metastatic tumors |
| Traumatic | With documented history of trauma. Secondary to subcapsular hematoma. |
| Necrotic | After spleen infection: history of endocarditis, typhoid fever, generalized lymphadenopathy due to infection, infectious mononucleosis, etc. |
| Degenerative | Cystified splenic infarcts |
From Morgenstern L. Nonparasitic splenic cysts: Pathogenesis, classification, and treatment. J Am Coll Surg. 2002; 194:306-14.
The first case of splenic hydatid cyst was reported by Berlot in 1790 as an autopsy finding. Sabadini presented the first cumulative report in 1991 with a literature review of 300 cases1.
Diagnosis is based on epidemiology and imaging tests because the clinical presentation is nonspecific and serologic tests have a high false negative rate. In our patients, the diagnosis was made by the epidemiologic history and imaging tests and was confirmed by pathological examination.
Work-up begins with ultrasound because of its low cost and high sensitivity and specificity (100% and 97%, respectively)2. The specificity of ultrasound in the diagnosis of splenic hydatid disease is three times higher than that of serology2. Another useful feature is the ability to classify cysts according to the Gharbi classification3.
Computed tomography provides additional information about the structure of the cyst, such as calcification or signs of complications (bleeding and infection). It also demonstrates the relationship between the cyst and the blood vessels and adjacent organs and can help in differentiating it from other lesions such as epidermoid cysts, splenic abscesses, and cystic neoplasms of the spleen2.
The serologic tests were negative in both patients. However, this does not exclude the diagnosis because, as Mejri et al.4 had described, serology can be negative in up to 62.5% of isolated splenic localizations, even with viable microorganisms as in our case 2.
Drug treatment is performed with antiparasitic drugs (albendazole) in asymptomatic patients, as preoperative prophylaxis, or in patients with contraindications to surgery. Preoperative treatment is given in doses of 10-15 mg/kg/day for 30 days and 90 days postoperatively5. In the case of a ruptured cyst with peritoneal spread, the dose is 15 mg/kg/day every 12 hours5.
The surgical treatment plan dpends on several factors, including the patient’s age and performance status, location, size and number of cysts, percentage of residual splenic parenchyma and comorbidities. Options include percutaneous drainage, unroofing with omentoplasty, and conservative or radical splenectomy.
The advantages of percutaneous drainage and unroofing with omentoplasty are that they are minimally invasive but expose the patient to the risk of recurrence and possible abscess formation in the residual cavity. Some authors have also indicated that these techniques could result in an increased length of hospital stay4.
Partial splenectomy and enucleation are associated with high risk of bleeding6. Therefore, these procedures should only be considered in selected cases, such as patients with significant comorbidities, small cysts, or in the pediatric population in whom spleen preservation should be attempted.
In our study, both cysts were larger than 15 cm and occupied more than 75% of the splenic parenchyma. Therefore, total splenectomy was considered the most appropriate option. This procedure avoids complications related to the residual cavity such as reinfection, is technically simpler, has lower risk of bleeding, and recurrence is rare.
Some authors recommend conventional surgery for large cysts due to the potential difficulty in mobilizing and releasing adjacent structures. In our opinion, laparoscopy is useful because once hemostatic control of the splenic pedicle is achieved, splenectomy is usually safe. This approach allows for improved postoperative recovery, earlier return to work and fewer abdominal wall complications.
Isolated splenic hydatid cyst is uncommon but should be considered in the initial work-up of splenic cystic lesions, especially in endemic areas. The diagnosis is suspected by epidemiology and imaging tests. Negative serologic tests should not exclude the diagnosis because of the high rate of false negative results. The diagnosis is confirmed by the pathological examination. Laparoscopic total splenectomy is the recommended approach, even in cases of large spleens, as it offers a low risk of morbidity, mortality and recurrence.
Acknowledgments
We appreciate the collaboration of Leandro M. Danze, of the Pathological Anatomy Service
REFERENCES
1. Prieto M, Marquina T, Mifsut P, Moreno T. Hidatidosis esplénica: 5 casos de esta rara localización. Enferm Infec Micr Cl. 2011;29(8):634-5. https://doi.org/10.1016/j.eimc.2011.04.003 [ Links ]
2. Tévez-Craise L, Daiana-Vaccaro R, De Luca PA, Vásquez-Guillén ME, Calaramo OA, Logioco F. Hidatidosis: Clasificación clínica-imagenológica según Gharbi y la Organización Mundial de la Salud. Rev Argent Radiol. 2022;86(1). https://doi.org/10.24875/rar.m22000010 [ Links ]
3. Gharbi HA, Hassine W, Brauner, M. W., Dupuch, K. Ultrasound examination of the hydatic liver. Radiology. 1981;139(2):459-63. https://doi.org/10.1148/radiology.139.2.7220891 [ Links ]
4. Mejri A, Arfaoui K, Ayadi MF, Aloui B, Yaakoubi J. Primitive isolated hydatid cyst of the spleen: total splenectomy versus spleen saving surgical modalities. BMC Surgery. 2021; 21(1), 46. https://doi. org/10.1186/s12893-020-01036-8 [ Links ]
5. Guía para el equipo de salud N.o 11: Enfermedades Infecciosas-Hidatidosis. (2012). Ministerio de Salud. ISSN 1852-1819 / en línea: ISSN 1852-219X https://bancos.salud.gob.ar/sites/default/files/2018-10/0000000797cnt-2012-03-29_hidatidosis-guia-medica.pdf [ Links ]
6. Cai H, An Y, Wu D, Chen X, Zhang Y, Zhu F, et al. Laparoscopic partial splenectomy: A preferred method for select patients. J Laparoendosc Adv Surg Tech A. 2016;26(12): 1010-4. https://doi.org/10.1089/lap.2016.0150 [ Links ]
Received: March 06, 2023; Accepted: May 03, 2023











 texto en
texto en