Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista argentina de cirugía
versión impresa ISSN 2250-639Xversión On-line ISSN 2250-639X
Rev. argent. cir. vol.116 no.2 Cap. Fed. jun. 2024 Epub 01-Jun-2024
http://dx.doi.org/10.25132/raac.v116.n2.1561
Scientific letter
Nodular fasciitis as cause of lateral neck tumor
1Práctica privada Sanatorio Otamendi Buenos Aires. Argentina.
Nodular fasciitis is a rare and benign neoplasm of the soft tissues that can occur in any region of the body and require surgical treatment. We report the case of a 41-year-old female patient with a lateral neck tumor which reached a size of 74.7 × 32.5 mm after two years. The tumor was completely removed under general anesthesia. The pathological examination reported proliferation of myofibroblasts, suggestive of nodular fasciitis. The patient evolved homolateral Claude Bernard Syndrome, without local complications and mild weakness of the ipsilateral arm which improved after 60 days with kinesiotherapy. This condition should be considered among the differential diagnoses of lateral neck tumors.
Keywords: fasciitis nodular; neck tumor; soft tissue neoplasia
Nodular fasciitis is a benign and rare condition that was first described by Knowaler et al. in 1955 as subcutaneous pseudosarcomatous fibromatosis1.
Later, in 1966, Mehrengan proposed the term nodular fasciitis and presented a series of 17 patients2.
It has a ubiquitous distribution, as has been demonstrated by many publications3, 4, 5, 6 and occurs 7-20% in the head and neck region3. The incidence of nodular fasciitis is low as it accounts for 0.025% of all pathology diagnoses1; nevertheless, it should be considered in the differential diagnosis in the region, as the diagnostic and therapeutic approach is different from other head and neck conditions. For this reason, the authors believe it appropriate to report a case to raise awareness of this condition.
A 41-year-old woman, with no history of trauma, sought medical care for discomfort while swallowing over the past two years. After undergoing several tests, she was diagnosed with a right lateral neck tumor. On May 9, 2018, she was operated on by other surgeons. The lymph nodes were resected; the pathology report was reactive lymph nodes, but the biopsy was inadequate as it did not correspond to lymph nodes of the lesion but to regional lymph nodes that were not affected. There was no documentation of other complementary tests of the material obtained.
As discomfort persisted and the tumor grew progressively, she underwent new tests.
A neck ultrasound performed on September 27, 2019, revealed a solid avascular mass with a size of 38 × 27 × 26 mm in the right lateral neck region.
A contrast-enhanced computed tomography scan performed on October 16th showed a solid mass with a size of 74.7 × 32.5 mm between C2 and C7 in the right prevertebral space with forward displacement of the vascular bundle and thyroid gland (Fig. 1 A and B). On computed tomography angiography the carotid vessels were displaced without intrinsic involvement (Fig. 1C).
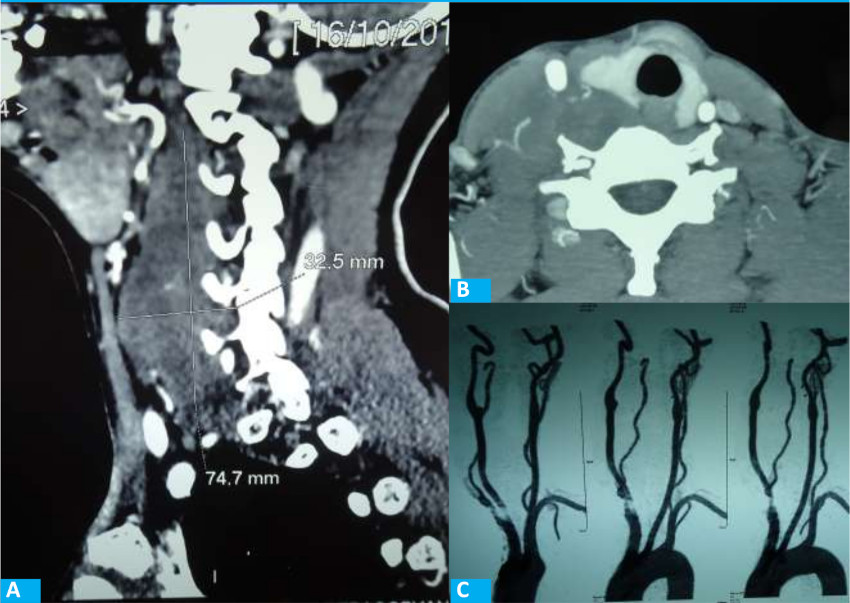
FIGURE 1 A: Tomografía computarizada (TC), corte sagital, en la que se observa un tumor pre-vertebral que desplaza el paquete vascular hacia adelante. B:TC, corte transversal, en la que se observa el desplazamiento de la tiroides y del paquete vascular. C: Angiotomografía de vasos de cuello, en la que se observa el desplazamiento de los vasos carotídeos derechos hacia afuera y adelante, sin patología intrínseca.
An ultrasound-guided fine needle aspiration biopsy was performed on November 19, 2019. The cytology revealed the presence of spindle-shaped cells with oval nuclei and pale cytoplasm, bur a definite diagnosis was not made. The pathologist reported that the mesenchymal lesions produced few cells.
With a presumptive diagnosis of neurogenic tumor, possibly originating from the sympathetic chain due to its prevertebral location, she underwent surgery under general anesthesia on January 17, 2020. The procedure was performed via an oblique anterior presternocleidomastoid cervicotomy. A hard tumor with the same size as indicated by the preoperative imaging studies was found fixed to the deep planes behind the vascular bundle of the neck.
After performing a complex dissection, the entire lesion was removed; it was attached to the prevertebral muscles, which were excised in continuity, with the internal jugular vein and the cervical sympathetic chain. The hypoglossal nerve, vagus nerve, spinal nerve, phrenic nerve, and brachial plexus were identified and preserved.
Intraoperative frozen section examination was not performed because the preoperative diagnosis was a benign lesion.
The patient developed postoperative Claude Bernard-Horner syndrome and right brachial paresis, which improved after 60 days with kinesiotherapy. There were no complications in the surgical site.
The pathological examination showed proliferation of myofibroblasts in tissue culture with extensive erythrocyte extravasation and low mitotic count, with dense collagen tissue. The resection margins were free. Immunohistochemical staining showed positive staining for vimentin and actin, negative for the S-100 protein and Ki-67 proliferative index of 2%; thus, the diagnosis of nodular fasciitis was made (Fig. 2).
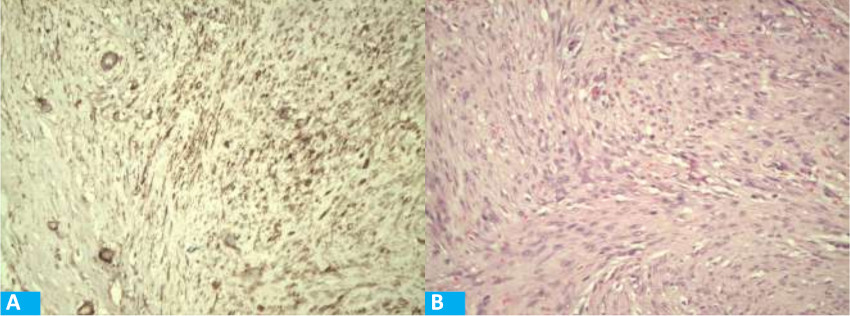
FIGURE 2 A: HE 200X Proliferación fusocelular miofibroblástica, con extravasación eritrocitaria.B: Tinción positiva con inmunohistoquímica para actina músculo liso 200X.
Nodular fasciitis presents as a single tumor in young adults (20 to 40 years), with similar distribution between males and females. The etiology remains unknown but has been related with a history of trauma or inflammatory processes3.
Different variants have been described according to their origin: subcutaneous, intramuscular or fascial6.
Due to its origin in soft tissues and its rapid growth, it can cause symptoms of compression and can be mistaken for sarcomas. The differential diagnosis with lymph node metastases or lymphomas should be made in nodular fasciitis of the neck. Other diagnoses to consider are some benign tumors of the connective tissue (as fibromas or desmoid tumor) and neurogenic tumors, as in the case presented here (7,8) .
Fine-needle aspiration biopsies are usually inconclusive, and there is no imaging pattern to confirm the diagnosis5,6. Although spontaneous remission has been described, the recommended treatment in cases of rapid growth is wide resection, since it can produce symptoms due to compression of the airway and gastrointestinal tract (7,8) .
With this treatment, local recurrences are very rare. As with other low prevalence diseases, most publications correspond to case reports. Lu et al. presented a series of 272 cases between 2004 and 2014, with different ages and from different locations, so it is difficult to draw conclusions about particular situations4. In conclusion, nodular fasciitis is a rare, benign condition that requires surgical treatment and can mimic the clinical presentation of other benign and malignant tumors, so it should be considered among the possible differential diagnoses of a lateral neck tumor.
Referencias bibliográficas /References
1. Borumandi F, Cascarini L, Mallawaarachchi R, Sandison A. The chameleon in the neck: Nodular fasciitis mimicking malignant neck mass of unknown primary. Int J Surg Case Rep. 2012; 3(10):501-3. [ Links ]
2. Almeida F, Picón M, Pezzi M, Sánchez-Jáuregui E, Carrillo R, Martínez-Lage JL. Rev Esp Cir Oral y Maxilofac. 2007; 29(1):43-7. [ Links ]
3. Khanna V, Rajan M, Reddy T, Alexander N, Surendran P. Nodular fasciitis mimicking a soft tissue sarcoma - A case report. Int J Surg Case Rep. 2018; 44: 29-32. [ Links ]
4. Lu L, Lao IW, Liu X, Yu L, Wang J. Nodular fasciitis: a retrospective study of 272 cases from China with clinicopathologic and radiologic correlation. Ann Diagn Pathol. 2015; 19(3):180-5. [ Links ]
5. Çelik SY, Dere Y, Çelik O¨I, Derin S, Sahan M, Dere O¨. Nodular fasciitis of the neck causing emergency: a case report. Oman Med J. 2017; 32(1): 69-72. [ Links ]
6. Gamboa-López VR, Soto-Becerril O, Abrahm-Zúñiga L, RamírezRamírez A. Fascitis nodular cervical, una causa poco frecuente de masa en el cuello. Rev Hosp Jua Mex. 2018; 85(4):238-40. [ Links ]
Received: April 10, 2022; Accepted: July 25, 2022











 texto en
texto en 



