Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista argentina de cirugía
versión impresa ISSN 2250-639Xversión On-line ISSN 2250-639X
Rev. argent. cir. vol.113 no.2 Cap. Fed. jun. 2021
http://dx.doi.org/10.25132/raac.v113.n2.1608.ei
Articles
Impact of the COVID-19 pandemic on the presentation of surgical conditions. Experience of Hospital de Clínicas in Uruguay
1 Departamento de Emergencia del Hospital de Clínicas, Facultad de Medicina. Universidad de la República. Uruguay
Introduction
COVID-19 (coronavirus disease 2019) was declared a global health emergency by WHO on March 11, 2020. On March 13, 2020, Uruguay declared the health emergency with the first imported cases.
As a result of the pandemic, patients’ visits to the emergency department were affected by the lockdown and social isolation, resulting in delays in seeking medical care. This is reflected by the complications associated with the course of the disease and secondary to treatment.
Standards for personal protection of the healthcare staff and healthcare protocols were established. Elective surgeries were postponed, and only oncologic emergency and urgent procedures were performed after swab testing. All the patients undergoing surgery with a PCR test positive for SARS-CoV-2 or who waiting for the test result (without or without symptoms or known close contact) were treated under the protocol for COVID-19 patients.
Objectives
▪▪To evaluate the stage of the conditions requiring emergency surgery at the moment of consultation in the context of the COVID-19 pandemic.
▪▪To analyze postoperative morbidity and mortality in the context of the pandemic.
▪▪To analyze if there were changes in the selection of the surgical approach based on the risk of transmission in the surgical area.
Material and methods
We conducted a single-center, retrospective and observational cohort study based on the information retrieved from the electronic record of the urgent and emergency procedures performed in the surgical area of Hospital de Clínicas.
Two study groups were generated to compare two populations over the same time interval but differentiated by the presence of the COVID-19 pandemic and its influence. The control group (group A) was made up of those patients undergoing urgent/ emergency surgery between March 13 and December 12, 2019, while group B was made up of patients operated on over the same time interval in 2020.
We established inclusion and exclusion criteria to evaluate both populations and assess if they were statistically comparable.
Inclusion criteria:
▪▪Age > 18 years.
▪▪Admitted to the emergency department.
▪▪Condition requiring urgent/emergency surgery.
▪▪Operated on by the staff of general surgery.
Exclusion criteria:
▪▪Elective procedures performed at the emergency department.
▪▪Surgical biopsies due to oncological emergencies.
The following data were recorded: age, diagnosis (on admission, intraoperative findings, disease stage or associated complications) and surgical approach (laparoscopy or laparotomy).
Laboratory and imaging tests were ordered according to the clinical diagnosis. Ultrasound and computed tomography scan were indicated following the institutional recommendations.
The surgical approach was decided by the surgeon on duty.
The intraoperative findings about the stage of the disease and its complications were duly recorded in the operative record of the institution which provided the information for this study.
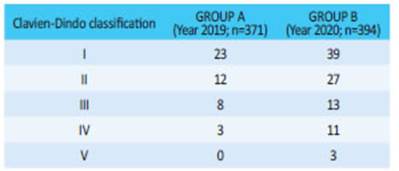
The presence of postoperative complications, defined as any deviation from the normal postoperative course, was considered. Postoperative complications were categorized using the Clavien-Dindo classification which is based in objective data depending on the treatment required. Categories I and II are mild complications, III-IV are serious complications and V corresponds to death.
Statistical and bivariate analysis
All the statistical procedures were performed using PSPP® and Epidat 4.1® software packages using frequency distribution and summary measures. The normality of variables was evaluated using the Kolmogorov-Smirnov test. Both groups were compared with the Student’s test and t test for the difference between means.
The Pearson’s chi square test with Yates’ correction or Fisher’s exact test were used depending on the distribution of the sample.
A p value < 0.05 was considered statistically significant.
Results
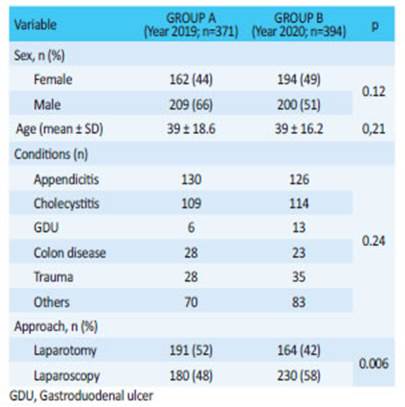
The cohort was made up of 765 patients, 371 in group A (2019) and 394 in group B (2020).
The demographic data are shown in Table 1. There were no significant differences in the variables (p > 0.05) except for the surgical approach, which will be discussed later.
The surgical diagnoses included acute appendicitis, cholecystitis, trauma (polytrauma and penetrating trauma due to stab wound or gunshot) complicated peptic ulcer disease (PUD) and other conditions (benign anal disease, perianal or buttock abscesses or other abscesses).
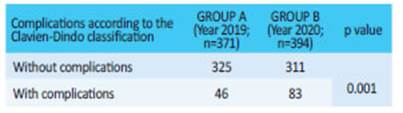
According to the intraoperative findings, results of the imaging tests and clinical diagnosis on admission, 10.5% of the cases in group A and 21.1% in group B presented complications associated with progression of the disease (p = 0.0001) (Table 2).
The complications according to the Clavien- Dindo classification are shown in Tables 3 and 4. A p value of 0.001 was observed for the presence or absence of postoperative morbidity and mortality. Three patients in group B died.
When the surgical approach used was compared, the laparoscopic approach was used in 48% of the cases in group A and 58% in group B (p = 0.006).
Discussion
The health emergency caused by the SARS-CoV-2 pandemic resulted in the implementation of regulations issued by the Presidency of the Republic and carried out through the Ministry of Public Health.
Institutional healthcare standards for the care of patients and healthcare workers were established, as well as specific protocols for triage and care of SARS-CoV-2 positive patients1,2.
Undoubtedly, all these measures had an impact at the hospital level. A general perception of the surgical teams was the difficulty in resolving common surgical emergency diseases in patients who, in the context of the pandemic, sought medical care with a more advanced or complicated stage of disease, a fact that could be reflected in higher postoperative morbidity and mortality rates.
In a report carried out in this healthcare setting at Hospital Maciel, Ruso et al. reported that -as a consequence of the healthcare emergency and the recommendations for rescheduling surgeries- there was a steep decline in the number of surgical procedures in the public system throughout the country. Thus, the total volume of surgeries decreased by 48% and elective procedures declined by 83%, while the number of emergency surgeries remained stable, as was also observed in that hospital3.
In general terms, the percentage of emergency surgical conditions in our hospital was similar in both periods, i.e., before and during the health emergency (p = 0.24).
However, the diagnosis associated with complications or advanced stages of the disease was twice as high, as there was a statistically significant difference compared with the same period in 2019 (p = 0.0001).
Postoperative morbidity and mortality were greater in the population analyzed during the COVID-19 pandemic (p = 0.01), which could be due to delayed consultation with complicated conditions, associated systemic involvement and the possible need for greater requirements in the postoperative period.
Like other international publications have mentioned, the attempt to limit the entrance of patients resulted in consultation delays, which is clearly reflected at the time of admission and during the surgical procedure. Zhang4 reported that 50% of elective surgeries that were postponed or canceled resulted in more emergency surgeries for complicated conditions with more advanced disease stages, requirement of intensive care unit, and higher morbidity. That is why he suggested revising the term “elective” as a surgery that can be scheduled but not postponed.
Initially, some studies suggested that the open approach was safer than the laparoscopic one. The rationale for this statement is that video-assisted surgeries are aerosol generating procedures with prolonged operative time thus increasing the risk of transmission5-7.
Thereafter, some studies suggested that the risk of transmission is lower when the laparoscopic approach is performed with the appropriate equipment and by experienced surgeons8. Other authors describe that the laparoscopic approach requires extreme measures to protect the airway and mucous membranes and avoid direct exposures during outflow of gas, occasional evacuations or final evacuation9.
The most recent guidelines of the SAGES and EAES10 suggest that while laparoscopy can theoretically lead to aerosolization of blood borne viruses, there is no evidence available to confirm this is the case with COVID-19. In fact, several studies failed to isolate the virus in samples of peritoneal fluid in these patients11.
Therefore, the decision of the approach should be made considering its benefits.
Bearing this in mind, it was reasonable to expect a slight increase in the open approach compared with the previous period (pre-COVID-19), a fact that we believe may be influenced by international protocols or guidelines on the approach in COVID-19 patients.
However, this perception proved to be wrong, as there was a statistically significant difference (p = 0.006) in favor of the laparoscopic approach in the group influenced by the presence of the pandemic. Our center is a university hospital in which the surgical team on duty is made up of residents in surgery and trained surgeons who might have chosen this approach based on the experience of the attending clinician, the patients’ needs, and on many studies which have demonstrated that the approach does not represent a major biohazard.
It should be noted that in our hospital all patients requiring emergency surgery underwent clinical triage, and no patients with suspected COVID-19 or confirmed cases were operated on.
Study limitations and strengths
This is a retrospective study with a sample size that has not been calculated, since the information about the surgical implications of the pandemic is scarce.
On the other hand, the strength of the present work is that it was conducted in a university reference center in Uruguay, where the most complex cases are treated. The period selected for the study does not include mandatory preoperative nasopharyngeal swab testing as nowadays, independently of the presence of respiratory symptoms. Considering that at present many patients become infected during hospitalization, it would be extremely valuable to analyze the preoperative, intraoperative and postoperative complications and how SARS-CoV-2 affects them; this study would then be the trigger for future research.
Referencias bibliográficas /References
1. Plan Nacional de Contingencia para la Infección (COVID-19) por el nuevo Coronavirus (SARS CoV-2). Ministerio Salud Pública. Versión 9.3.2020. [Consulta 3 de mayo de 2020]. Disponible en. Disponible en. https://www.gub.uy/ministerio-salud-publica/comunicacion/publicaciones/plan-nacional-contingencia-para-infeccion-covid-19-nuevo-coronavirus [ Links ]
2. Comunicado Nº 12. Definiciones de caso confirmado y sospechoso y realización de hisopados. Comité de Contingencia Coronavirus. ASSE. 27.3.2020 [ Links ]
3. Ruso L, Rodríguez G, Perdomo M, Olivera E, Bruno G, González D y cols. COVID-19 en fase 2 sostenida. Experiencia quirúrgica inicial en el Hospital Maciel. Cir Urug 2020;4(2):1-3. [ Links ]
4. Zhang S. What it really means to cancel elective surgeries: to make room for coronavirus patients, hospitals are delaying procedures that would make major differences in people’s li ves. The Atlantic. March 17, 2020.12.[Consulta 16 de abril de 2020]. Disponible en: Disponible en: https://www.theatlantic.com/science/ar chive/2020/03/patients-whose-surgeries-are-canceled-because-coronavirus/608176 [ Links ]
5. De Simone B, et al. Emergency surgery during COVID-19 pande mic: what you need to know for practice. Ann R Coll Surg Engl. 2020;00:1-10. [ Links ]
6. Kwak HD, Kim SH, Seo YS, Song KJ. Detecting hepatitis B virus in sur gical smoke emitted during laparoscopic surgery. Occup Environ Med. 2016;73:857-63. [ Links ]
7. Choi SH, Kwon TG, Chung SK, Kim TH. Surgical smoke may be a biohazard to surgeons performing laparoscopic surgery. Surg En dosc. 2014; 28:2374-80. [ Links ]
8. Zheng MH, Boni L, Fingerhut A. Minimally Invasive Surgery and the Novel Coronavirus Outbreak: Lessons Learned in China and Italy. Ann Surg. 2020;272(1):e5-e6. [ Links ]
9. Balibrea JM, Badia JM, Rubio Pérez I , Martín Antona E, Álvarez Pena E y cols.. Manejo quirúrgico de pacientes con infección por COVID-19. Recomendaciones de la Asociación Española de Cirujanos. Rev Esp Cir. 2020: 98:251-59. [ Links ]
10. Francis N, Dort J, Cho E, Feldman L, Keller D, Lim R. SAGES and EAES recommendations for minimally invasive surgery during COVID-19 pandemic. Surg Endosc. 2020;34(6):2327-31. [ Links ]
11. Ngaserin SH, Koh FH, Ong B, Chew MH. COVID-19 not detected in peritoneal fluid: a case of laparoscopic appendicectomy for acu te appendicitis in a COVID-19-infected patient. Langenbecks Arch Surg. 2020 9:1-3. [ Links ]
Received: January 21, 2021; Accepted: April 19, 2021











 texto en
texto en