Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista argentina de cirugía
versión impresa ISSN 2250-639Xversión On-line ISSN 2250-639X
Rev. argent. cir. vol.114 no.2 Cap. Fed. jun. 2022
http://dx.doi.org/10.25132/raac.v114.n2.1633
Articles
Experience in laparoscopic distal pancreatosplenectomies
Introduction
Distal pancreatectomy with or without splenectomy is a surgical technique used to approach traumatic, benign or malignant lesions of the left pancreas. The right portion (head) and the left potion (body and tail) are divided by the mesentericoportal axis at the level of the neck and behind it1. This division allows different types of surgical techniques depending on the location of the lesion and whether the lesion is suspected to be benign or malignant.
In recent years, the indication for laparoscopic surgery of the pancreas has increased as an increasing number of pancreatic lesions are incidentally detected with the expansion of utilization of imaging tests currently being performed2.
The aim of this study is to analyze the documented results of the experience in laparoscopic distal pancreatectomies and splenectomies in the section of hepatobiliary and pancreatic surgery in our hospital to evaluate the results and benefits obtained.
Material and methods
We conducted a retrospective and observational study. Data from 17 patients operated on in the section of hepatobiliary and pancreatic surgery of Hospital Militar Central de Buenos Aires between 2015 and 2020 were retrieved from the electronic clinical records. The following variables were analyzed: demographics, personal history, reasons for consultation, American Society of Anesthesiologists (ASA) physical status classification3, preoperative and pathological diagnoses, tumor size, type of procedure and level of pancreatic section, operative time, conversion rate, length of stay in the intensive care unit (ICU) and length of hospital stay (from admission to hospital discharge). Readmissions were defined as a new hospitalization within 30 days after hospital discharge. The type of nutrition and postoperative complications according to the modified Clavien- Dindo classification4 were recorded. Postoperative pancreatic fistulas were classified according to the 2016 International Study Group on Pancreatic Fistula (ISGPF) criteria5. Data were analyzed using a Microsoft Office Excel spreadsheet.
Surgical technique: the patient was positioned in the supine position with his/her legs apart and rotated to the right. Pneumoperitoneum was performed with Veress needle inserted above the umbilicus. A 12-mm supraumbilical trocar was inserted in the midline. Under direct laparoscopic vision, three trocars were inserted: a 12-mm trocar in the midclavicular line below the left costal margin, a 5-mm trocar in the mid-clavicular line below the right costal margin, and a 5-mm trocar in the left flank and anterior axillary line. Exploratory laparoscopy: The greater omentum was opened using a vessel sealing device to access the lesser sac until reaching the short vessels. A 2.0 Nylon® suture was used for gastropexy. The splenic flexure of the colon was lowered. The inferior border of the pancreas was dissected from the neck (superior mesenteric vein) to the tail allowing mobilization of the gland. Intraoperative ultrasound was performed with a high frequency laparosocopic probe to detect the lesion and the macroscopic resection limits. The splenic artery and the splenic vein were dissected and identified at the level of the neck of the pancreas and were sectioned with 45-mm vascular mechanical stapler (roticulator stapler with 3 rows of staples). A tunnel below the neck of the pancreas was created using a tape. The pancreas was transected using a 60-mm mechanical stapler (roticulator stapler with 3 rows of staples) and intraoperative ultrasound was performed thereafter. The dissection continued in a medial to lateral direction. The splenic ligaments were released. The surgical specimen was removed in a laparoscopic retrieval bag through a Pfannestiel suprapubic incision using a wound retractor. Two drains were left in all the patients for the pancreatic bed and splenic bed.
Results
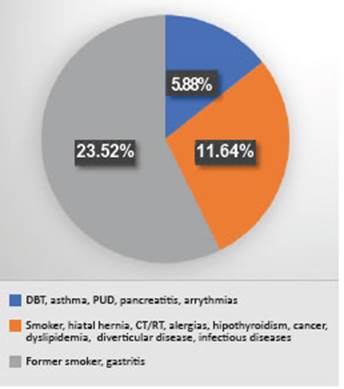
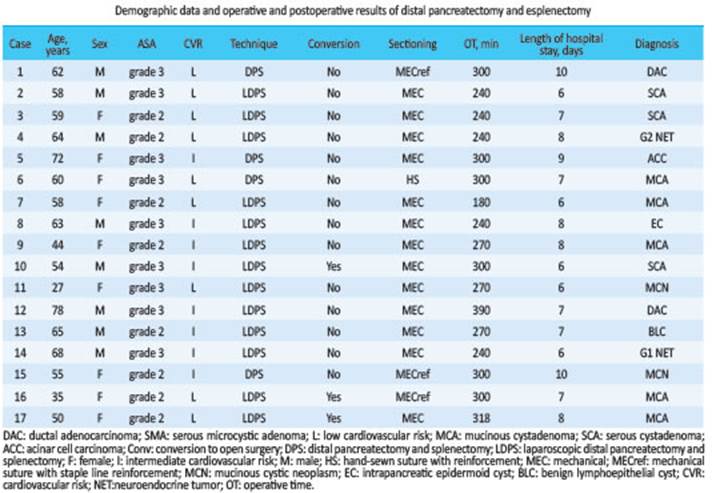
During the study period, 17 patients underwent distal pancreatectomy; 47.10% were men (n = 8) and 52.90% were women (n = 9). Mean age was 57 years (range 27-78). The ASA physical status classification system was grade 3 in 52.94% of the patients and grade 2 in 47.05% (Table 1). Most patients reported history of surgery (88.23%), hypertension and gastroesophageal reflux (GERD) (29.41%). The data are summarized in Figure 1.
The reasons for consultation included incidental tumors in 52.94% (n = 9), abdominal pain in 48.06% (n = 8), loss of weight in 11.76%, abdominal bloating in 5.88% and constipation in 5.88%. The diagnostic tests most commonly performed were abdominal ultrasound and contrast-enhanced multidetector-row computed tomography scan and were complemented with magnetic resonance imaging with gadolinium-based contrast agent, dynamic scan of the pancreas, magnetic resonance cholangiopancreatography, laboratory tests with tumor markers and positron emission tomography (PET-CT) in case malignancy was suspected.
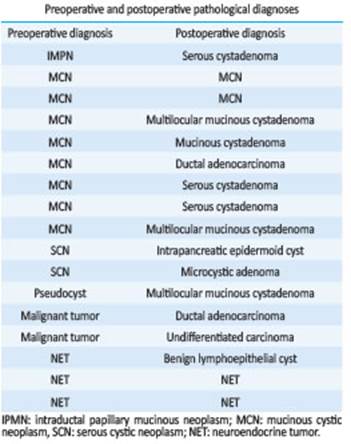
The preoperative diagnoses were mucinous cystic neoplasm (MCN) in 47.06% (n = 8), neuroendocrine tumor (NET) in 17.66% (n = 3), serous cystic neoplasm (SCN) in 11.76% (n = 2) operated on due to tumor size and symptoms, malignant tumor in 11.76% (n = 2), intraductal papillary mucinous neoplasm (IPMN) in 5.88% (n = 1) and pancreatic pseudocyst (PPC) in 5.88% (n = 1). The comparative data with the postoperative pathological diagnoses are shown in Table 2. The mean size of the tumors was 4.26 cm (range 2-10 cm). Involvement of other organs: 1 patient presented splenic vein thrombosis in the imaging tests made for preoperative staging.
Of the 17 patients with indication for surgery, 13 underwent laparoscopic distal pancreatectomy and splenectomy while the conventional approach was performed in 4 patients. The criteria for laparoscopic surgery were based on the absence of proximity of the tumor to the mesentericoportal axis and of extrapancreatic extension in case of malignancy. Other criteria included tumor size, distal lesions, and surgeon’s experience. The 4 patients undergoing conventional surgery were excluded from laparoscopy due to tumor thrombosis of the mesentericoportal axis, tumor size and history of abdominal surgeries. Among the patients who underwent surgery, laparoscopy was indicated in 76.47%.
The conversion rate of the 13 distal laparoscopic pancreatectomies and splenectomies was 23.08% (n = 3) (Table 1). The reasons for conversion were intraoperative bleeding (n = 2) and difficult pancreatic dissection (n = 1). One patient underwent an associated left partial adrenalectomy due to tumor infiltration and 5 patients required video-assisted laparoscopic cholecystectomy due to cholelithiasis.
Median operative time was 270 minutes (Table 1). The pancreas was sectioned at the level of the neck in 14 patients and at the level of the body in 3. Mean length of hospital stay was 7.41 days (Table 1). In our department, the protocol establishes that patients undergoing this type of procedures should be transferred to the intensive care unit (ICU) for strict postoperative monitoring. Mean stay in the ICU was 2.52 days (range 1-8). Oral feeding was started early in all the patients (48 hours).
The complications observed in our series were sub-divided in minor (grade I and II) and major (grade IIIa and b, IVa and b, and V)4 (Table 3). Two patients presented grade I complications which were biochemical leaks that did not prolong hospital stay and had no clinical impact. Grade II complications included 2 bleeding events requiring transfusion, 4 episodes of hyperglycemia that were treated with insulin, 3 hospital-acquired pneumonias treated with broad-spectrum antibiotics, 1 postoperative ileus that required insertion of a nasogastric tube for gastric decompression, 2 type B fistulas treated with octreotide, parenteral nutrition and drainage, and 1 surgical site infection that required rotation of the initial antibiotic regimen. Finally, grade IIIa complications included 1 type B fistula requiring computed tomography-guided percutaneous drainage and 1 abdominal collection treated with ultrasound-guided percutaneous drainage (Table 4). In cases of pancreatic leaks and fistulas, the analysis of drainage fluid showed amylase levels > 3 times the upper limit of normal serum amylase activity5. Two patients were readmitted due to the grade IIIa complications previously mentioned. None of the patients died or required reoperations in our series.
Discussion
In this analysis of the surgical experience of our department, we conclude that the laparoscopic technique is a safe and effective approach for benign and malignant conditions in properly selected cases, based on an exhaustive staging and preoperative planning. In agreement with other published studies, the surgeon’s experience in pancreatic surgery and advanced laparoscopy should also be considered6-10. Recent studies have confirmed that the laparoscopic approach tends to reduce intraoperative bleeding and to shorten time to feeding and length of hospital stay11-13.
Although there are techniques with and without splenic preservation, in all our cases we performed splenectomy due to tumor size, preoperative diagnosis and confidence in the surgical skills of the treating team considering our learning curve, since the number of patients in our series is lower than that of other centers with high volume of patients undergoing pancreatic surgery. Taking this into consideration, the mean operative time in our study (270 minutes) was not very different from the one reported in another centers7-9,12.
Several publications have reported that certain tumors, such as mucinous cystadenoma, intraductal mucinous neoplasia and NETs have a higher risk of malignant transformation and thus should be resected once the diagnosis is made or in case of suspicion14.
In the pathological examination, most tumors were benign, in agreement with the incidence reported in other series7,6,12, and all the malignant tumors underwent adequate oncologic resection.
As for the surgical complications, biochemical leakage (type A) and pancreatic fistula (type B) occurred in 11.76% and 17.64% of the cases, respectively, and there were no type C fistulas. In other published series of laparoscopic pancreatectomies, Marcos García Ejarque et al. reported an incidence of type B and C fistulas of 18% while Oscar M. Mazza et al. reported 23% (n = 6) of grade A fistulas, 7.69% (n = 2) of grade B and 7.69% (n = 2) of grade C fistulas. Finally, Brian K. P. Goh reported 41 grade A fistulas (18%), 13 (16%) grade B fistulas and 18 (8%) grade C fistulas.
Some publications reported that the use of mechanical stapler to close the pancreatic stump in laparoscopic surgery could increase the incidence of pancreatic fistula; however, it has been demonstrated that the incidence of fistula in conventional surgery is high (30%), so this should not be a limitation15,16. Moreover, there are no significant differences in the risk of fistula between closure of the pancreatic stump with mechanical stapler or hand-sewn suture17-19,1,20. In our series we did not obtain discordant results when comparing pancreatic transection performed with mechanical stapler or reinforced stapler. Morbidity rate was similar to other publications.
Referencias bibliográficas /References
1. Galindo F. Resecciones pancreáticas. En: Galindo F y cols. Enciclopedia Cirugía Digestiva. Buenos Aires: s.n., 2014. Cap 486, pp.1. [ Links ]
2. Jusoh AC, Ammori Basil J. Laparoscopic versus open distal pancreatectomy: a systematic review of comparative studies. [En línea] Surg Endosc. 2012. 10.1001/s00464-011-2016-3. [ Links ]
3. Owens WD, Felts JA, Spitznagel EL Jr. ASA Physical status classifications: a study of consistency of ratings. [En línea] october de 1978. 10.1097/00000542-197810000-00003. [ Links ]
4. Clavien P, et al. The Clavien-Dindo classification of Surgical Complications: Five-Year experience. [En línea] August de 2009. 10.1097/SLA.0b013e318b13ca2. [ Links ]
5. Bassi C, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. [En línea] 2016. 10.1016/j.surg.2016.11.014. [ Links ]
6. Melotti G, Butturini G, Piccoli M, et al. Laparoscopic distal pancreatectomy: results on a consecutive series of 58 patients. 1 Ann Surg, 2007; 246: 77-82. [ Links ]
7. Fernández-Cruz L, Herrera M, Sáenz A, et al. Laparoscopic pancreatic surgery in patients with neuroendocrine tumours: indications and limits. 2. Best Pract Res Clin Endocrinol Metab. 2001; 15: 161-75. [ Links ]
8. García Ejarque M, Durán M, Bregante M, Bogetti D, Maurette R, Pirchi D. Pancreatectomía distal laparoscópica: nuestra experiencia. 2. 2016, Fronteras en Medicina. 2016; 11:39- 42. [ Links ]
9. Mazza OM y cols. Pancreatectomías distales laparoscópicas: nuestra experiencia. RevArgent Cirug. 2015;107 (2): 51-6. [ Links ]
10. Korrel M, Vissers FL, Van Hilst J, de Rooij T, Dijkgraaf MG, Festen S, Groot Koerkamp B, et al. Minimally invasive versus open distal pancreatectomy: an individual patient data meta-analysis of two randomized controlled trials. 3. International minimally invasive pancreatic resection trialists group. 2020; 23: 323-30. [ Links ]
11. Nigri GR, Rosman AS, Petrucciani N, et al. Metaanalysis of trials comparing minimally invasive and open distal pancreatectomies. 5. Surg Endosc. 2011; 25:1642-51. [ Links ]
12. Melotti G, Butturini G, Piccoli M, Casetti L, Bassi C, Mullineris B, et al. Laparoscopic distal pancreatectomy results on a consecutive series of 58 patients. 2007, Ann Surg. 2007; 246:77-82. [ Links ]
13. Poves I, Burdio F, Dorcaratto D, Grande L. Resultado del abordaje laparoscópico en la pancreatectomía izquierda. 1. Cir Espan. 2013; 91: 25-30. 0009-739X. [ Links ]
14. Jean Michel Butte JM y col. Pancreatectomía distal: Indicaciones y resultados quirúrgicos inmediatos. [ed.] Revista Chilena de Cirugía. Revista Chilena de Cirugía. 2007; 59:360-5. [ Links ]
15. Hashimoto Y, Traverso LW. After distal pancreatectomy pancreatic leakage from the stump of the pancreas may be due to drain failure or pancreatic ductal back pressure. 2012, J Gastrointest Surg. 2012; 16;993-1003. [ Links ]
16. Goh BK, Tan YM, Chung YF, et al. Critical appraisal of 232 consecutive distal pancreatectomies with emphasis on risk factors, ourcome, and management of the postoperative pancreatic fistula: a 21 year experiencie at a single institution. Arch Surg. 2008; 143: 956-65. [ Links ]
17. Nathan H, et al. Risk factors for pancreatic leak after distal pancreatectomy. Ann Surg. [En línea] August 2009. 10.1097/SLA.0b013e3181ac34be. [ Links ]
18. Ramia JM y col. Pancreatectomía corporocaudal: una misma técnica con variadas indicaciones. 1. Doyma;. Cir Espan. 2005; 77:22-6. [ Links ]
19. Zhou W, Lv T, Wang X, et al. Stapler vs suture closure of pancreatic remnant after distal pancreatectomy: a meta-analysis. Ann J Surg. 2010; 200: 529-36. [ Links ]
20. Diener MK, Seiler CM, Rossion I, et al. Efficacy of stapler versus hand-sewn closure after distal pancreatectomy (DISPACT): a randomised, controlled multicentre trial. 2011, Lancet. 2011; 377: 1512-22. [ Links ]
Received: July 14, 2021; Accepted: December 15, 2021











 texto en
texto en