Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista argentina de cirugía
versión impresa ISSN 2250-639Xversión On-line ISSN 2250-639X
Rev. argent. cir. vol.114 no.3 Cap. Fed. set. 2022
http://dx.doi.org/10.25132/raac.v114.n3.1594
Articles
Hepatocellular carcinoma in intrathoracic ectopic liver tissue
1 Departamento Cirugía General Hospital Interzonal General de Agudos Dr. José Penna, Bahía Blanca. Buenos Aires. Argentina
Ectopic liver is defined as liver tissue with no connection to orthotopic liver due to aberrant migration of hepatic cells during embryonic development1,2. It is a rare finding that is mostly found incidentally in surgical procedures or autopsies and has been described in many sites, but is most common in the gallbladder wall, and, to a lesser extent, in the spleen, pancreas, mesentery, adrenal glands and in supradiaphragmatic sites as the thorax and heart1. Collan et al. described 4 main types: a) an accessory lobe of the liver of considerable size and with a connecting stalk to the liver, b) a small accessory lobe attached to the liver, c) ectopic liver without connection to the liver, and d) microscopic ectopic liver tissue3.
The first case of intrathoracic ectopic liver was reported by Hansbrough and Lipin in 1957. The reason to present this case report is the low number of cases reported in the world literature. We report the case of a 27-year-old otherwise healthy female, former smoker of 10 pack-years, who started with stubbing pain between the shoulder blades 2 months before and progressed to continuous pain. Pain intensity was 6/10, was not relieved by common analgesics, and was associated with a palpable mass at the level of the 5th posterior intercostal space.
Complete blood count, liver panel, liver serology and tumor markers (CA 19-9, CEA and alphafetoprotein) were normal. A contrast-enhanced computed tomography (CT) scan of the thorax, abdomen and pelvis was also ordered. A heterogeneous soft tissue density mass, measuring 50 × 29 × 22 mm, was identified at the right posterior subpleural level, with heterogeneous enhancement after the administration of contrast material. The mass was associated with distortion of the architecture of the body and transverse process of the fifth thoracic vertebra, with extension to the spine cord and paravertebral and intercostal soft tissues. The azygous vein was thickened and occupied, suggestive of thrombosis. The lungs and other structures were within normal limits (Figs. 1a and 1b).

Figure 1 A: Soft tissue density mass involving the posterior and medial wall of the rib cage in contact with the pleural space, and extending to the posterior mediastinum, the spine and body of the 5th thoracic vertebra. B: Contrast-enhanced computed tomography scan of the chest. Sagittal section. Maximum intensity projection reconstruction showing extension of azygous vein thrombosis. C: Contrast-enhanced magnetic resonance imaging of the chest. T1-weighted fat-saturated gadolinium-enhanced image showing an infiltrative, heterogeneous and solid mass invading the adjacent paraspinal muscles and extending into the spinal canal displacing and narrowing the spinal cord.
The preoperative assessment was completed with contrast-enhanced magnetic resonance imaging (MRI) of the thoracic spine, which showed the mass extending from the thoracic spine to the spinal canal and spinal foramen, narrowing the spinal canal and generating spinal edema. The 5th vertebral body and adjacent posterior ribs were involved (Fig. 1c). For these reasons, a CT-guided biopsy was performed and the pathological examination showed the presence of ectopic liver tissue. Surgery was then decided. The patient was positioned in the left lateral decubitus position, anteriorly tilted for better exposure of the spine. The thoracic cavity was approached via a right posterolateral incision through the fifth intercostal space. Pneumonolysis was performed due to lax adhesions between the upper lobe and the tumor, followed by resection of the posterior segment of the 4th and 5th ribs and intercostal muscles. Then, the azygous vein was ligated and partially resected due to tumor invasion and, together with the department of neurosurgery, a partial vertebrectomy was performed at the level of the 5th thoracic vertebra. Subsequently, a polypropylene mesh was fixed using transparietal sutures to replace the thoracic wall and two chest tubes were placed in the base and apex (Figs. 2a, 2b and 2c).
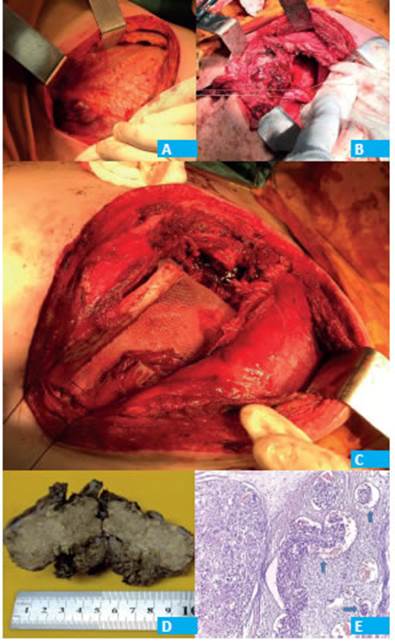
Figure 2 A: Tumor invading the 5th rib. B: Ligation of the azygous vein before its section. C: Wall replacement with polypropylene mesh. D: Gross examination: half section of the mass. The cut surface presents multiple yellowish nodules. D: Hematoxylin and eosin stain (10×). Left: solid pattern of infiltrative hepatocellular carcinoma. Right: vascular tumor invasion (arrows).
The patient evolved with favorable outcome and acceptable pain tolerance. The pleural drainages were removed and the patient was discharged on postoperative day 7. The pathological examination of the surgical specimen reported the presence of hepatocellular carcinoma with micronodular cirrhosis in ectopic liver tissue (Figs. 2d and 2e). The patient underwent regular postoperative follow-up with favorable outcome of the surgical site and did not present associated symptoms. One month after surgery, she presented with a mass of approximately 2 cm in diameter in the right mandible, hard elastic in consistency and fixed to deep planes, which was not associated with symptoms. As the mass had not been described in the previous staging CT scan, a core-needle biopsy was performed. The pathological examination of the mass revealed metastasis of hepatocellular carcinoma. The case was discussed in a multidisciplinary oncology committee and adjuvant treatment with oral sorafenib was decided.
After three months of treatment with sorafenib, the mandibular mass increased in size; sorafenib was switched to intravenous nivolumab, with no response. Third-line treatment with intravenous gemcitabine + oxaliplatin was then initiated with a partial response > 75% in the target lesion of the right mandible. After 19 months of postoperative treatment, when this case report was submitted, the patient presented complete regression of the mandibular lesion.
Ectopic liver tissue is a rare entity with a higher rate of neoplastic transformation than that of normal liver. According to Yamashita et al., there were 70 cases of ectopic liver reported in the literature up to 1985; they included 9 cases with transformation to hepatocellular carcinoma4. The presence of ectopic liver is more common in the Asian population, but a few cases have also been reported in Western populations5. In Japan, the estimated incidence is 0.47%4. It is usually asymptomatic; however, it can occasionally cause compression of adjacent structures, intra-abdominal bleeding and hepatocarcinogenesis5.
Ectopic liver tissue, as normal liver tissue, is affected by the same risk factors for the development of hepatocellular carcinoma, such as infection with hepatitis B and hepatitis C viruses. However, these factors seem to be less involved in the development of hepatocellular carcinoma compared with orthotopic liver. Arakama et al. reported 22 cases of ectopic liver affected by hepatocellular in which the mother liver was free of disease. Viral serology was positive in only 2 cases4. Thus, our case meets all the characteristics previously mentioned, since the patient did not present risk factors for hepatocellular carcinoma. The increased incidence of hepatocellular carcinoma in ectopic liver has not been defined yet. Independently of their location, because ectopic liver does not have a complete vascular and ductal system as a normal liver, it may be more exposed to hepatocarcinogenesis agents affecting the mechanisms of nuclear repair4,6.
The treatment of choice for patients presenting with ectopic liver tissue with or without hepatocellular carcinoma is surgical resection, with favorable longterm outcomes especially if complete tumor resection is achieved,4 as in our case. Few long-term follow-up data of these patients are found in the literature. In their publication, Leone et al. reported that one of the three cases reported presented multiple abdominal recurrences with progression to multifocal hepatocellular carcinoma in the mother liver, while the other two cases were free of disease at 4 years of follow-up5.
Referencias bibliográficas /References
1. Braun M, Kuncman W, Teresiński L, et al. Pure hepatocellular carcinoma originates from an ectopic liver nodule located in the pancreas. Contemp Oncol. 2017;21(4):311-31. [ Links ]
2. Seo UH, Lee HJ, Ryu WS, et al. Laparoscopic resection of a hepatocellular carcinoma arising from an ectopic liver. Surg Laparo Endo Per. 2008;18(5):508-10. [ Links ]
3. Collan Y, Hakkiluoto A, Hästbacka J. Ectopic liver. Ann Chir Gynaecol. 1978;67(1):27-9. PMID: 637502. [ Links ]
4. Arakawa M, Kimura Y, Sakata K, Kubo Y, Fukushima T, Okuda K. Propensity of ectopic liver to hepatocarcinogenesis: case reports and a review of the literature. Hepatology. 1999; 29:57-61. [ Links ]
5. Leone N, De Paolis P, Carrera M, Carucci P, Musso A, David E, et al. Ectopic liver and hepatocarcinogenesis: report of three cases with four years’ follow-up. Eur J Gastroenterol Hepatol. 2004; 16:731-5. [ Links ]
6. Caygill CP, Gatenby PA. Hígado ectópico y hepatocarcinogénesis. Revista Europea de Gastroenterología y Hepatología. 2004;16 (8):727-9. [ Links ]
Received: March 29, 2021; Accepted: May 07, 2021











 texto en
texto en 


