Primary hyperparathyroidism (PHPT) is characterized by elevated levels of calcium and parathyroid hormone (PTH)1. It affects approximately 0.3% of the general popu lation, with women experiencing twice the incidence, and both pregnant and nonpregnant women having a similar frequency2. Nonspecific clinical manifestations and changes in calcium metabolism that occur during pregnancy can complicate the diagnosis of PHPT3.
Studies suggest a correlation between higher calcium levels and increased risks of maternal, fetal, and neonatal complications4,5. Mild cases of PHPT can be managed conservatively, but in cases of severe or symptomatic hyper calcemia, parathyroidectomy is the treatment of choice3.
The aim of this presentation is to highlight an unusu al case of PHPT in a pregnant woman, with a particular emphasis on the complications, diagnostic methodolo gies, and therapeutic interventions implemented.
Clinical case
Patient, a 17-year-old female was admitted to the hos pital with a history of 9-week amenorrhea and intoler ance to fluids and solids lasting over a week. Pregnancy at 9.1 weeks was confirmed by obstetric ultrasound (US), and the condition was interpreted as gravidarum hyper emesis. Treatment was initiated with fluid replacement, vitamin B supplementation, and antiemetics.
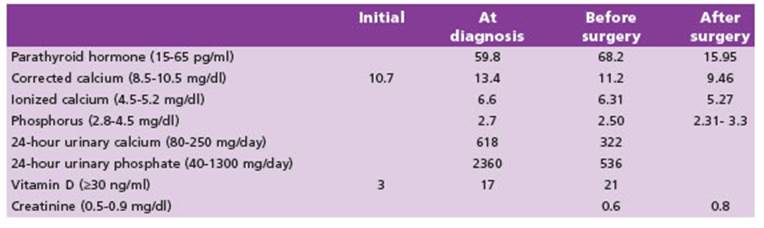
After 24 hours, the patient developed severe head ache, photophobia, muscular weakness, difficulty walk ing, and right sided faciobrachiocrural hemiparesis ac companied by ipsilateral hemihypoesthesia. An urgent computed tomography of the brain revealed acute ce rebral venous thrombosis in the superior sagittal si nus and left transverse sinus. A cerebral angiography was performed, confirming the diagnosis of dural sinus thrombosis (longitudinal, transverse, and left sigmoid). Thrombophilia studies yielded normal results. Concur rently, serum calcium level was found to be 10.7 mg/dl and 25(OH)D was 3 ng/ml (Table 1). Biochemical param eters of renal function were within normal range. The patient was discharged with a prescription of enoxapa rin and vitamin D3.
During follow-up, total serum calcium level was found to be 13.4 mg/dl, ionized calcium 6.6 mg/dl, PTH 59.8 pg/ ml, and urinary calcium excretion 618 mg/day (Table 1). These results confirmed the diagnosis of PHPT in the woman at 19.1 weeks of gestation. The patient was read mitted for the establishment to treat hypercalcemia (Ta ble 1). Upon discharge, a parathyroid US was performed, revealing a 6.6 mm hypoechoic solid nodule located be hind the lower pole of the right thyroid lobe, suggestive of a parathyroid adenoma (Fig. 1).
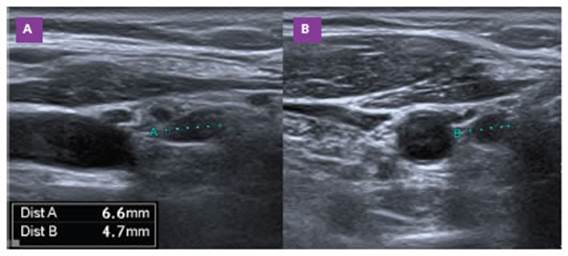
Figure 1 Ultrasonographic findings of parathyroid adenoma. The patient’s ultrasound scan revealed a 6.6-mm adenoma of the lower portion of the right parathyroid gland. A: Sagittal orientation. B: Transverse orientation
At 24 weeks of pregnancy, an obstetric US revealed a fetal weight of 511 grams, estimated gestational age of 21.5 weeks, and increased resistance in the uterine arter ies. These findings indicated intrauterine growth restric tion (IUGR). Furthermore, ventricular extrasystoles were observed in the maternal electrocardiogram.
A multidisciplinary decision was made to perform surgical intervention for PHPT, considering the persistent hypercalcemia and hypercalciuria alongside the pres ence of IUGR. A parathyroidectomy was performed on the lower right parathyroid gland. Corrected calcium levels, accounting for albumin, were recorded at 9.3 mg/dl (Ta ble 1). Obstetric evaluation demonstrated preserved fetal well-being, and the patient was discharged on the sev enth day. The histopathological analysis revealed a para thyroid adenoma with a maximum diameter of 9 mm and no signs of malignancy.
During the follow-up period, the patient developed severe hypertension, proteinuria of 7 grams in a 24-hour period, and IUGR, suggestive of severe preeclampsia. At 33.1 weeks of gestation, the decision was made to admit the patient for antihypertensive treatment and expedite delivery. An emergency cesarean section was performed after discontinuing enoxaparin, resulting in the birth of a female neonate. The neonate had a gestational age of 33 weeks, and birth weight of 1320 grams. Apgar scores of 8 at one minute and 9 at five minutes were obtained to as sess the neonate’s condition.
This publication was approved by the Ethics Commit tee, and written informed consent was obtained from the patient.
Discussion
PHPT is a common cause of hypercalcemia and is characterized by elevated levels of calcium and PTH1. In this case, we present an occurrence of PHPT in a pregnant adolescent, elucidating the related complica tions, the employed diagnostic methodology, and the established treatment.
It is well-established that women, both pregnant and nonpregnant, have a higher incidence of PHPT compared to men2. The hormonal and metabolic changes during pregnancy can complicate the diagnosis, as the symp toms of PHPT may overlap with those commonly seen in pregnancy3. During pregnancy, total calcium concentra tions may appear falsely lower and PTH may be physi ologically suppressed. PTH levels can decrease because of the physiological rise in parathyroid hormone-related protein. Its levels begin to increase as early as 3-13 weeks into gestation and continue to peak in the third trimester, which can lead to the suppression of PTH levels3. The combination of elevated ionized or albumin-corrected calcium associated with detectable PTH is indicative of PHPT in most cases6. The diagnosis of PHPT in our patient was confirmed by elevated calcium levels and normal/high PTH levels.
Approximately 10% of cases of PHPT are attributed to hereditary syndromes such as multiple endocrine neoplasia, familial hypocalciuric hypercalcemia, hyper parathyroidism jaw tumor, and familial isolated PHTP7. The remaining 90% of cases are sporadic, commonly caused by parathyroid adenomas. Due to the earlier age of onset of familial parathyroid disorders compared to sporadic disease, genetic testing should be considered in pregnant women with PHPT7. In our case, we did not have the availability to carry out genetic testing, but it will be a matter to be considered in the future. This approach will allow us to assess the necessity of organ-specific examinations, including those involving the pituitary gland, thyroid, adrenal glands, pancreas, and other relevant structures.
The optimal method for localizing parathyroid ad enomas in PHPT during pregnancy remains a topic of debate. US has a sensitivity of 69% and specificity of 94% for diagnosing and localizing parathyroid adenomas8. Sestamibi scanning, which has a sensitivity of 80% to 99% for single adenoma identification, is not recom mended during pregnancy due to the potential placental transfer of 99-Tm-sestamibi9. Given the limitations of imaging modalities during pregnancy, a bilateral surgical approach may be required to locate all four parathyroid glands6,10. Intraoperative PTH monitoring, validated in non-pregnant individuals, can be employed to confirm successful excision of the glands3.
The clinical presentation and the occurrence of ma ternal, fetal, and neonatal complications in pregnant women with PHPT are influenced by the level of hyper calcemia. Numerous studies have demonstrated an in creased risk of adverse outcomes, including preeclamp sia, IUGR, maternal hypertension, and other complica tions, in pregnant women with PHPT4,5,11. Nephrolithiasis is commonly observed in symptomatic patients with PHPT during pregnancy. Fetal complications associated include premature birth, IUGR, low birth weight, neo natal hypocalcemia, and tetany due to the suppression of fetal parathyroid tissue3-5. Our patient developed pre eclampsia following the resolution and remission of the disease of PHTP. This finding should not be surprising, as it has been demonstrated that a history of parathyroid adenoma, even up to 5 years before delivery, is associated with an increased risk of preeclampsia11. These complications underscore the importance of multidisci plinary management in pregnant patients with PHPT, as close monitoring and timely intervention are essential for optimizing outcomes.
In our case, the patient presented with venous sinus thrombosis, which added further complexity to the management. Thrombophilia studies yielded normal re sults, indicating that the thrombosis may be associated with hypercalcemia. Several potential mechanisms have been proposed to explain the pathophysiological link between calcium and thrombosis. Calcium can induce vasoconstriction by activating vascular smooth muscle, triggering platelet aggregation, and activating various clotting factors12. Increases in platelet count, elevated factor FVII and FX activities, elevated D-dimer, elevated levels of tissue plasminogen activator inhibitor-1 (PAI-1) and tissue plasminogen activator, and decreased levels of factor pathway inhibitor were observed in PHTP13. Additionally, it has been demonstrated that there is a correlation between elevated PAI-1 and PTH levels in PHPT patients14. However, the possibility that PHPT may synergically promote thrombosis when interacting with other prothrombotic factors such as mutations or autoimmune cannot be excluded.
The management of PHPT during pregnancy should be based on gestational age, severity of hypercalce mia, and risk-benefit balance. In cases of symptomatic hypercalcemia or when complications are present, surgery is the preferred treatment option3,8. Research has shown that parathyroidectomy during pregnancy in women with gestational HPT resulted in a signifi cantly lower neonatal complication rate compared to medical therapy15. The optimal timing for surgery is in the second trimester, especially if albumin-adjusted calcium is above >11.42 mg/dl and/or above >1 mg/dl upper limit of normal, and/or ionized calcium is above >5.81 mg/dl, as in the first trimester fetal organogen esis takes part and in the third trimester the risk for preterm labor increases3. Close monitoring of calcium levels and a conservative treatment approach may be appropriate for mild to moderate hypercalcemia (serum calcium <11 mg/dl), but if maternal-fetal complications occur or conservative medical therapy fails, urgent parathyroidectomy is recommended regardless of fetal gestational age15. However, some studies suggest that mild hypercalcemia may not exclude the possibility of severe complications4,5.
In conclusion, this case underscores the challenges in diagnosing and managing PHPT in pregnancy. Early recognition, appropriate diagnostic evaluation, and tai lored management, including parathyroidectomy when indicated, are crucial to mitigate the risks associated with PHPT in pregnancy and optimize maternal and fetal outcomes.