The apnea test is a widely utilized diagnostic technique for brain death (BD) assessment, aim ing to demonstrate the absence of respiratory drive due to hypercapnia1. The apnea test using the tracheal oxygen insufflation mode (I-AT) in volves disconnecting the patient from invasive mechanical ventilation (iVM) for approximately 8 minutes while maintaining oxygenation by advancing an insufflation catheter into the en dotracheal tube, to the level of the carina. This apnea test mode supports the diagnosis of BD when an increase in PaCO2 exceeding 20 mmHg compared to the baseline or a PaCO2 level ex ceeding 60 mmHg is determined at the end of the test.
Hypoxemia and hemodynamic instability are frequent side effects of the I-AT treatment that may be more severe in patients who already have hypoxemia or obesity2,3. Another complication less reported during the I-AT is the mag nitude of lung collapse induced by the loss of in trathoracic pressure. Additionally, lung collapse can persist after iVM reconnection, leading to reduced end-expiratory lung volume (EELV) and increasing pulmonary strain, even without hy poxemia4. Furthermore, a number of therapies, including recruitment maneuvers, may increase pulmonary strain and stress in an attempt to prevent this EELV loss, which could result in lung injury5.
The CPAP-mode apnea test (CPAP-AT), an al ternate technique, has shown better PaO2/FiO2 values than I-AT6. By maintaining constant pres sure in the airway, CPAP-AT could prevent the occurrence of atelectrauma, thus mitigating the risk of lung injury in lung donors.
On the other hand, nothing is known about how lung volumes and lung strain behave in various apnea test modes.
Electrical impedance tomography (EIT) pro vides a valuable tool for assessing lung aera tion by analyzing impedance (resistance to al ternating current) in the thoracopulmonary system7,8. While this tool measures impedance variation, it maintains a linear relationship with volume changes, allowing these terms to be interchangeable. EIT can estimate the EELV during the apnea test9. Also can be measured the tidal volume and pulmonary strain, revealing poten tial mechanisms of lung injury with different ventilation strategies10-12.
We provide a case series comprising three brain death diagnosis patients to examine differences in lung volumes and global pul monary strain between I-AT and CPAP-AT. Be cause of their persistent oncological illnesses, these patients were not considered for organ donation.
Case series
The first case involved a 43-year-old female patient with a history of medical breast cancer, obesity (body mass index = 40.2), and asthma. She was diagnosed with BD attributed to a left frontotemporal intracerebral he matoma measuring 60 × 43 mm, accompanied by a mid line shift of 13 mmHg. This condition was secondary to anticoagulation therapy for transverse venous sinus thrombosis.
The second case involved a 63-year-old female patient recently diagnosed with acute myeloid leukemia. She ex perienced refractory intracranial hypertension resulting from multiple intraparenchymal cerebral hematomas. These hematomas were a consequence of severe throm bocytopenia, a side effect of her ongoing chemotherapy regimen involving cytarabine and idarubicin.
In the third case, a 62-year-old female patient who had been recently diagnosed with adenocarcinoma affecting the pleura, heart, and bone, and whose primary tumor’s origin remained unidentified, suffered an ischemic stroke in the right occipito-parietal region. This stroke was fur ther complicated by extensive hemorrhagic transforma tion within the affected area.
In all three cases, the diagnosis of BD was confirmed by detecting systolic spikes in the examined arteries using transcranial Doppler ultrasound. The diagnostic process was completed by performing the apnea test.
We used EIT equipment to estimate lung volumes du ring the different apnea tests (Pulmovista V500, Drager, Germany). This equipment consists of a belt equipped with 16 channels and is positioned at the level of the fifth intercostal space. It allows continuous monitoring of glo bal and regional changes in TV and EELV.
Initially, all patients underwent I-AT. Unfortunately, one patient experienced hypoxemia and had to discon tinue the test prematurely. However, the remaining pa tients completed the study without any complications. Throughout the apnea period for all patients, EIT con sistently showed the complete cessation of pulmonary ventilation. During I-AT, there was a notable decrease in EELV for the three patients. Specifically, in patient 1, EELV decreased by 701 ml; in patient 2, 669 ml; and in patient 3, 433 ml. This reduction in EELV indicates lung collap se resulting from the cessation of intrathoracic positive pressure.
During the CPAP-AT, we observed minor reduction in EELV compared to I-AT. Specifically, in patient 1, EELV de creased by 282 ml; in patient 2, by 97 ml; and in patient 3, by 146 ml. This indicates that the applying continuous positive pressure during the apnea test effectively pre vented a substantial decrease in EELV compared to I-AT. It prevented of approximately 59.8%, 85.5%, and 66.3% of the EELV reduction observed during I-AT.
Since the tidal volume was constant, the lower reduc tion in EELV after CPAP-AT implied an improvement in pulmonary strain compared to I-AT. In CPAP-AT, the pul monary strain values were 0.88, 0.76, and 0.80, while in I-AT, they were 0.91, 1.20, and 1.07 for patients 1, 2, and 3, respectively. Table 1 provides comprehensive information about the demographic characteristics, ventilatory para meters, and EIT data for the three patients involved in the study. For a visual representation of these changes, please refer to Figure 1, which illustrates the variations in tidal impedance and end-expiratory lung impedance during I-AT and CPAP-AT.

Figure 1 Monitoring of tidal impedance variation and end-expiratory lung impedance using electrical impedance tomography during the apnea test with tracheal oxygen insufflation and during the application of continuous airway pressure
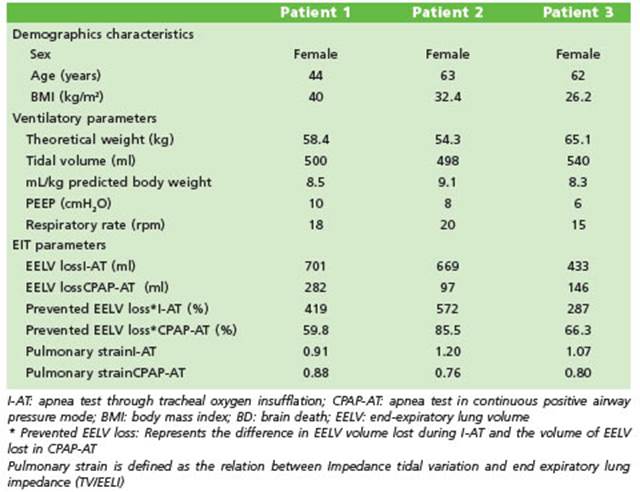
Table 1 Demographic characteristics, ventilatory parameters, and electrical impedance tomography data
Written informed consent was obtained from patient’s relatives.
Discussion
In this case series of three patients assessed using EIT, it was observed that CPAP-AT effec tively mitigated the lung collapse that occurs when disconnecting from iMV during I-AT. This prevention resulted in preserving 70.5% (+/-11) of EELV. Since tidal volume remained constant during both tests, the more significant decrease in EELV during I-AT increased pulmonary strain in all three patients compared to CPAP-AT.
Pulmonary strain is defined as the relation between tidal volume and residual functional capacity (VT/FRC) and reflects the deformation that the alveolar surface undergoes during inspi ration and expiration4. In several situations, such as acute respiratory distress syndrome (ARDS), an increase in pulmonary strain is associated with lung injury4,13. Gogniat et al. demonstrated in an experimental model of ARDS that pulmo nary strain can be measured by EIT14. Therefore, the presence of an elevated pulmonary strain at the end of I-AT could indicate potential lung in jury due to lung collapse compared to CPAP-AT, even in the absence of hypoxemia. Furthermore, this intervention enabled one of the patients to complete the test, unlike the I-AT mode, where the test had to be suspended due to hypoxemia.
At present, the I-AT method remains the most commonly employed test in the diagno sis of brain death. However, it is associated with potential complications, including hypoxemia, which can be attributed to multiple factors, such as the reduction in airway pressure causing lung collapse. Solek-Pastuszka et al. conducted a study demonstrating that CPAP-AT effectively prevents a drop in PaO2/FiO2 compared to I-AT, regardless of whether patients are hypoxemic6. This observed benefit aligns with our findings, where using CPAP-AT effectively safeguards against the decrease in EELV. These findings are particularly relevant for potential lung donors, as the use of I-AT may potentially lead to in creased pulmonary strain15,16. Therefore, it may be prudent to consider routine CPAP-AT for this subgroup of patients.
In our case series, the application of EIT pro duced results consistent with those reported by Westphal et al. where EELV remained stable dur ing CPAP-AT. In contrast, in the case of I-AT, it exhibited a gradual decline9. An innovative as pect of our study is quantifying the estimated loss of EELV and its relationship with the in crease in pulmonary strain and potential lung injury. Furthermore, to our knowledge, this is the first study utilizing EIT to assess pulmonary strain generated during the apnea test in two different modalities.
Finally, continuous monitoring of tidal ven tilation using EIT revealed the absence of ven tilatory movements during the apnea test. This situation could lead to confusion in standard clinical practice, as cardiac movements may be mistakenly interpreted as ventilatory move ments. In this scenario, EIT monitoring dis played minimal impedance variations, primar ily reflecting intrathoracic impedance changes from cardiac volume fluctuations during systole and diastole.
In conclusion, within this patient series, us ing EIT revealed that employing CPAP during the apnea test effectively mitigated lung collapse and improved pulmonary strain compared to the disconnection of iMV.














