INTRODUCTION
Aortic stenosis (AS) is the most common valvular disease in Western countries. Prevalence increases with age, reaching 4-7% in patients over 65. 1 The only effective treatment is aortic valve replacement (AVR), either via surgery or percutaneously. AVR indication is evident and recommended in symptomatic patients with severe AS, as well as in patients with impaired ventricular function despite absence of symptoms. 2-4
While it is recognized that symptoms are one of the main prognostic markers of severe AS, 5,6 some series show that natural progress in asymptomatic patients is not exempt from complications. 7,8 In addition, surgical mortality has reduced over the years, 9 and percutaneous aortic replacement has advanced. 10 This makes the risk/benefit ratio of early intervention increasingly favorable. It is also important to note that symptoms, as defined, are subjective features which are highly variable according to the pa tient. This makes them difficult to identify, especially in elderly patients.
Therefore, using biomarkers for risk stratification of patients with severe AS has become more appealing. The N-terminal fraction of the pro-B-type natriuretic peptide (NT-proBNP) is one of the most common biomarkers resulting in an adverse and more fatal prognosis when increased. 11,12
The objective of this study is to assess whether increased NT-proBNP can predict symptoms and AVR indication in patients with severe AS and preserved left ventricular ejection fraction (LVEF), initially asymptomatic.
METHODS
An observational, prospective, single-site study was conducted enrolling patients with severe AS and preserved LVEF under outpatient follow-up in the site’s Valvular Heart Disease Department, who were considered asymptomatic and had no initial indication of aortic valve replacement. Patients were enrolled from July 2017 to July 2021.
All the patients had an echocardiogram performed with the Esaote MyLab Seven equipment (Florence, Italy) with a multi-frequency probe (1.5 MHz to 2.6 MHz), and the fol lowing parameters were evaluated: aortic valve peak velocity (V max), mean pressure gradient (MG), aortic valve area (AVA) by continuity equation, LV diastolic and systolic diameters (LVDD and LVSD, respectively), left ventricular mass index (LVMI), pulmonary artery systolic pressure (PASP), and LVEF using Simpson’s biplane formula. Furthermore, the lateral wall tissue S wave (lat. S) and E/e’ ratio were determined.
Severe AS was defined as a V max ≥4 m/s, MG ≥40 mmHg, and AVA ≤1 cm2. Ventricular function was consid ered preserved if LVEF was ≥55%.
Exclusion criteria: Patients who were symptomatic upon assessment, or for whom the physical examination showed clinical signs of heart failure. Patients with suspected symptoms had an exercise stress test according to the Naughton protocol. Patients with symptoms or a systolic pressure flat curve during exercise were considered symptomatic and therefore excluded. Patients with impaired ventricular func tion (LVEF ≤55%) and dilated left ventricle (diastolic diameter >60 mm) were also excluded.
An NT-proBNP assessment was required for all patients in the site’s laboratory using Vitros 5600 equipment after the first visit.
Follow-up was performed by means of clinic visits. The primary endpoint was the AVR requirement.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation, or median and interquartile range (IQR) based on a normal or abnormal distribution, and categories are expressed as percentages. For continuous variables, group comparisons between AVR and non-AVR patients were performed using Student’s t test for normal distributions and Mann-Whitney test for abnormal distributions. Categorical variables were compared using the chi-square test or the Fisher exact test when a variable showed an absolute <5 frequency.
The univariate analysis was performed using Cox regres sion, considering AVR as the dependent variable, and both NT-proBNP and several echocardiographic parameters as predictive variables. Those variables that were significant for the univariate analysis (considering p<0.05) were analyzed using a multivariate model through the proportional hazards regression method to assess variables that are independently associated with the AVR requirement.
Then, receiver operating characteristic (ROC) curves were developed, with the corresponding area under the curve (AUC), and the best cutoff point was established for significant variables in the multivariate analysis.
Finally, an event-free survival test was performed using the Kaplan-Meier method.
Statistix 7 and Epidat 3.1 softwares were used for the analysis.
RESULTS
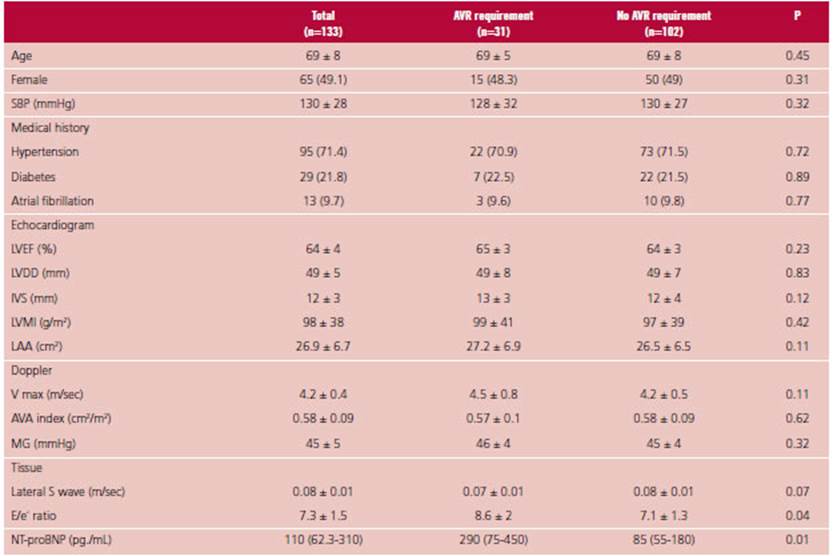
One hundred seventy-five patients were evaluated, 27 of whom were excluded as they were considered symptomatic (19 upon the initial interview, and 8 after an exercise stress test); 13 patients had im paired ventricular function, and 2 could not have an NT-proBNP assessment. Therefore, 133 patients aged 69 ± 8 were enrolled, 49% were female (n=65). The most common cause of AS was sclerodegenerative aortic valve (70%, n=93), followed by bicuspid (25.5%, n=34) and rheumatic (4.5%, n=6) aortic valve. Table 1 shows the patients’ clinical and echocardiographic characteristics.
The median follow-up was 570 days (IQR 380-680), and 23.3% (n=31) of patients required an AVR. As observed in Table 1, the group requiring AVR had a higher baseline NT-proBNP: 290 (IQR 75-450) vs. 85 (IQR 55-180) pg/mL, p=0.01, with a higher E/e’ ratio (8.6 ± 2 vs. 7.1 ± 1.3, p=0.04), a tendency towards a lower tissue S wave (0.07 ± 0.01 m/s vs. 0.08 ± 0.01 m/s, p=0.07), and no difference for the remaining parameters.
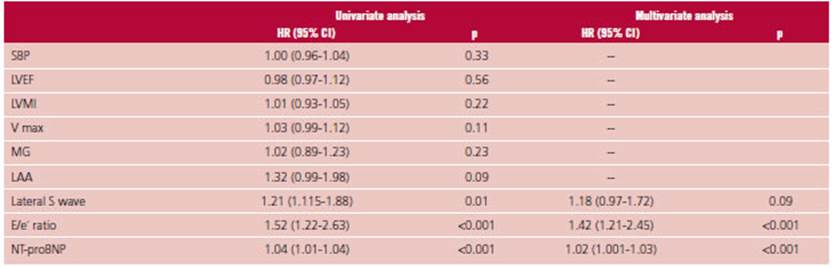
Table 2 shows the univariate and multivariate analysis. In the univariate analysis, NT-proBNP, the E/e´ ratio and lat. S were predictors of the AVR requirement. In the multivariate analysis, NT-proBNP and E/e´ ratio were independent predictors of the surgery requirement: HR 1.02 (95% CI 1.001-1.03), p<0.001, and HR 1.42 (95% CI 1.21-2.45), p<0.001, respectively.
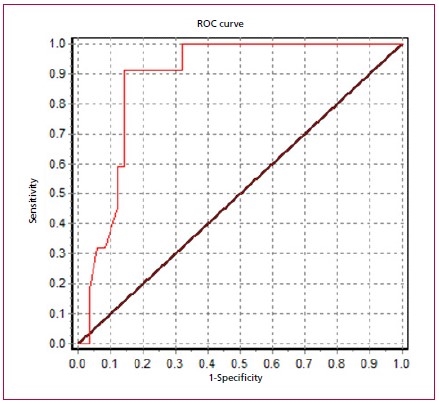
The AUC for NT-ProBNP was 0.88 (95% CI 0.81- 0.91), and the best cut-off point was 350 pg./mL, while the AUC for the E/e´ ratio was 0.64 (95% CI 0.52- 0.68), significantly lower than that of the NT-proBNP (p=0.02). See Figure 1.
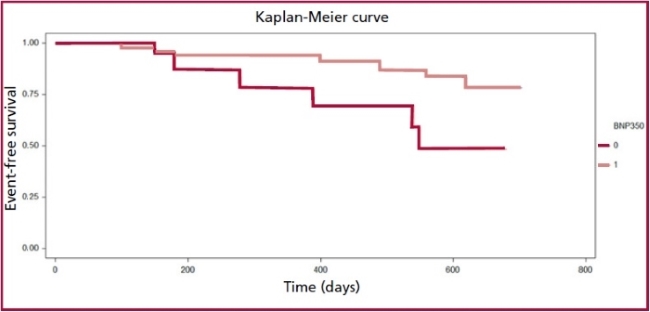
The NT-proBNP >350 pg./mL showed an adjust ed HR of 1.55 (95% CI 1.38-2.01), p<0.001. Figure 2 shows the corresponding Kaplan-Meier curve.
DISCUSSION
Our study found that an elevated NT-proBNP was associated with the AVR requirement in asymptomatic patients with severe AS and preserved ventricular function after a 1-year follow-up. The biomarker had a very good discrimination capacity (AUC 0.88), and a value higher than 350 pg./mL was associated with an increased AVR requirement higher than 50% (HR: 1.55). As acknowledged, NT-proBNP and the active BNP hormone are released in response to ventricular and/or atrial cardiomyocyte stretch, mainly as a result of increased filling pressures. 13 Several studies have previously evaluated the prognostic value of natriuretic peptides in AS. Recently, White et al. 12 published a meta-analysis to assess the prognostic role of several biomarkers in AS. They considered 33 studies evaluating the NT-proBNP in 8597 patients. In the combined analysis, an elevated NT-proBNP predicted mortality at follow-up (HR 1.73). All studies included both asymptomatic and symptomatic patients, as well as AVR and non-AVR patients.
In addition, several studies have shown that elevated BNP and NT-proBNP are associated with symp toms and a higher V max in patients with severe AS and preserved function. 14-16
As regards AS without symptoms, in 2014 Clavel et al. 11 published an observational study of nearly 2000 patients with moderate or severe AS, 560 of whom were asymptomatic at baseline. In this subgroup, an increased BNP was an independent predictor of mortality at follow-up. BNP values ≥3 times the reference value represented an adjusted risk of event nearly 4 times higher than normal BNP. In this sense, a Spanish study including 237 asymptomatic patients with mod erate and severe AS evidenced that an increased NT-proBNP was an independent predictor of events (AVR requirement, mortality) at follow-up. 17 Unlike our study, they found a mild discrimination capacity (AUC 0.62). More recently, Henri et al. evaluated the purpose of a serial BNP measurement to predict events in asymptomatic patients with severe AS. 18 An annual 20 pg./mL increase in BNP was independently associated with a growing number of events at 3-year follow-up. A retrospective study of 74 patients found that NT-proBNP and the interventricular septum thickness were independent predictors of events (mortality and AVR requirement) at 4-year follow-up. 19 Previously, Monin et al. 20 found that BNP was associated with increased events and mortality in asymptomatic patients with severe AS and an AUC 0.74. They proposed a risk score considering the BNP value, the V max, and the female sex, leading to better event prediction. This score was later validated by Farre et al., 17 using NT-proBNP instead of BNP. Based on these observations, the latest guidelines propose AVR as a Class IIA indica tion in patients with elevated natriuretic peptides. 3
In our population, 23% of patients developed symptoms and required AVR during follow-up. This rate of events is lower than the rate reported in previous studies, where about half of the patients required AVR. The Spanish group 17 reported that 110 out of 237 patients required AVR in a follow-up similar to ours. In addition, they recorded a 12% mortality. This is remarkable, since they included a group with mod erate AS. Our population was a little younger (69 versus 74 years old) and had a lower baseline NT-proBNP level (110 versus 490 pg./mL). This may partly explain the difference in events. Our patients were probably in an earlier stage of AS.
We also found that the E/e´ ratio was an independent predictor of AVR, with a mild predictive capacity (AUC 0.64). This is consistent with previous studies evaluating diastolic dysfunction parameters in AS. Especially the left atrium area (LAA) and the E/e´ ratio have been found to be independent markers of events in severe asymptomatic AS. 21,22 In our study, pa tients requiring AVR had a higher LAA than those who didn’t; however, in the multivariate analysis, LAA lost independent predictive value, due to the E/e´ ratio and NT-proBNP. Something similar happened with the tissue S wave, which was significant in the univariate but not in the multivariate analysis. The V max is another parameter associated with worse AS progress. V max >5 m/sec indicates a very severe AS, and AVR is recom mended in the absence of symptoms. 2,3 We have not found an association with the primary endpoint, probably because the average V max was 4.2 m/sec, and very few patients had a V max >5 m/sec.
The natural progress of severe AS and the time when AVR should be indicated while the disease is asymptomatic, is being increasingly discussed. The recommendation in the absence of adverse prognosis features is careful surveillance and immediate intervention as soon as symptoms occur. 2-4 The basis for this consensus is that the benefit of avoiding sudden death (1% per year in asymptomatic AS) may not be higher than AVR mortality. However, a recent retrospective study compared progress in patients with asymptomatic AS under a conservative treatment against a group of patients who had received AVR. Asymptomatic patients with no AVR at the beginning had higher mortality at 5-year follow-up than AVR patients. 23 Recently, the results of the RECOVERY study were published; 24 this study randomly as signed 145 asymptomatic patients with severe AS to early AVR versus a conservative treatment. The early AVR group had reduced events (death at surgery or within 30 days after surgery, or cardiovascular death during follow-up) versus the conservative treatment (1% vs. 15%, HR 0.09 and a large 95% CI, 0.01-0.67). However, this population was carefully picked, rela tively young (aged 64), predominantly had a bicuspid etiology, and an average V max of 5.1 m/sec. Several randomized studies are currently being conducted to evaluate the early AVR strategy for asympto matic AS: EARLY TAVR (NCT03042104), EASY-AS (NCT04204915), EVOLVED (NCT03094143) (clinicalstrials.gob).
As we have said, the value of natriuretic peptides increases with higher filling pressures. The increase in these and other biomarkers may serve to identify a subgroup of patients who, even if they are asymp tomatic, are not so well adjusted to a higher afterload caused by AS, and therefore, have worse progress. This subgroup could benefit from early intervention. 25,26 In this sense, the study by Nakatsuma et al. 27 included 380 asymptomatic patients with severe AS and ventricular function that were divided based on their baseline BNP levels. The rate of events in the group with BNP <100 pg/mL was low both after a year and after 3 years (2.1% and 6.2 %, respectively), while in the group with BNP >300 pg./mL, the rate of events was considerably higher (22% and 42% after 1 and 3 years, respectively). The results of our study contribute to the hypothesis that natriuretic peptides may be a major factor when making decisions about asymptomatic patients with severe AS and preserved function.
Limitations
Our study has several limitations. It is a single-site study, so it is difficult to extrapolate results to other populations. Follow-up was relatively short; therefore, the impact of baseline NT-proBNP cannot be assessed in the long term, and the discrimination capacity of events might be overestimated. Nevertheless, one of the objectives was to evaluate factors helping to identify patients with a higher risk that might benefit from early intervention. As a result, we believe that a 36-month follow-up is sufficient for the study objectives. Lastly, as this is an observational prospective study, the NT-proBNP value may have affected the medical decision to perform an AVR, which may also help to overestimate the event discrimination capacity of the biomarker.