Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista argentina de cardiología
versão On-line ISSN 1850-3748
Rev. argent. cardiol. vol.92 no.1 Ciudad Autónoma de Buenos Aires mar. 2024 Epub 28-Fev-2024
http://dx.doi.org/10.7775/rac.es.v92.i1.20733
SCIENTIFIC LETTER
Malignant Type 2 Endoleak: An Already Recognized Entity, But With a More Aggressive Course
Current evidence indicates that endovascular aortic aneurysm repair (EVAR) is associated with a low perioperative mortality rate and high rates of medium and long-term survival related to the aneurysm. However, the rate of reinterventions is considerable, particularly due to endoleaks, the main cause of reintervention. 1 While type I and type III endoleaks require reintervention, the clinical significance of type II endoleaks (T2EL) remains controversial. 2
Type II endoleak is defined as the presence of blood flow within the aneurysm sac after stent placement, resulting from collateral retrograde flow from the aortic branches, usually from the lumbar arteries, inferior mesenteric artery, polar renal arteries, or middle sacral artery. Most T2EL resolve spontaneously and the one-year post-operative prevalence ranges from 1-10% (defined as persistent endoleaks). However, there is evidence that persistent T2EL are associated with an increased risk of adverse outcomes (sac enlargement, aneurysm rupture, need for reintervention, conversion to open repair). A study of 832 EVAR patients found persistent T2EL accounting for 38% of secondary reinterventions. 3
Current recommendations suggest intervention for T2EL in the presence of aneurysmal growth and/or endoleak persistence; however, the exact criteria for reintervention remain undefined. 2 Some physicians argue for aggressive management, such as prophylactic embolization of patent vessels communicating with the endoleak at the time of graft implantation (intraoperative embolization), 4 while others endorse conservative monitoring approaches. 2
Although the discussion may focus on the sac size and its treatment, our presentation is based on the imaging tests findings of a specific type of T2EL. This type is more aggressive and resistant to conventional treatments such as embolization or laparoscopic ligation of collaterals.
The aim of this scientific letter is to describe a specific imaging pattern of these persistent "malignant" T2EL.
A 76-year-old male underwent endovascular repair of a ruptured abdominal aortic aneurysm using standard stent grafting in May 2016. The preoperative size of the aneurysm was 64 mm, and a significant retroperitoneal hematoma was present. The patient had favorable postoperative outcome. As predictors of T2EL, the patient had 3 patent lumbar arteries and 1 inferior polar artery exiting the aneurysm sac. At the six-month follow-up visit, the sac was excluded, the polar artery was thrombosed, and the two inferior lumbar arteries remained patent. The aneurysm sac size had decreased to 49 mm. However, one year later, the aneurysm sac increased to 58 mm, with a T2EL as the only attributable cause. Once type I and III endoleaks were ruled out, transarterial embolization of the T2EL was decided. In October 2019, EndoAnchors were placed due to persistent growth of the sac and dilation of the proximal neck. EndoArchs are endosutures or endovascular screws placed to reinforce the contact between the endograft and the arterial wall at the level of the infrarenal neck. However, due to persistent neck dilatation, a type IA endoleak developed, requiring repair with a physician-modified fenestrated endovascular graft (PMEG) (Figure 1) in October 2022. By that time the aneurysm sac had reached a size of 76 mm. The new postoperative control revealed a slight increase in the size of the sac (3 mm in 6 months) without type I or III endoleak, but with an image of a heterogeneous thrombus with central enhancement and distinct borders, which we have named 'malignant' T2EL. (Figure 2)
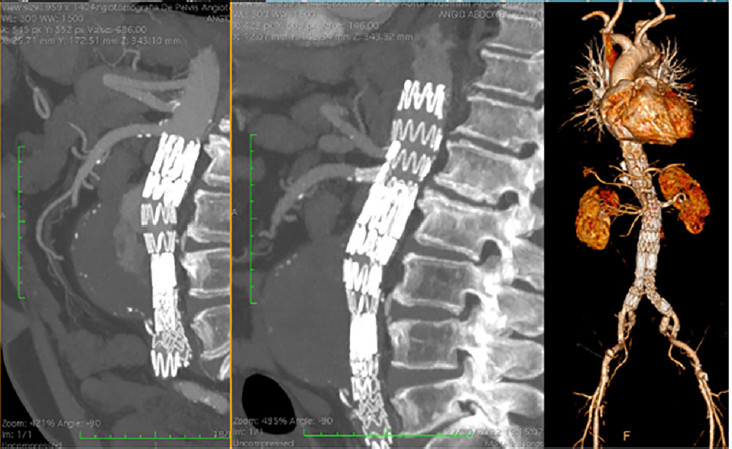
Figure 1 From left to right. Computed tomography scan before and after placement of a fenestrated stent due to type IA endoleak. 3D reconstruction of the fenestrated endograft (right).
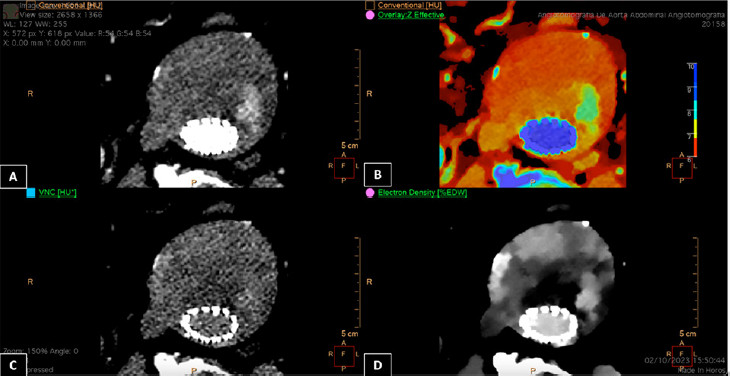
Figure 2 Four images of the aneurysm sac acquired with spectral computed tomography (iQon Spectral CT, Philips). A) Image of conventional computed tomography angiography with iodine in the arterial phase. B) Fusion image (conventional mode and iodine map). C) Virtual non contrast (VNC) mode, where by analyzing the density of the materials it is possible to virtually extract iodine. D) Image obtained by spectral analysis of electron density (ED). Electron density values in the image are expressed in percentage relative to the ED of water; the expected ED of water is 100 (%EDW). It provides a more precise characterization of the tissue and displays various densities within the thrombus, and not just the enhanced areas, that are not visible in conventional images
This patient should be managed with a conservative approach. If necessary, conversion to open surgery with sacotomy and partial resection of the aneurysm sac without graft explant may be considered as a last resort.
Among endoleaks, type II is the most common and occurs in 9-30% of patients following EVAR. Those that remain patent beyond one year postoperatively are known as persistent endoleaks. Patients with persistent T2ELs are more likely to develop sac expansion and undergo reintervention during follow-up. 2
The typical findings involve a cavity within the aneurysm, usually with one or more inflow and outflow arteries. However, the T2EL that we are describing as "malignant", has no cavity, but, on the contrary, presents irregular and diffuse contrast enhancement Fig. 1. From left to right. Computed tomography scan before and after placement of a fenestrated stent due to type IA endoleak. 3D reconstruction of the fenestrated endograft (right). Fig. 2. Four images of the aneurysm sac acquired with spectral computed tomography (iQon Spectral CT, Philips). A) Image of conventional computed tomography angiography with iodine in the arterial phase. B) Fusion image (conventional mode and iodine map). C) Virtual non contrast (VNC) mode, where by analyzing the density of the materials it is possible to virtually extract iodine. D) Image obtained by spectral analysis of electron density (ED). Electron density values in the image are expressed in percentage relative to the ED of water; the expected ED of water is 100 (%EDW). It provides a more precise characterization of the tissue and displays various densities within the thrombus, and not just the enhanced areas, that are not visible in conventional images of the aortic wall and thrombus on computed tomography angiography. For this reason, traditional endovascular treatments, such as embolization of the sac or its branches by transarterial, lumbar or transcaval routes, or even laparoscopically, are not very effective.
From a pathophysiological perspective, the vasa vasorum are the vessels associated with arterial microcirculation. The vasa vasorum comprise a vascular network that originate in the adventitial layer of large arteries from which smaller vessels branch. The outermost thirds of the great arteries receive nutrients from the vasa vasorum, while the innermost third is an avascular zone passively nourished by the luminal blood flow. Several publications have shown that endovascular stenting of an artery with a covered stent caused proliferation of the vasa vasorum from the adventitia to the intima layer. The changes that occur in vasa vasorum after EVAR and the role of developed vasa vasorum in aneurysm expansion after EVAR are currently unknown. However, there have been reports of thrombosed cerebral aneurysms that continued to grow after complete endovascular occlusion due to developed vasa vasorum. Occasionally, the organized thrombus may exhibit heterogeneous contrast enhancement, as in the case described, and this expanding thrombus is referred to as chronic expansive hematoma (CEH). 5 Enhancement of the aneurysm wall is through the network of small arteries, which could correspond to vasa vasorum. The heterogeneous and patchy enhancement of the intrasaccular thrombus, without the typical endoleak cavity, was considered analogous to the findings of CEH.
The use of the IQon Spectral CT (Philips Healthcare Inc., The Netherlands) is another remarkable feature. The images in Figure 2 display the spectral analysis of electron density, highlighting the varying densities within the thrombus in contrast-enhanced CT angiography. This makes the areas of post-contrast enhancement more evident. 6
To the best of our knowledge, these findings have not been previously reported. Although we are presenting a clinical case and our experience with ten additional cases, we believe that the imaging findings of 'malignant' T2EL may be useful for managing these cases. The visualization of the sac with heterogeneous and patchy enhancement of the thrombus could be distinctive findings in these cases.
REFERENCES
1. Schanzer A, Greenberg RK, Hevelone N, Robinson WP, Eslami MH, Goldberg RJ, et al. Predictors of abdominal aortic aneurysm sac enlargement after endovascular repair. Circulation. 2011;123:2848- 55. https://doi.org/10.1161/CIRCULATIONAHA.110.014902 [ Links ]
2. Chaikof EL, Dalman RL, Eskandari MK, Jackson BM, Lee WA, Mansour MA, et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018;67:2-77.e2. https://doi.org/10.1016/j.jvs.2017.10.044 [ Links ]
3. Conrad MF, Adams AB, Guest JM, Paruchuri V, Brewster DC, LaMuraglia GM, et al. Secondary intervention after endovascular abdominal aortic aneurysm repair. Ann Surg. 2009;250:383-9. https://doi.org/10.1097/SLA.0b013e3181b365bd [ Links ]
4. Fabre D, Mougin J, Mitilian D, Cochennec F, Garcia Alonso C, Becquemin JP, et al. Prospective, Randomised Two Centre Trial of Endovascular Repair of Abdominal Aortic Aneurysm With or Without Sac Embolisation. Eur J Vasc Endovasc Surg. 2021;61:201-9. https://doi.org/10.1016/j.ejvs.2020.11.028 [ Links ]
5. Pahl FH, Vellutini Ede A, Cardoso AC, de Oliveira MF. Vasa Vasorum and the Growing of Thrombosed Giant Aneurysm of the Vertebral Artery: A Case Report. World Neurosurg. 2016;85:368.e1-4. https://doi.org/10.1016/j.wneu.2015.09.103 [ Links ]
6. Kazimierczak W, Kazimierczak N, Lemanowicz A, Nowak E, Migdalski A, Jawien A, et al. Improved Detection of Endoleaks in Virtual Monoenergetic Images in Dual-Energy CT Angiography Following EVAR. Acad Radiol. 2023;30:2813-24. https://doi.org/10.1016/j.acra.2023.03.018 [ Links ]











 texto em
texto em 



