Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista argentina de cardiología
versão On-line ISSN 1850-3748
Rev. argent. cardiol. vol.92 no.1 Ciudad Autónoma de Buenos Aires mar. 2024 Epub 28-Fev-2024
http://dx.doi.org/10.7775/rac.es.v92.i1.20731
SCIENTIFIC LETTER
What Are the Potential Determinants of Favorable Long-term Outcomes Following Drug-coated Balloon Treatment? Gathering Data from a Single Observation
1Department of Cardiology, University of Galway, Galway, Ireland
2Department of Mechanical Engineering, Melbourne School of Engineering, University of Melbourne, Victoria, Australia
3Cardio Center, IRCCS, Humanitas Research Hospital, Rozzano, Milan, Italy
Coronary angiography of a 58-year-old man with angina showed a de novo stenosis in the mid left circumflex coronary artery (LCX) with a minimum lumen diameter (MLD) and reference diameter (RD) of 1.20 and 2.44 mm, respectively. Quantitative flow ratio (QFR, Medis) was 0.80 distal to the lesion (Figure 1A and 1B). Optical coherence tomography (OCT) was performed after pre-dilatation, prior to drug-coated balloon (DCB) treatment for selection of an appropriately calibrated size DCB and to assess the extent of the barotrauma pre DCB.
The patient was loaded with prasugrel 60 mg in addition to his daily chronic aspirin therapy. Initially, pre-dilatation was performed with a semi-compliant 2.5×20 mm balloon inflated at 6 atmospheres resulting in an angiographically type B dissection without impaired distal flow. OCT disclosed a dissection with a length of 12.6 mm extending to the media; the RD was 2.55mm and the minimal lumen area (MLA) 2.36 mm2 after pre-dilatation; the DCB treatment was successfully performed with SeQuent Please NeoTM paclitaxel coated balloon (PCB) (2.5 × 30 mm) inflated for 60 seconds. The transit time, duration from insertion of DCB into the sheath until DCB inflation, was 45 seconds. Acute gain was 0.6 mm (MLD pre-procedure vs MLD post-DCB: 1.20 vs 1.80 mm) and post-DCB QFR was 0.91 (Figure 1C and 1D). Dual antiplatelet therapy (DAPT) with a maintenance dose of 10 mg of prasugrel was prescribed at discharge.
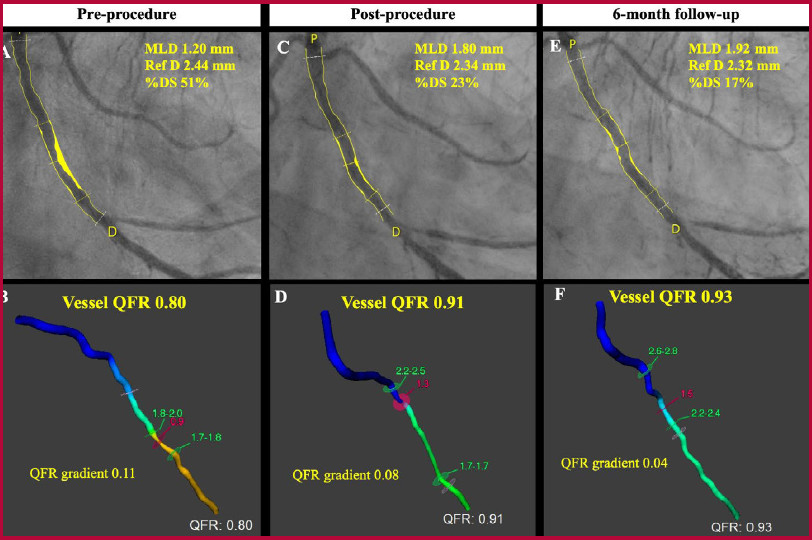
Figure 1 Serial change of MLD and QFR following drugcoated balloon. MLD and QFR pre-procedure (A and B), post-procedure (C and D), and at 6-month follow- up (E and F). DS=Diameter stenosis; MLD= Minimum lumen diameter; QFR= Quantitative flow ratio; Ref D= Reference diameter
The 6-month angiography showed a late lumen gain (LLG) of 0.12 mm at the site of the MLD post-DCB with a healed dissection (Figure 1E). The QFR at 6-month follow-up was 0.93 (Figure 1F).
DCB treatment in this case resulted in an expansive remodeling. Comprehensive assessments of determinants of long-term outcome, including physiological and morphological features, were retrospectively performed.
Type of drug, and drug transfer
Limus drugs are cytostatic, while paclitaxel is a cytotoxic drug, which means it essentially induces smooth muscle cell death and has potential for toxicity. Clinical data from randomized clinical trials of DCBs are primarily based on studies of PCB putatively related to their favorable pharmacokinetic properties. 1,2 It is not clear whether the effect of vessel remodeling is exclusive for paclitaxel or whether it can also be seen with sirolimus or biolimus A9. In our case, an adequate drug transfer of paclitaxel after a short transit time of 45 seconds potentially could contribute to the late lumen enlargement (LLE).
Dissection
The degree of lesion expansion will be associated with the extent of dissection. Some studies demonstrated the relationship between non-flow limiting larger dissection during PCB treatment and the LLG or enlargement. 3 The mechanism might be explained by vessel growth (expansive remodeling) induced by a direct exposure to paclitaxel delivered into the adventitia and/or plaque regression induced by an intensive lipid-lowering therapy. In this case, flap type dissection extending to the media was observed; the maximum dissection arc was 153 degrees, and the total dissection volume was 13.8 mm3 (Figure 2A).
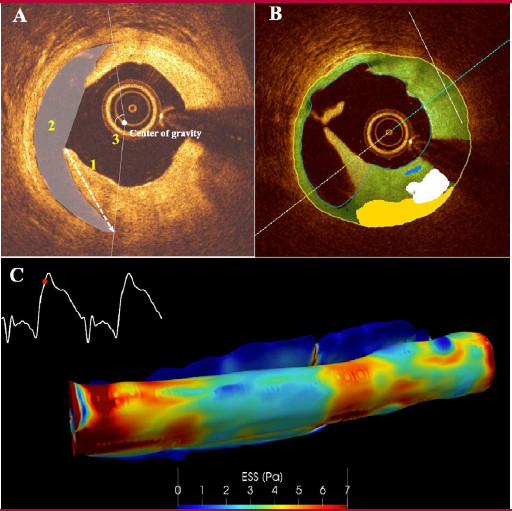
Figure 2 Extent of the barotrauma following DCB treatment. (A) Precise quantification of dissection volume derived from cross-sectional slices with a thickness of 100 microns. (B) OCT deep learning analysis using OctPlus software (Pulse, Shanghai). (C) Wall shear stress derived from the fusion of OCT and angiography. DCB= drug-coated balloon; OCT= optical coherence tomography
Tissue composition
The tissue composition of the target lesion must have implication on the site of fracture, the extent of dehiscence of the intima from the media and adventitia, on the drug transfer at the time of the procedure, and later on the process of late lumen loss (LLL) or LLG. In this case, the tissue components of vessel wall plaque within the target lesion were identified by OCT deep learning (OctPlus, Pulse, Shanghai). 4 The distribution of fibrous, lipid, calcium plaque, and macrophage/ crystal-cholesterol were 89.5%, 3.7%, 6.4%, and 0.6% (Figure 2B). The fact that fibrous plaque is predominant in this lesion may have been associated with greater dissection, adequate drug transfer and subsequent favorable outcomes.
Wall shear stress
Figure 2C shows a great heterogeneity of high and low shear stress derived from the fusion of OCT and angiography in a Computational Fluid analysis based on the Navier Stoke and Quemada equations after finite element analysis. 5 In the dissected area low shear stress dominates and is associated with high viscosity prone to thrombosis. This pattern of shear stress is at total variance with the homogeneous profile usually seen after a well deployed stent implantation. Further investigations are warranted to understand the favorable or unfavorable impact of shear stress on outcome.
Post procedural physiological assessment
Although QFR >0.91 after stent implantation could predict a favorable vessel-oriented composite endpoint, only scarce evidence of prognostic value of QFR post procedure exists in patients treated with DCB. 6 In our case, the QFR gradually increased: 0.80 at procedure, 0.91 at post procedure, and 0.93 at 6-month follow-up.
In conclusion, the determinant of favourable outcomes following DCB treatment are multifactorial. Previous studies as well as our case report illustrate the numerous potential factors affecting outcomes after DCB treatment, and their positive and/or negative impact, as well as their complex interplay, need further study
REFERENCES
1. Lemos PA, Farooq V, Takimura CK, Gutierrez PS, Virmani R, Kolodgie F, et al. Emerging technologies: polymer-free phospholipid encapsulated sirolimus nanocarriers for the controlled release of drug from a stent-plus-balloon or a stand-alone balloon catheter. EuroIntervention. 2013;9:148-56. https://doi.org/10.4244/EIJV9I1A21 [ Links ]
2. Ahmad WAW, Nuruddin AA, Abdul Kader MASK, Ong TK, Liew HB, Ali RM, et al. Treatment of Coronary De Novo Lesions by a Sirolimus- or Paclitaxel-Coated Balloon. JACC Cardiovasc Interv. 2022 Apr 11;15(7):770-779. https://doi.org/10.1016/j.jcin.2022.01.012. Epub 2022 Mar 16. PMID: 35305906.. [ Links ]
3. Yamamoto T, Sawada T, Uzu K, Takaya T, Kawai H, Yasaka Y. Possible mechanism of late lumen enlargement after treatment for de novo coronary lesions with drug-coated balloon. Int J Cardiol. 2020;321:30-7. https://doi.org/10.1016/j.ijcard.2020.07.028 [ Links ]
4. Chu M, Jia H, Gutiérrez-Chico JL, Maehara A, Ali ZA, Zeng X, et al. Artificial intelligence and optical coherence tomography for the automatic characterisation of human atherosclerotic plaques. EuroIntervention. 2021;17:41-50. https://doi.org/10.4244/EIJD-20-01355 [ Links ]
5. Thondapu V, Tenekecioglu E, Poon EKW, Collet C, Torii R, Bourantas CV, et al. Endothelial shear stress 5 years after implantation of a coronary bioresorbable scaffold. Eur Heart J. 2018;39:1602-9. https://doi.org/10.1093/eurheartj/ehx810 [ Links ]
6. Yamamoto T, Ishii T, Ishida A. Impact of post physiological assessment after treatment for de novo coronary lesions using drug-coated balloons. Int J Cardiol. 2022;363:11-9. https://doi.org/10.1016/j.ijcard.2022.06.009 [ Links ]
Ethical considerations The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient in line with COPE guidance.











 texto em
texto em 



