Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista argentina de cardiología
versão On-line ISSN 1850-3748
Rev. argent. cardiol. vol.92 no.1 Ciudad Autónoma de Buenos Aires mar. 2024 Epub 28-Fev-2024
http://dx.doi.org/10.7775/rac.es.v92.i1.20738
IMAGES IN CARDIOLOGY
Pulmonary Thromboembolism and Takotsubo Syndrome as Causes of Cardiopulmonary Arrest
1Cardiovascular Critical Care Unit, Hospital de Clínicas José de San Martín Buenos Aires, Argentina.
Venous thromboembolism (VTE), with pulmonary embolism (PE) as its most serious manifestation, is the third leading cause of in-hospital mortality. The thrombus usually comes from the veins of the lower limbs. Virchow's triad of venous stasis, hypercoagulability and endothelial injury usually triggers the pathophysiologic cascade that contributes to the development of venous thrombosis. 1
Stress cardiomyopathy or takotsubo syndrome presents as an acute, transient and reversible left ventricular dysfunction, often related to an emotional or physical stressful event producing a reduction in cardiac output. Most cases occur in postmenopasual women > 55 years. Patients may be asymptomatic or present serious symptoms due to heart failure. 2,3
Pulmonary embolism has been reported as a physical and psychological trigger for stress cardiomyopathy. The combination of these two factors, which have been extensively described and studied in the literature, can be catastrophic for the patient and result in a high mortality rate. 2
This situation is of the utmost interest due to the combination of these factors, the severity of the condition, the high clinical suspicion, and the role of bedside echocardiography in identifying this type of event and enabling prompt intervention to minimize consequences and mortality.
We present a 65-year-old female patient with a history of hypertension, hypothyroidism, smoker of 20 packsyear, and dermatomyositis with involvement of the skin, joints and lungs.
She was admitted with fractures on the left side, one in the femoral shaft and the other in the proximal humerus. During hospitalization, the patient evolved with septic shock due to urosepsis and was transferred to the critical care unit. Four days after being admitted, she developed cardiac arrest with ventricular fibrillation and required basic and advanced cardiopulmonary resuscitation for four minutes.
Thereafter, an echocardiogram was performed, which showed akinesis of the mid and apical segments with hypercontractility of the basal segments, and severe left ventricular dysfunction (left ventricular ejection fraction 33%). The right ventricle was slightly dilated with decreased systolic function and tricuspid annular plane systolic excursion (TAPSE) of 10 mm (Figure 1). There was a mobile hyperechogenic image in the right atrium swinging between the inferior vena cava and the right atrium, which could correspond to a thrombus in transit.
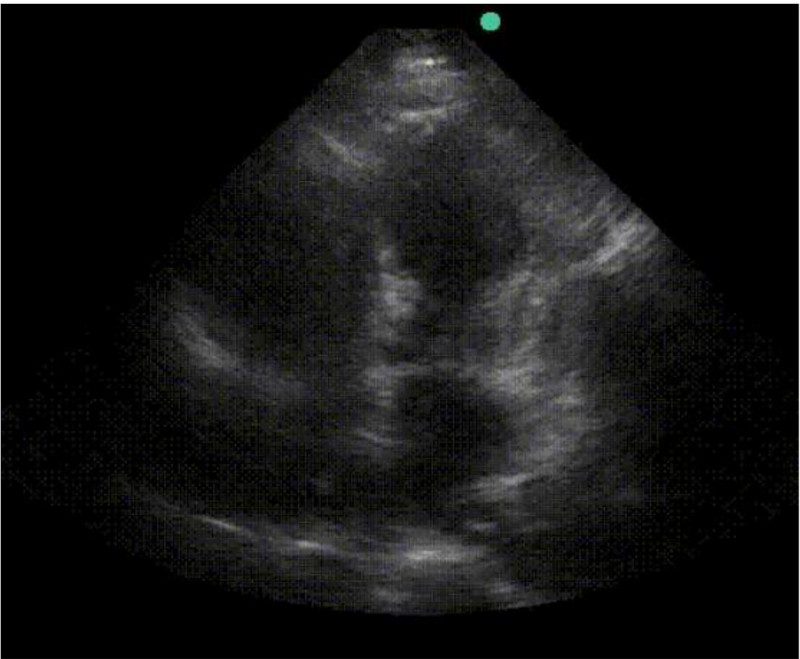
Fig. 1 Four-chamber apical view. Depressed contractility in mid an apical segments with normal wall motion in basal segments. The right chambers are dilated and the septum is flattened.
She was managed with Alteplase and anticoagulation, and the hemodynamic status improved. (Figure 2) The patient underwent coronary angiography and left ventriculography. The coronary arteries showed no significant obstructions but the ventriculography evidenced apical ballooning (Figure 3). The cause of cardiac arrest was interpreted as pulmonary embolism combined with stress cardiomyopathy. The patient had a favorable clinical course. An echocardiogram performed 10 days later revealed complete improvement of the systolic function in both ventricles, normal wall motion and absence of thrombus in transit.

Fig. 2 Subcostal view. The arrowhead shows a hyperechogenic image in transit between the inferior vena cava and the right atrium, suggestive of a thrombus in transit.
BIBLIOGRAFIA
1. Ubaldini J, Bilbao J, Spenatto MC, Bonorino J, Flores LA, Kenar M, et al. Consenso de Enfermedad Tromboembólica Aguda. Rev Argent Cardiol. 2016;84:74-91. https://doi.org/10.7775/rac.es.v84.i1.7739 [ Links ]
2. Jin Q, Luo Q, Zhao Z, Zhao Q, Yu X, Yan L, et al. Takotsubo syndrome with pulmonary embolism: a case report and literature review. BMC Cardiovasc Disord. 2018;18:229. https://doi.org/10.1186/s12872-018-0953-7 [ Links ]
3. Challa S, Ganji J, Raizada A, Najib M, Panse P, Chaliki, H. Takotsubo cardiomyopathy in a patient with pulmonary embolism. Eur J Echocardiogr. 2011;12:E39. https://doi.org/10.1093/ejechocard/jer151 [ Links ]











 texto em
texto em 



