INTRODUCTION
Apical periodontitis (AP) is an inflammatory condition of periapical tissues, and one of the most common infectious diseases in the world 1-3 . When the root canal treatment fails, post-treatment AP may set in or persist and lead to tooth loss. Persistent, secondary, or extra-radicular infections are the leading causes of endodontic treatment failure 2 , 3 . Epidemiological studies have traditionally used periapical and panoramic radiographs to follow up endodontic treatment and determine possible variables associated with post-treatment AP. However, these radiographic examinations have limitations such as the superimposition of the overlying anatomy, the two-dimensional nature of the image, and the geometric distortion 4 . These deficiencies have been partly overcome by cone-beam computed tomography (CBCT) due to its high sensitivity to assess three-dimensional changes in dental tissues and supporting structures 5 , the quality of endodontic fillings, and hypodense bone lesions. It can also be used to evaluate different visual planes with slices as thin as 0.5 mm or less 6 .
Recent epidemiological studies using CBCT in Scotland, Brazil, France, Belgium, Germany, and Portugal confirmed the high prevalence of post-treatment AP, ranging from 40.8% to 55.5% 7-12 . In addition, a systematic review and meta-analysis of cross-sectional studies showed that 41.3% of endodontically treated teeth had post-treatment AP, on average. AP was significantly more frequent in teeth with both inadequate endodontic treatment and poor coronal restoration 13 .
A risk factor for post-treatment AP is the inability of the clinician to locate all the root canals. Missed canals may harbor enough bacteria to maintain or lead to apical periodontitis. Even when initially uninfected, a missed canal becomes a susceptible site for infection 14 . Studies conducted in North America, Brazil, Portugal, and Saudi Arabia have reported a strong association between a missed canal and the presence of AP, with frequencies ranging from 12% to 23%, and 2.57 to 6.25 times more risk of presenting AP than teeth in which all canals have been treated 14-18 . However, these studies focused mainly on the missed canal variable, which could be considered a selection bias, given the greater number of teeth with AP in which all canals were treated 19 .
It is not clear whether the presence of a missed canal would remain statistically significant in a multivariate analysis with a large set of variables, including those known to have a significant impact on treatment prognoses, tooth type, and quality of endodontic treatment 19 . Considering this context and the limited number of studies in the Latin American population, the present study evaluated the relation between the quality of endodontic treatment and the frequency of missed canals associated with teeth presenting AP through CBCT in a Colombian sub-population. The frequencies were determined for all tooth types.
MATERIALS AND METHOD
This research was conducted under the principles established by Resolution 08430 of the Government of Colombia and approved by the Ethics Committee of Santo Tomás University.
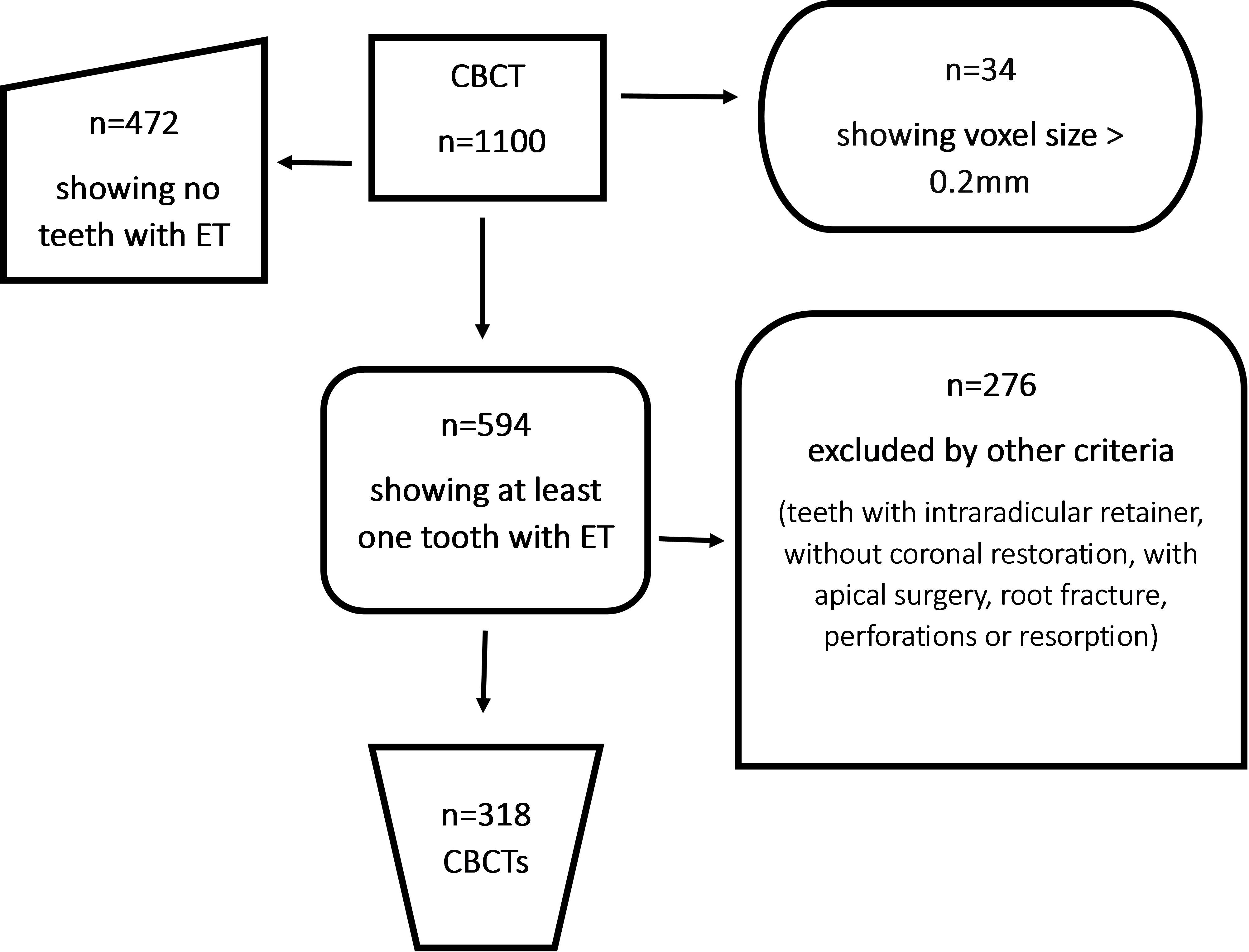
A cross-sectional study was conducted. A database of 1100 CBCT scans of Colombian individuals (n=318: 190 females and 128 males) was analyzed. Scans showing at least one endodontically treated tooth and voxel size between 0.125 and 0.20 mm were selected (594), while scans not showing endodontic treatment (472) or with voxel size greater than 0.20 mm (34) were excluded. Ofthe 594 selected scans, 276 were discarded due to artifacts, teeth without coronal restoration, or teeth with intra-radicular retainer, apical surgery, root fracture, perforations or resorption, leaving 318 CBCTs for study ( Fig. 1 ). The CBCTs were obtained from two private radiology centers, one in Bucaramanga and another in Medellin. The scans were taken between June 2017 and June 2020, using two J Morita X550 CBCT Scanners (J Morita Corporation, Osaka, Japan): 127V, 50/60 Hz and 4 A panoramic X-ray, and three different FOV sizes: small (up to 5 cm), single arc (5 to 7 cm), and inter-arc (7 to 10 cm) 20 . The I-Dixel One volume viewer software (J. Morita) was used. The tomographic images included in the database were requested for reasons beyond the scope of this research.
All dental types were evaluated. In multirooted teeth, each root was evaluated independently, centered, and aligned in sagittal and coronal planes, obtaining the most centered image to determine treatment quality based on the following criteria: Adequate Endodontic Treatment (AET), apical obturation limit between 0-2 mm from the root apex, and homogeneous compaction of filling mass; or Inadequate Endodontic Treatment (IET), apical obturation ending more than 2 mm from the apex or extruded gutta-percha, or poorly compacted root canal filling 21 . Missed canals were considered when there was a hypodense image, similar to a root canal, but without evidence of filling material, Crossing the tooth root vertically, from the cervical region to the root apex 15 , and they were also classified as IET 11 . AP was defined according to the cone-beam computed tomographic-endodontic radiolucency index (ERI), as a hypodense zone associated with the root apex greater than 0.5 mm in a coronal-sagittal view; length measured in millimeters in the vestibule-palatine or lingual direction and the mesial-distal direction, tracing a perpendicular from the root apex to the upper limit of the radiolucent area in its greatest extension 6 .
Two endodontic specialists independently analyzed all samples. An oral and maxillofacial radiology specialist decided on discordant cases to identify the quality of the ET, the presence of missed canal, and the presence of AP. The observers’ accuracy in detecting missed canals and AP was initially gauged with a pilot test of 100 images and using Cohen kappa intra and inter-evaluator reliability tests 22 , the kappa concordance coefficient obtained was higher than 90% intra-evaluator and between 95.34 and 96.1% inter-evaluator for both evaluators, a satisfactory data reliability result.
Statistical analysis
The data were recorded using the Microsoft Excel software database (Microsoft Corp., LA, USA) and entered into the STATA 14.2 software (StataCorp LP, College Station, TX, USA). Absolute frequencies and percentages were calculated for qualitative variables. The proportion of AP in each group was calculated and expressed with a 95% confidence interval (CI). The presence of AP was related to the explanatory variables (quality of the filling, presence of missed canal, and tooth type) using the chi-square test or Fisher’s exact test for proportions and analysis of group differences. P-value < 0.05 was considered significant. The odds ratio (OR) was calculated to analyze the odds that AP occurs in teeth with missed canal or IET compared to teeth with all canals treated or AET, respectively.
RESULTS
The frequency of AP was 62.34% (288/462); 27.43% (n = 79) of teeth with AET, and 72.57% (n = 209) of teeth with IET, a statistically significant result (p < 0.01, Table 1 ).
The 288 teeth with AP and 174 without AP were distributed as follows: for teeth with IET, 60.76% had AP without missed canal, compared to 39.23% with AP and missed canal, with a statistically significant difference (p < 0.01, Table 2 ). In this study, 18.61% of endodontically treated teeth had a missed canal, of which 95.3% had AP compared to a prevalence of AP of 54.7% for teeth without a missed canal ( Table 3 ). Concerning dental groups, multi-rooted teeth had the highest frequency of missed canal, with maxillary molars showing the highest percentage (55.23%, 58/105). The presence of AP in these teeth was 96.55% (56/58) ( Table 3 ). In the mesiobuccal (MB) roots of maxillary molars, the MB2 canal was the most frequently missed canal (88.52%, 54/61), with 90.74% being associated with AP (49/54) ( Table 4 ).
Table 1 Frequency of apical periodontitis according to the quality of endodontic treatment
| Endodontic Treatment Quality N (%) | Apical Periodontitis | ||||
|---|---|---|---|---|---|
| Yes (n) | % | No (n) | % | ||
| Adequate (AET) | 207 (44.81) | 79 | 27.43 | 128 | 73.56 |
| Inadequate (IET) | 255 (55,19) | 209 | 72.57* | 46 | 26.43 |
| Total | 462 | 288 | 62.34 | 174 | 37.66 |
Table 2 Frequency of AP according to the presence or absence of missed canals in teeth with inadequate endodontic treatments (IET)
| Sealing quality | N (%) | Presence of apical periodontitis | |||
|---|---|---|---|---|---|
| Yes | % | No | % | ||
| (n) | (n) | ||||
| IET and missed canal | 86 | 82 | 39.23 | 4 | 8.69 |
| IET without missed canal | 169 | 127 | 60.76* | 42 | 91.31 |
| Total | 255 | 209 | 100 | 46 | 100 |
Table 3 Association between presence of missed canals and apical periodontitis (AP) in types of teeth
| Sample | Missed canal | Missed canal | Without missed canal | Without missed canal | |||
|---|---|---|---|---|---|---|---|
| Types of Teeth | Teeth with ET | n (%) | With AP n (%) | Without AP n (%) | n (%) | With AP n (%) | Without AP n (%) |
| Maxillary | |||||||
| Central | 48 | 1 (2.12) | 1 (100) | -.- | 47 (97.87) | 22 (46.81) | 25 (53.19) |
| Lateral | 49 | -.- | -.- | 49 (100) | 27 (55.10) | 22 (44.90) | |
| Canine | 31 | -.- | -.- | 31 (100) | 13 (41.94) | 18 (58.06) | |
| Premolar | 101 | 10 (9.90) | 8 (80) | 2 (20) | 91 (90.10) | 54 (59.34) | 37 (40.65) |
| 1st Molars | 71 | 44 (61.9) | 42 (95.4) | 2 (4.5) | 27 (38.1) | 20 (74) | 7 (26) |
| 2nd Molars | 34 | 14 (41.1) | 14 (100) | -.- | 20 (58.82) | 13 (65) | 7 (35) |
| Mandibular | -.- | ||||||
| Central | 5 | -.- | -.- | 5(100) | 2 (40) | 3 (60) | |
| Lateral | 5 | -.- | -.- | 5 (100) | 3 (60) | 2 (40) | |
| Canine | 4 | -.- | -.- | 4 (100) | -.- | 4 (100) | |
| Premolar | 32 | 2 (6.25) | 2 (100) | -.- | 30 (93.75) | 9 (30) | 21 (70) |
| 1st Molars | 53 | 10 (18.8) | 10 (100) | -.- | 43 (81.13) | 29 (67.44) | 14 (32.55) |
| 2nd Molars | 29 | 5 (17.24) | 5 (100) | -.- | 24 (82.75) | 14 (58.33) | 10 (41.66) |
| Total | 462 | 86 (18.6) | 82 (95.3) | 4 (4.7%) | 376 (81.39) | 206 (54.7%) | 170 (42.3%) |
Teeth with endodontic treatment but with missed canals had a crude OR: 16.9 (95% CI, 6.07 -47.10) to be associated with an AP, indicating a greater probability. In addition, according to the statistical significance found in the maxillary and mandibular molar teeth groups in the bivariate analysis, the logistic regression model adjusted for the variable type of tooth found an OR: 10.5 (95% CI 3.61- 30.86). Similarly, the groups of teeth with a statistically significant risk association were maxillary molars, OR :2.5 (95% CI 1.25-5.02), and mandibular molars, OR: 1.96 (95% CI 1.07-3.59), suggesting that a maxillary molar with missed canal had a 2.5-fold risk of having AP, and a mandibular molar with missed canal had a 1.96-fold risk of having AP when a missed canal was present ( Table 5 and 6 ).
DISCUSSION
Several studies have investigated the prevalence of AP in teeth with endodontic treatment and its risk factors 23 , 24 ; however, they have used 2D images, which have disadvantages compared to 3D images. Due to its high sensitivity, CBCT can more accurately evaluate the presence of AP 25 , the quality of the endodontic treatment, and the presence of missed canals 14-16 . For example, a study conducted in Colombia in 2013 found an AP prevalence of 49% using 2D images for endodontic treatments 21 , whereas the current study using CBCT found a higher prevalence of AP (62.34%), similar to recent CBCT studies that found AP between 51.8% and 88% 14-16 .
A noteworthy aspect of the current study is the evaluation of a significant variable, the quality of endodontic treatment, in addition to the presence of missed canals. It was observed that 27.43% of teeth with Adequate Endodontic Treatment (AET) and 72.57% of teeth with Inadequate Endodontic Treatment (IET) presented Apical Periodontitis (AP). This suggests that the presence of missed canals is not the sole factor associated with AP. In fact, 60.76% of teeth with IET and all canals treated had AP, compared to 39.23% of teeth with IET and missed canals. This finding could address the letter to the editor by Leprince & Nieuwenhuysen 19 , who, after pooling data from the most relevant studies on missed canals 14-16 , showed that 81.8% of all evaluated teeth presented AP and had all canals treated. Only 18.2% had presence of AP in teeth with missed canals. This corroborates the idea that multiple variables are associated with the presence of AP.
Furthermore, the current study found 18.61% of missed canals, similar to previous studies, which reported 12% to 23% 14-18 . Also, in the present study, 95.3% of missed canals had AP, comparable with previous studies 14-16 , which found 82.8%, 82.6%, and 98%, respectively.
Table 4 Association between presence of missed canal and apical periodontitis (AP) in the root and canals of maxillary and mandibular molars
| With missed canal | Without missed canal | ||||||
|---|---|---|---|---|---|---|---|
| Root canals | Sample | With missed canal | AP | Without missed canal | AP | ||
| Yes | No | Yes | No | ||||
| N | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Maxillary molars | |||||||
| 1st molar | |||||||
| Mesiobuccal root | |||||||
| Mesiobuccal canal | 71 | 1 (1.40) | 1 (100) | -.- | 70 (98.59) | 53 (75.71) | 17 (24.28) |
| Mesiobuccal 2 canal | 50 | 43 (86) | 39 (90.69) | 4 (9.30) | 7 (14) | 5 (71.42) | 2 (28.57) |
| Distobuccal root | |||||||
| Distobuccal canal | 71 | 3 (4.22) | 2 (80) | 1 (20) | 68 (95.77) | 30 (44.11) | 38 (55.88) |
| Palatal root | |||||||
| Palatal canal | 71 | -.- | -.- | -.- | 71 (100) | 32 (45.07) | 39 (54.92) |
| 2nd molar | |||||||
| Mesiobuccal root | |||||||
| Mesiobuccal canal | 28 | 2 (7.14) | 2 (100) | -.- | 26 (92.85) | 19 (73.07) | 7 (26.92) |
| Mesiobuccal 2 canal | 11 | 11 (100) | 10 (90.9) | 1 (9.1) | -.- | -.- | -.- |
| Distobuccal root | |||||||
| Distobuccal canal | 28 | 2 (4.14) | 2 (100) | -.- | 26 (92.85) | 13 (50) | 13 (50) |
| Palatal root | |||||||
| Palatal canal | 28 | -.- | -.- | -.- | 28 (100) | 15 (53.57) | 13 (46.42) |
| Mandibular molars | |||||||
| 1st molar | |||||||
| Mesial root | |||||||
| Mesiobuccal canal | 51 | 2 (3.92) | 2 (100) | -.- | 49 (96.07) | 28 (57.14) | 21(42.85) |
| Mesiolingual canal | 51 | 2 (3.92) | 2 (100) | -.- | 49 (96.07) | 29 (59.18) | 20 (40.81) |
| Distal root | -.- | ||||||
| Distobuccal canal | 14 | 6 (42.85) | 6 (100) | -.- | 8 (57.14) | 5 (62.5) | 3(37.5) |
| Distolingual canal | 14 | 3 (21.42) | 3 (100) | -.- | 11 (78.57) | 8 (72.72) | 3 (27.27) |
| 2nd molar | |||||||
| Mesial root | |||||||
| Mesiobuccal canal | 19 | 2 (10.52) | 2 (100) | -.- | 17 (89.47) | 10 (58.82) | 7(41.17) |
| Mesiolingual canal | 19 | 4 (21.05) | 4 (100) | -.- | 15 (78.94) | 8 (53.33) | 7 (46.66) |
| Distal root | |||||||
| Distobuccal canal | 2 | -.- | -.- | -.- | 2 (100) | 2 (100) | -.- |
| Distolingual canal | 2 | -.- | -.- | -.- | 2 (100) | 2 (100) | -.- |
Maxillary molars were the teeth with the highest frequency of missed canals, with 55%, similar to prior reports of 40.1% 14 , 15 . Another study found 59.55% and 40% missed canals in maxillary first and second molars, respectively 16 , while the present study found similar results for the first and second maxillary molars, with 61.97% and 41.18%, respectively. The reason for the high percentage of missed canals may be the presence of a second mesial buccal (MB) canal in 88.5% of maxillary first molars and 83.4% of second molars 25 . The MB root has complex anatomy that usually presents Vertucci configurations type II (69.1%) 26 and type IV (48.7%) 27 . MB2 was also the most frequently missed canal in maxillary molars in previous studies, with prevalences of 65% 16 , 93% 14 , and 89% in the current study. This might be explained by the fact that the MB2 canal is usually narrow, significantly smaller than the MB1 canal, with its opening often covered by secondary dentin or calcifications 28 , 29 , and the curvature in the mesial root is pronounced in the apical third of both canals and stronger in the MB2 canal. These anatomical features may make it more difficult to locate and achieve a straight course to the apex 29 . The presence of an MB2 canal should be considered the rule rather than the exception.
Table 5 Association between presence of apical periodontitis (AP) and quality of endodontic treatment in types of teeth
| Sample | Inadequate | Inadequate | Adequate | Adequate | |||
|---|---|---|---|---|---|---|---|
| Types of Teeth | Teeth with ET | n (%) | With AP n (%) | Without AP n (%) | n (%) | With AP n (%) | Without AP n (%) |
| Maxillary | |||||||
| Central | 48 | 9 (18.75) | 9 (100) | -.- | 39 (81.25) | 14 (35.89) | 25 (64.10) |
| Lateral | 49 | 17 (34.6) | 13 (76.47) | 4 (23.52) | 32 (65.30) | 14 (43.75) | 18 (56.25) |
| Canine | 31 | 7 (22.58) | 3 (42.85) | 4 (57.14) | 24 (77.41) | 10 (41.66) | 14 (58.33) |
| Premolar | 101 | 57 (56.4) | 43(75.43) | 14 (24.56) | 44 (43.6) | 19 (43.18) | 25 (56.81) |
| 1st Molars | 71 | 62 (87.3) | 58 (93.5) | 4 (6.45) | 9 (12.6) | 4 (44.4) | 5 (55.5) |
| 2nd Molars | 34 | 26 (76.4) | 24 (92.3) | 2 (7.69) | 8 (23.5) | 3 (37.5) | 5 (62.5) |
| Mandibular | -.- | ||||||
| Central | 5 | -.- | -.- | 5 (100) | 2(40) | 3 (60) | |
| Lateral | 5 | -.- | -.- | 5 (100) | 3 (60) | 2 (40) | |
| Canine | 4 | -.- | -.- | 4 (100) | -.- | 4 (100) | |
| Premolar | 32 | 17 (53.1) | 10 (58.82) | 7 (41.17) | 15 (46.9) | 1 (6.66) | 14 (93.33) |
| 1st Molar | 53 | 40 (75.4) | 32 (80) | 8 (20) | 13 (24.52) | 7 (53.84) | 6 (46.15) |
| 2nd Molar | 29 | 20 (68.9) | 17 (85) | 3 (15) | 9 (31.03) | 3 (33.33) | 6 (66.66) |
| Total | 462 | 255 (55) | 209 (81.96) | 46 (18.03) | 207 (45) | 80 (38.64) | 127 (61.35) |
In the current study, mandibular molars had the second-highest frequency of missed canals, with 18%, similar to previous studies, which found 19.7% 15 , 26% 14 , and 10.42% 16 . All mandibular molars with missed canals were associated with AP in the present study. Other studies have reported similar frequencies, such as 94.1% 16 and 95.5% 14 . Another study found 62% of missed canals in the mandibular first molars, with the distolingual canal being the most frequently missed canal, although it did not specify the percentage of AP in mandibular first molars with missed canals 15 .
In the current study, the most frequently missed canals were the distobuccal canal in mandibular first molars (42.85%), followed by the mesolingual canal in mandibular second molars (21.05%). This was similar to another study that found in mandibular first molars missed distolingual canals (21%) and mesolingual canals (29%), and in mandibular second molars, missed mesolingual canals (62%) 14 . These frequencies of missed canals in mandibular molars may occur due to variations in anatomy and location, which make it difficult to access and treat all root canals 14-16 .
In the present study, the probability of a tooth with a missed canal having AP was 16.9 (crude OR) and 10.5 (OR adjusted to the tooth type variable). These findings could be considered higher than those of previous studies, which reported probabilities of 4.38 15 , 6.25 14 , and 4.4 16 . These differences may be related to the higher percentage of teeth with IET in this study.
Good quality endodontic treatment seems to decrease the prevalence of apical periodontitis in teeth with missed canals compared to teeth with IET and missed canals. However, further studies are needed to confirm this hypothesis.
Table 6 Association between presence of quality of endodontic treatment and apical periodontitis (AP) in the root and canals of maxillary and mandibular molars
| Inadequate | Adequate | ||||||
|---|---|---|---|---|---|---|---|
| Root canals | Sample | Inadequate | AP | Adequate | AP | ||
| Yes | No | Yes | No | ||||
| N | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Maxillary molars | |||||||
| 1st molar | |||||||
| Mesiobuccal root | |||||||
| Mesiobuccal canal | 71 | 42 (59.1) | 36 (85.71) | 6 (14.28) | 29 (40.8) | 18 (62.06) | 11 (37.93) |
| Mesiobuccal 2 canal | 50 | 47 (94) | 43 (91.48) | 4(8.52) | 3 (6) | 1(33.33) | 2 (66.66) |
| Distobuccal root | |||||||
| Distobuccal canal | 71 | 34 (47.88) | 21 () | 13 () | 37 (52.1) | 11 (29.72) | 26 (70.27) |
| Palatal root | |||||||
| Palatal canal | 71 | 30 (42.25) | 19 (63.33) | 11(36.66) | 41 (57.74) | 13 (31.70) | 28 (68.29) |
| 2nd molar | |||||||
| Mesiobuccal root | |||||||
| Mesiobuccal canal | 28 | 18 (64.28) | 14 (77.7) | 4 (22.2) | 10 (35.71) | 7 (70) | 3 (3) |
| Mesiobuccal 2 canal | 11 | 11 (100) | 10 (90.9) | 1 (9.1) | -.- | -.- | -.- |
| Distobuccal root | |||||||
| Distobuccal canal | 28 | 15 (53.57) | 10 (66.66) | 5 (33.33) | 13 (46.42) | 5 (38.46) | 8 (61.53) |
| Palatal root | |||||||
| Palatal canal | 28 | 13 (46.42) | 9 (69.23) | 4 (30.76) | 15 (53.58) | 6 (40) | 9(60) |
| Mandibular molars | |||||||
| 1st molar | |||||||
| Mesial root | |||||||
| Mesiobuccal canal | 51 | 21 (41.17) | 15 (71.42) | 6 (28.57) | 30 (58.83) | 15 (50) | 15 (50) |
| Mesiolingual canal | 51 | 26 (50.98) | 17 (65.38) | 9 (34.61) | 25 (49.01) | 14 (56) | 11 (44) |
| Distal root | |||||||
| Distobuccal canal | 14 | 10 (71.42) | 9(90) | 1 (10) | 4 (28.57) | 2 (50) | 2 (50) |
| Distolingual canal | 14 | 10 (71.42) | 9 (90) | 1(10) | 4 (28.57) | 2(50) | 2(50) |
| 2nd molar | |||||||
| Mesial root | |||||||
| Mesiobuccal canal | 19 | 10 (52.63) | 7 (70) | 3 (30) | 9(47.36) | 5 (55.55) | 4 (44.44) |
| Mesiolingual canal | 19 | 12 (63.15) | 10 (83.33) | 2 (16.66) | 7 (36.84) | 2 (28.51) | 5 (71.42) |
| Distal root | |||||||
| Distobuccal canal | 2 | 2 (100) | 2 (100) | -.- | -.- | -.- | -.- |
| Distolingual canal | 2 | 2 (100) | 2(100) | -.- | -.- | -.- | -.- |
Bivariate analysis of the results obtained in the current study was very similar to that reported in the studies mentioned above. Additionally, a wide confidence interval was observed for crude OR and OR adjusted for the tooth type variable. According to tooth type, an OR of 2.5 was observed for maxillary molars, similar to the 3.1 previously reported 16 .
The major advantage of cross-sectional studies is that, with a large sample size, potential interpretation errors can be diluted 14 . However, the nature of cross-sectional studies may also be a limitation owing to the reliability of the observations. Moreover, it is difficult to establish the natural history of the disease, e.g., it is impossible to determine whether
AP is expanding, healing or stable 1 . Many of the images classified as AP at the time of analysis could be AP in the process of healing, reducing in size 30 . Another limitation was the CBCT method, which may show artifacts caused by high-density objects such as gutta-percha, which might generate false positives 14-16 .
The diagnosis, histological and microbiological analysis of the small variations seen as areas of low density (0.5 mm radiolucent zone) around the apex in ET teeth when viewed in CBCT images is another crucial factor to consider. However, treatment need not be started immediately based on this finding because when the tooth in question is asymptomatic and functions normally, the clinician should evaluate subtle changes histologically or wait for a reasonable amount of time 31 . Future studies should also consider factors including lesion size and patient age.
CONCLUSION
The frequency of missed canals was 19%, with apical periodontitis being observed in 95,3% ofthese cases. More than half of the teeth with missed canals were maxillary molars, and the MB2 was the most frequently missed canal, with apical periodontitis being observed in 90.74%. Based on these results we conclude that there was a high frequency of teeth with missed canals and PA and more than half of the teeth with missed canals were maxillary molars, with MB2 being the most common canal, commonly presenting apical periodontitis.