Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista argentina de cirugía
versão On-line ISSN 2250-639X
Rev. argent. cir. vol.112 no.4 Cap. Fed. dez. 2020
http://dx.doi.org/10.25132/raac.v112.n4.1489.ei
Articles
Extraocular sebaceous carcinoma
1 Servicio de Cirugía del Hospital Central de las Fuerzas Armadas Montevideo, Uruguay
Sebaceous carcinoma is a rare and aggressive neoplasm derived from the adnexal epithelium of the sebaceous glands with a tendency toward local recurrence and distant metastasis1-4. Although its etiology is unknown, several studies suggest that it derives from pluripotent stem cells differentiating into sebaceous lineage cells1-3. In 75% of cases sebaceous carcinomas develop in the head and neck, particularly in the periocular region, predominantly on the upper eyelid, although they can appear in any area with sebaceous glands.
We report the case of a female patient with extraocular sebaceous carcinoma of the perianal region.
A 72-year-old female patient sought medical care due to a perianal tumor lasting several months. She had a history of hypertension, type 2 diabetes mellitus, hysterectomy with bilateral oophorectomy for a benign condition and severe aortic stenosis with indication of aortic valve replacement and no history or symptoms of gastrointestinal disease.
The perianal tumor was painless but had increased in size over the past months.
The physical examination revealed a firm, irregular, non-ulcerated tumor located at the left perianal region at the 3 o’clock position with a major diameter of 3 cm (Fig. 1).

Figure 1 The tumor is visualized in the perianal margin at the 3 o’clock posi tion with resection edges marked before resection, preserving surgi cal margins.
The patient underwent excisional biopsy.
The pathology report (Fig. 2) described a nodular lesion with cords of cells with vesicular and clear nuclei, finely granular chromatin and relatively abundant cytoplasm, mitotic count of 21 mitosis per 10 high power fields, tumor emboli in lymphatic and blood vessels and infiltration of adipose tissue and skeletal muscles. In summary, the histology corresponds to a poorly differentiated tumor.
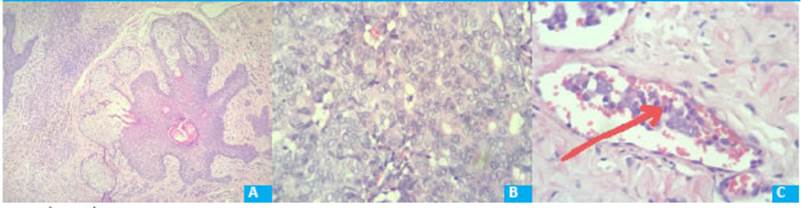
Figure 2 Anatomía patológica. A: Normal sebaceous gland. Hematoxylin and eosin stain x4 B: Tumor with some neoplastic cells with clear cytoplasm like sebocytes..Hematoxylin and eosin stain x4. C: Blood vessel emboli of neoplastic cells. Hematoxylin and eosin stain x4
The immunohistochemical tests concluded that the sample corresponded to a malignant adnexal neoplasm suggestive of a primary sebaceous carcinoma of the perianal region.
A computed tomography scan requested to evaluate regional and distant spread showed enlargement of two left inguinal lymph nodes. These findings, in addition to infiltration of the adipose tissue and external sphincter and presence of tumor emboli in lymphatic and blood vessels, indicated a locally aggressive neoplasm. The patient underwent further excision to widen the margins and inguinal lymph node clearance. The pathology report confirmed that the margins were clear and presence of lymph node metastasis of sebaceous carcinoma.
One month after surgery, the oncology team indicated external radiation therapy in the perianal and inguinal regions. After one year, the patient remains without symptoms and with normal imaging tests. Chemotherapy was not indicated.
Sebaceous carcinoma represents between 0.2 and 4.6% of all skin cancers. One or two new cases per million population are reported per year1. The tumor typically arises in elder patients (60-80 years)1-4. The literature is inconsistent about which sex is predominant1-4. Sebaceous carcinoma may be sporadic or associated with genetic syndromes such as Muir Torre syndrome (colon, breast, urinary and skin cancer) with mutations in genes MSH2, MLH1 and MSH61-3; therefore, these patients should be carefully evaluated in terms of personal and family oncological history, complementary tests and close monitoring for other neoplasms.
Extraocular sites for these tumors include the parotid region, nose, scalp, neck, external auditory canal, retroauricular region, submandibular region, trunk, hips, arms and toes1,2,4.
Sebaceous carcinoma presents as a painless, rapidly growing, and hard subcutaneous erythematous or yellowish nodular lesion. Clinically and histologically these tumors can mimic inflammatory diseases or other tumors, often delaying the diagnosis1-3. Most of the lesions develop de novo, but in some cases sebaceous carcinoma develops from a preexisting sebaceous cyst.
Extraocular tumor stage is based on the TNM staging system of non-melanoma skin cancers1.
Multicentricity, poor differentiation, aggressive local invasion and lymphatic and blood vessel involvement are predictors of adverse outcome. Local involvement is one of the strongest determinants of prognosis1 and is characterized by its aggressiveness with high rate of regional lymph node and distant metastases in the liver, lung, brain and bones. Yet, some authors suggest that lymphatic involvement has no significant influence on 5-year survival1,2. The histology of sebaceous carcinoma is characterized by dermal lobes of sebocytes in different grades of maturity, tubular structures of ductal differentiation and hyperchromatic nuclei with high mitotic activity. Tumors may be moderately or poorly differentiated. Immunohistochemical testing is important and necessary when the histologic findings are not conclusive2,3.
Surgical resection is the treatment of choice with margins of 5 to 6 mm; in case of lymph node involvement, lymph node clearance is indicated. The level of evidence to recommend the best treatment is weak due to the low incidence of these tumors1,2,4.
Local recurrence after surgery varies between 9 and 36% at 5 years with margins of 4 mm1. The evidence for curative or palliative chemotherapy is scarce and its use becomes relevant in cases with metastases. Radiation therapy alone has a mortality rate of 78% at 4 years, compared with 33% for simple tumor resection and 7% for extended local resection1.
Although there are no follow-up protocols, clinical examination and imaging tests have been suggested for early detection of local or lymphatic recurrences to perform rescue surgery.
Survival rates at 5 and 10 years range from 78 to 92% and 6 to 86%, respectively1.
In our population of approximately three million people, three new cases of sebaceous carcinoma are estimated every year, of which 25% (0.75 patients per year) would correspond to extraocular location as in our patient. We have not found any publication of sebaceous carcinoma in the perianal region.
Referencias bibliográficas /References
1. Eyssautier S F y cols. Carcinoma sebáceo extraocular, reporte de un caso. Rev Otorrinolaringol Cir Cabeza Cuello 2019; 79:98- 104. [ Links ]
2. Moliné et al. Carcinoma Sebáceo. Dermatol Argent 2013; 19 (2): 112-116 [ Links ]
3. Cieza-Díaz DE y cols. Carcinoma sebáceo extraocular: presentación de 2 casos. Actas Dermosifiliogr 2012; 103(10):919-22. http://dx.doi.org/10.1016/j.ad.20111.05.022 [ Links ]
4. González-Almaraz G y cols. Carcinoma Sebáceo. Rev Cent Dermatol Pascua 1999; 8 (2). [ Links ]
Received: March 24, 2020; Accepted: August 04, 2020











 texto em
texto em 


