Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista argentina de cirugía
versão On-line ISSN 2250-639X
Rev. argent. cir. vol.113 no.1 Cap. Fed. abr. 2021
http://dx.doi.org/10.25132/raac.v113.n1.1569.ei
Articles
How to train a complex skill in surgery: Qualitative evaluation of a simulation-based strategy
Introduction
It has been two decades since the publication of To Err is Human, a report on the impact of medical errors on health care1. Since then, several valuable tools have been developed to promote advances in the prevention or reduction of damage. “Never events” such as wrong-patient and wrong-site surgery still occur with disturbing frequency2. The challenge for patient safety is the development and implementation of tools and strategies to allow organizations to measure and reduce harm inside and outside the hospital, on an ongoing and routine basis.
Several patient safety tools, as checklists and time-outs, have been adopted in the surgical field and are effective when used appropriately3. As a result of the greater understanding of the importance of teamwork, simulation-enhanced interprofessional education interventions have been used to improve professional performance inside and outside the operating room; some of these interventions have been associated with better results in health care4. Diagnostic errors have been a neglected topic in patient safety until recently; similarly, the surgical decision-making process has also been neglected, particularly when whether to operate or not. A perfectly performed but inappropriate operation is still an example of avoidable damage.
There is evidence that technical skills in surgery are closely associated with better outcomes for patients5; however, we cannot forget that about 80% of serious errors in this specialty are due to failures in non-technical skills inherent to the science of human factors6, as leadership, communication, mutual support, resource management, help management, teamwork, situational awareness, anticipation and planning7.
Therefore, non-technical skills must be trained in the operating room or in simulating scenarios to make the difference8. Simulation-based training has an impact on skills and attitudes, especially when training concludes with debriefing, which is “crucial to the learning process”.
The development of non-technical skills may benefit from debriefing and from the reflective processes involved9. Non-technical skills are the cognitive, social and personal resource skills that, within health care, are recognized as being crucial to the provision of high-quality, safe and effective patient care. Certain experiences can result in transformative learning by prompting reflection of one’s prior assumptions and a significant shift in one’s outlook and understanding of the world; this is referred to as the process of perspective transformation10. These include a shift from “fact memorization” to the development of decision-making skills, another non-technical skill, and a shift to the achieving of effective teamwork within health systems to improve care.
Quality care of any patient requires more than procedural expertise. It requires learning tasks that integrate knowledge, skills, and attitudes. In other words, the coordination of qualitatively different “constitutive skills” necessary for complex learning, to mitigate the drawbacks of compartmentalization11 and partly based on the theoretical frameworks of experiential and reflective learning.
The aim of this study is to report the results of a short simulation-based educational program for training in complex surgical skills. We focused on technical and non-technical skills involved in a complex task, such as the adequate care of patients with complex acute gallbladder disease. A summarized description of the activities carried out and the results of the learning process are presented considering the participants’ perceptions.
Material and methods
We present a case study, analyzing a short training program on the appropriate management of patients with acute gallbladder disease developed at INSPIRE Simulación Femeba, Argentina, in October 2019. This program was developed using a simulation program12 to manage the content, level of complexity and fidelity of the training activities and the type of support provided to the participants by the instructors. This approach combines single-loop with double-loop learning processes. Single-loop learning involves doing things right and improving efficiency while double-loop learning involves questioning the assumptions about what is done.
The course lasted 20 hours divided into 6 hours of asynchronous on-line training and 14 hours of on-site classes distributed in two days. TTen health care professionals (5 women and 5 men) from different disciplines and education levels participated: 4 specialists with 2 to 20 years of experience, 4 residents with 3 to 4 years of experience, and 2 were crub nurses with more than 20 years of experience.
The on-line phase was implemented under the flipped classroom approach using an open source platform (Moodle®) used by the Femeba Institute for distance learning. Only surgeons participated in this phase and had to solve a real case of a patient with a complex acute disease. A directory of scientific articles was available to participants to provide rationale for decision making in a discussion forum with peers.
On the first day of the on-site phase, an expert provided feedback on the discussion held on the on-line platform, followed by a step devoted to drawing conclusions. This was followed by a Supervised Skills Workshop, consisting of 6 task simulation stations and 2 stations with virtual reality simulator, as detailed below:
▪▪One station with the virtual reality simulator Vimedix Cardiac/Abdo® ultrasoundsimulator (CAEHealthcare, Inc).
▪▪One station for percutaneous surgery using Lubox/ CP®, a training box with a synthetic model for interventional procedures developed at Creative Lab, INSPIRE Simulación Femeba.
▪▪Four stations for laparoscopic surgery using Lubox/ CL®, a training box with a camera developed in the same laboratory with a simple synthetic model of dissection; these were later replaced by different synthetic models representative of cholecystectomy cases of increasing complexity (Fig. 1).
▪▪Two stations using the virtual reality simulators LapSim® (Surgical Science).

Figure 1 Lubox/CL: training box with a camera with a synthetic model of liver-gallbladder-extrahepatic bile ducts and hepatic pedicle for training in difficult cholecystectomy.
This workshop lasted 4 hours. The participants were divided into 4 groups of 2 physicians each. There was also a scrub nurse in two of these groups who participated in all the stations except for the virtual reality ultrasound simulator and both stations with the LapSim® simulator. All the participants were assigned a role for each station: surgeon, camera/assistant and scrub nurse. The physicians switched roles during the passage through the different stations. Each station had specific learning goals represented by a series of assigned tasks related with the following topics:
Technical goals:
▪▪Pedicle dissection.
▪▪Cholecystecotmy and cannulation of the cystic duct.
▪▪Cholecystectomy.
▪▪Ultrasound exploration.
▪▪Percutaneous cholecystectomy.
Non-technical goals:
▪▪Communication.
▪▪Teamwork.
Performance at all stations was evaluated by peers (within the same group) using a checklist. The instructors evaluated the groups through direct feedback (feedback in action). In the case of virtual reality simulators with complete procedural exercises, team performance could have been evaluated using computer-derived metrics; however, we decided to ignore these records as this was the first contact of the participants with this type of simulators to avoid possible bias caused by the strange cognitive load13.
Afterwards, all participants took part in a focus group session with a role-switch activity14 based on a trigger video. The aim of the activity was to discover the key points of crisis resource management (CRM), as a way to begin learning the science of human factors and its impact on health outcomes, and concluded with an instructor-led debriefing using advocacy and inquiry15.
The last activity of the first day consisted of the presentation of the simulation scenario as a preliminary step to the simulated clinical experiences (SCEs) that would take place during the following day.
During the second day all the participants participated in different SCEs. By definition, a SCE consists of an initial introduction or briefing stage, followed by immersion in a scenario -in this case, of high complexity and fidelity -and ends with reflective learning or debriefing16.
Four SCEs were carried out with high physical, conceptual and emotional fidelity. Each of them represented a complex case problem of patients with acute gallbladder disease. The physicians underwent at least 2 SCEs to go through the experience, reflect on it, analyze possibilities for improvement and learn from them, apply what they had learned and reflect on it again17. The scrub nurses participated in the four SCEs. These experiences took place in the operation room and covered different learning goals, which are summarized below:
▪▪Clinical reasoning.
▪▪Decision-making.
▪▪Situational awareness.
▪▪Role clarity, including leadership and teamwork.
▪▪Communication.
In each scenario, the participants played the same role as in their professional life: resident, specialist, and scrub nurse. The role of the anesthesiologist was played by an instructor as confederate. Different hybrid simulation models were used in combination:
▪▪Lucina® high-fidelity manikin simulator (CAE Health care, Inc) with synthetic models (Fig. 2).
▪▪Virtual reality simulator with torso cardiopulmonary resuscitation training manikin.

Figure 2 Escenario de alta fidelidad: equipo quirúrgico inmerso en escenario de alta fidelidad donde se observa simulador híbrido: Lubox/CL + si mulador maniquí de alta complejidad Lucina (CAE Healthcare, Inc).
Before immersion in the simulation scenarios, a confidentiality agreement was established and signed to protect the image, except for the case of academic purposes, and identity of the participants in the scenarios and during the group analysis. Failure to comply with a prompt or clue and time (duration) would be the criteria for terminating the scenarios. None of the scenarios lasted more than 10 minutes and all of them were followed by a focus group session using a PEARLS debriefing tool18. This type of debriefing included feedback for issues inherent to the management of protocols, and the advocacy-inquiry method for the non-technical aspects of performance.
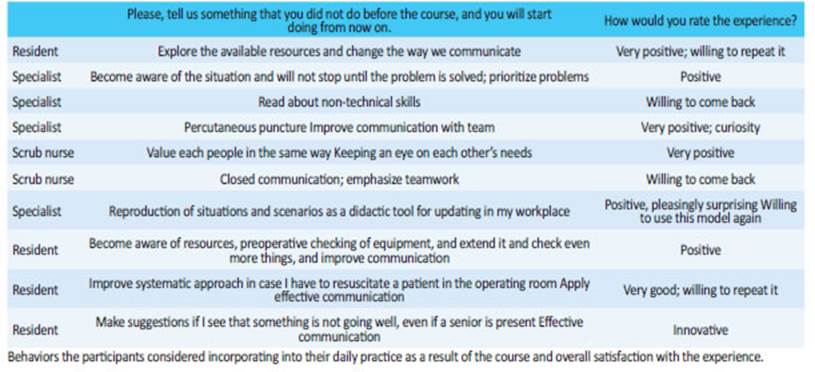
Finally, a questionnaire was administered to explore participants’ perceptions of the educational impact of the experience and of the changes in their attitudes towards their own professional practice.
Results
The results of the participants’ performance are not included because they are beyond the scope of this article.
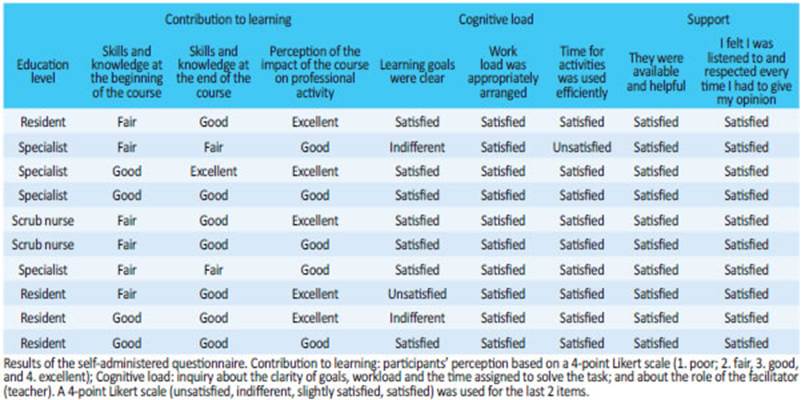
The questionnaire explored the following items:
a) Perception of the contribution of learning.
b) Cognitive load of tasks.
c) Instructors’ support.
d) Changes of attitude towards the future.
A 4-point Likert scale (poor, fair, good, and excellent) was used to score the responses, except for the questions on attitude changes, which were open-ended (Tables 1 and 2). Fifty percent of the participants perceived their skills and knowledge improved at the end of the course compared to their perception at the beginning of the course, while 80% perceived the impact of the course on their professional activity was good or excellent.
With respect to the cognitive load of the tasks, 70% responded with the highest scores that the objectives were clear, and 30% gave low or very low scores. The distribution of the workload and the time load obtained the highest level of satisfaction in 100% and 90% of the participants, respectively.
The level of support provided by the instructors received the highest rating in all cases.
Regarding changes of attitude towards the future - “ which behaviors that were not usually developed are you considering incorporating?” - 100% of the participants mentioned the need to improve human factors (communication, teamwork, situational awareness); only one also emphasized the need for improving a technical skill. The experience was rated as positive or very positive by all participants, who were eager to repeat it.
Discussion
This strategy was widely accepted among the participants. Diversity in terms of discipline, age, sex, and level of education made it possible to cover the different possible perspectives; however, the number was limited. Nevertheless, we were able to reach some conclusions that are consistent with the literature. The incorporation of non-technical skills in surgical training, residency programs, and training of health care professionals involved in surgery is a recent process, and its progress is still uneven and intermittent. As non-technical skills do not form part of formal teaching and training, they are rarely considered by professionals when evaluating their performance. In fact, one problem of the poor insight of non-technical skills is the overinflated perception of self-efficacy19.
The perspective of those who participated in this training program based on advanced clinical simulation was retrieved by means of a questionnaire and suggests that, when these skills are deliberately subjected to reflection and training, they become conscious and valued. In this way, a change of attitude towards the own practice is possible.
We believe that simulation-based training, focused on learning complex tasks, offers the possibility of improving the overall performance of the surgical team. As Cragno20 has mentioned, the participation of different actors in the activity creates a collective that we could call a team that carries out a task, in this case the management of a patient with acute gallbladder disease, which is not the result of the algebraic sum of the tasks of each member and which cannot be carried out by any of its members acting on their own. This is how the concept of collective competencies arises. As the author mentions, one of the core challenges of medical education is the design and use of teaching strategies that allow the development of these competencies which constitute properties that emerge from a complex system, since the task of the group in terms of learning is much more than the product of the sum of the participation of the different actors. Future research should focus on evaluating the impact of this training on the development of non-technical skills, their incorporation into real life, how long they last over time and the overall performance of the teams, that is, to determine the conversion of knowledge into new behaviors21. The incorporation of a validated survey for the evaluation of attitudinal changes will be another challenge.
Referencias bibliográficas /References
1. Corrigan JM, Kohn LT, Donaldson MS (editors). To err is human: building a safer health system. Washington (DC): National Acade mies Press; 1999. [ Links ]
2. Bates DW, Singh H. Two Decades Since To Err Is Human: An As sessment of Progress and Emerging Priorities in Patient Safety. Health Aff (Millwood). 2018; 37(11):1736-43. doi:10.1377/hltha ff.2018.0738. [ Links ]
3. Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009; 360(5):491-9. doi:10.1056/NEJMsa0810119. [ Links ]
4. Wong AH, Gang M, Szyld D, Mahoney H. Making an “Attitude Adjustment”: Using a Simulation-Enhanced Interprofessional Education Strategy to Improve Attitudes Toward Teamwork and Communication. Simul Healthc. 2016; 11(2):117-25. doi:10.1097/SIH.0000000000000133. [ Links ]
5. Birkmeyer JD, Finks JF, O’Reilly A, et al. Surgical skill and com plication rates after bariatric surgery. N Engl J Med. 2013; 369(15):1434-42. doi:10.1056/NEJMsa1300625. [ Links ]
6. Greenberg CC, Regenbogen SE, Studdert DM, et al. Patterns of communication breakdowns resulting in injury to surgical pa tients. J Am Coll Surg. 2007; 204(4):533-40. doi:10.1016/j.jamcoll surg.2007.01.010. [ Links ]
7. Cobián JI. Entrenamiento en cirugía mínimamente invasiva hoy. Revisita de la Sociedad de Ginecología y Obstetricia de la Provin cia de Buenos Aires. 2020; 51:249/1. [ Links ]
8. Gjeraa K, Spanager L, Konge L, Petersen RH, Østergaard D. Non-technical skills in minimally invasive surgery teams: a systematic review. Surg Endosc. 2016; 30(12):5185-99. doi:10.1007/s00464-016-4890-1. [ Links ]
9. Fanning RM, Gaba DM. The role of debriefing in simulation-based learning. Simul Healthc. 2007; 2(2):115-25. doi:10.1097/SIH.0b013e3180315539. [ Links ]
10. Kerins J, Smith SE, Phillips EC, Clarke B, Hamilton AL, Tallentire VR. Exploring transformative learning when developing medical students’ non-technical skills. Med Educ. 2020; 54(3):264-74. doi:10.1111/medu.14062. [ Links ]
11. van Merriënboer JJG y Kirschner PA. Ten Steps to Complex Lear ning: A Systematic Approach to Four-Component Instructional Design. ISBN 978-0-8085-5792-3. [ Links ]
12. Roussin CJ, Weinstock P. SimZones: An Organizational Innova tion for Simulation Programs and Centers. Acad Med. 2017; 92(8):1114-20. doi:10.1097/ACM.0000000000001746. [ Links ]
13. Leppink J, van den Heuvel A. The evolution of cognitive load theory and its application to medical education. Perspect Med Educ. 2015; 4(3):119-27. doi:10.1007/s40037-015-0192-x. [ Links ]
14. University of Tenesse (s.f.) The What, Why & How of Role Playing in the College Classroom. Knoxville. Recuperado de: https://tea ching.utk.edu/wp-content/uploads/sites/78/2018/03/RolePla ying_Handout.pdf. [ Links ]
15. Rudolph JW, Simon R, Dufresne RL, Raemer DB. There’s no such thing as “nonjudgmental” debriefing: a theory and method for debriefing with good judgment. Simul Healthc. 2006; 1(1):49-55. doi:10.1097/01266021-200600110-00006. [ Links ]
16. INACSL Standards Committee (2016, December). INACSL Stan dards of Best Practice: Simulation SM: Simulation Glossary. Clinical Simulation in Nursing. 2016; 12:S39-S47. https://doi.org/10.1016/j.ecns.2016.09.012 [ Links ]
17. Grant J, Marsden P. Training Senior House Officers by Service- Based Learning. London: Joint Centre for Education in Medicine; 1992. [ Links ]
18. Eppich W, Cheng A. Promoting Excellence and Reflective Learning in Simulation (PEARLS): development and rationale for a blended approach to health care simulation debriefing. Simul Healthc. 2015; 10(2):106-15. doi:10.1097/SIH.0000000000000072. [ Links ]
19. Pena G, Altree M, Field J, et al. Surgeons’ and trainees’ perceived self-efficacy in operating theatre non-technical skills. Br J Surg. 2015; 102(6):708-15. doi:10.1002/bjs.9787. [ Links ]
20. Cragno AG. Trabajo en equipo y educación. Breve reflexión desde la complejidad. Rev Arg Med. 2020; 8(2):151-3. [ Links ]
21. Nolla-Domenjo M. La evaluación en educación médica: Principios básicos. EducMéd. [online]. 2009; 12(4) [citado 2020-08-17]: 223- 9. Disponible en: <Disponible en: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1575-18132009000500004&lng=es&nrm=iso >. ISSN 1575-1813. [ Links ]
Received: August 19, 2020; Accepted: October 16, 2020











 texto em
texto em