Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista argentina de cirugía
versão On-line ISSN 2250-639X
Rev. argent. cir. vol.113 no.1 Cap. Fed. abr. 2021
http://dx.doi.org/10.25132/raac.v113.n1.1485.ei
Articles
ALPPS using liver-first reverse approach as a surgical option to treat synchronous colorectal liver metastases
1 Servicio de Cirugía Hepatobiliar y Trasplante Hepático. Hospital El Cruce. Buenos Aires, Argentina.
2 Servicio de Oncología. Hospital El Cruce. Buenos Aires, Argentina.
Introduction
The risk for postoperative liver failure is the most important limitation for the treatment of patients with primary or secondary liver cancer. The liver-first approach for patients with colorectal cancer with synchronous liver metastases is a valid therapeutic option which allows the multidisciplinary team to start chemotherapy as an initial step, and thus observe which patients have a favorable response to the adjuvant treatment, avoiding major surgery in those who would not benefit from it.
Among the different strategies used to increase resectability in liver tumors, a technique known as ALPPS (associating liver partition with portal vein ligation for staged hepatectomy), originally performed by Hans Schlitt in 2007, was developed for patients with tumors previously considered unresectable1.
We report the case of a male patient referred to our center with a diagnosis of synchronous multiple liver metastases of colorectal cancer considered unresectable who underwent ALPPS using the liver-first reverse approach.
A 74-year-old male patient with a performance status of 0 and a history of asymptomatic polycystic kidney disease was referred to our center with synchronous liver metastases of colorectal cancer considered unresectable.
During the initial evaluation, the tumor was identified 4 cm above the anal margin without signs of sub-occlusion. Tumor markers: CA 19-9: 68.6 (< 37 IU/mL) and CEA 48.16 (< 5 ng/mL). The video-assisted colonoscopy showed the presence of a vegetative, infiltrating, and ulcerated rounded lesion which produced luminal deformation and narrowing, 6 cm in length and 3 cm above the anal margin. Pathology report: cross-shaped infiltrating tubulopapillary adenocarcinoma (Viena category 5) KRAS PG12D mutation.
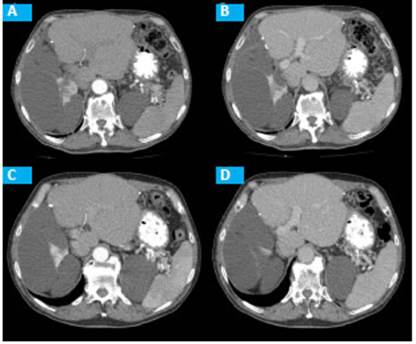
The computed tomography (CT) scan showed multiple and bilateral metastases in segments III, IV, VI, VII y VIII (Fig. 1). After discussing the case in an interdisciplinary meeting, neoadjuvant therapy with capecitabine and oxaliplatine was decided. After three cycles of chemotherapy, surgical treatment with a liver-first approach was planned due to partial hepatic response.
The ALPPS procedure was considered a feasible means to perform extended liver resection with insufficient future liver remnant, combined with decreased risk of tumor progression in the interim. The first step of the procedure was performed through a conventional approach via a right subcostal incision with extension to the subxiphoid region. The right and left liver lobes were completely mobilized by dissecting the hepatic ligaments, and the lesions in segments III and IV were resected under ultrasound guidance using parenchymal-sparing technique. The gallbladder was resected, the liver pedicle was dissected, and the right portal vein was ligated. The line of demarcation was identified until reaching the Cantlie’s line. Parenchymal hepatic transection was performed along the Cantlie’s line using ultrasonic surgical aspirator until the vena cava was visualized (Fig. 2). There were no complications. The future liver remnant was evaluated on postoperative day 7 by CT volumetry. The residual liver volume (RLV) was 396 cm3 and the preoperative volume was 238 cm3, corresponding to an increase of the RLV from 21% to 35% of the total liver volume (TLV). The second step of the ALPPS procedure was then carried out. The right pedicle was individualized and transected using a 45-mm mechanical vascular stapler, and a 60-mm stapler was used to close the right suprahepatic vein and right liver resection was completed. The patient evolved with favorable outcome and was discharged on postoperative day five.
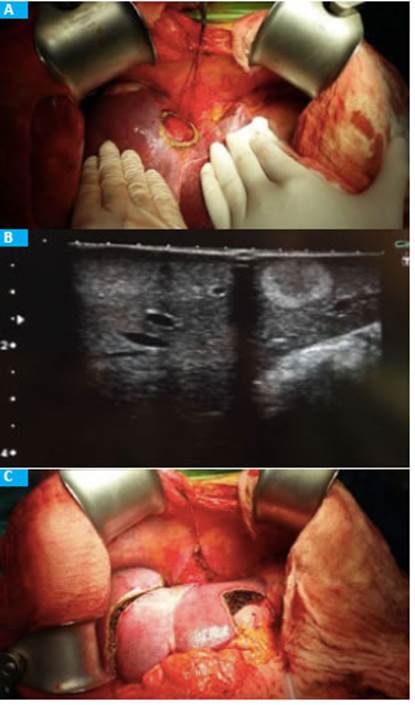
Figure 2 First stage of ALPPS. A. Liver resection segment IV. B. Intraoperative ultrasound showing mestastasis. C. Surgical bed of segments III, IV and liver transection.
During follow-up, CT scan and magnetic resonance imaging (MRI) showed a lower rectal tumor, absence of mesorectal lymph nodes and infiltration of the anal margin and sphincter. Radiation therapy was started on postoperative day 40 (4500 cGy to whole pelvis +/ 540 cGy boost) and concurrent chemotherapy of capacitabine for the rectal lesion, followed by Miles procedure through laparoscopic. The patient stayed 24 hours in the intensive care unit (ICU) and was discharged on postoperative day 4. He did not develop complications during long-term follow-up and started monotherapy with capacitabine on postoperative day 45.
Pathology report: Liver: surgical specimens of liver segments III, IVA, IVB and right liver resection with metastases of mucinous colloid colorectal adenocarcinoma. Clear surgical margins. Rectum: ulcero-infltrative, moderately differentiated rectal adenocarcinoma, 1.8 × 1.5 × 1.5 cm in diameter with irregular appearance, without evident perforations; proximal and distal margins of resections free of malignancy, and of angiolymphatic and perineural invasion. Tumor invasion of the serous layer and microscopic invasion of the perirectal fat. One pericolic lymph node (1/5) with metastasis. Tumor stage PT3 PN1 PM1.
Three years after surgery, the patient continues with oncologic follow-up and receives chemotherapy due to multiple pulmonary metastases (Fig. 3).
Discussion
Surgical resection is the only potentially curative treatment for patients with synchronous colorectal liver metastases2. The underlying rationale for the use of preoperative chemotherapy in these patients is to provide early treatment of metastatic disease, reduce the rate of recurrence after surgery, evaluate tumor biology, improve patient selection for an aggressive surgical procedure, avoid unnecessary surgery in those with rapidly advancing disease, test tumor chemosensitivity, and adapt postoperative treatment3.
Adam et al.4 reported the results in 58 patients (44%) who underwent hepatectomy after an objective tumor response (group 1), 39 (30%) after tumor stabilization (group 2), and 34 (26%) after tumor progression (group 3). The global recurrence was 78% and was lower in group 1 (68%) versus groups 2 and 3 (89% and 83%, respectively, P = 0.05), associating poor outcomes after resection in case of tumor progression after neoadjuvant therapy.
In the classic approach, borderline liver metastases are resected later after the primary tumor has been approached first or simultaneously with the primary tumor; the time of tumor progression is minimized, but morbidity is high (not appropriate for patients who require major liver resection, elder patients and with locally advanced rectal cancer)5. The reverse strategy, also known as “liver-first”, is a downstaging approach and consists of systemic chemotherapy, followed by resection of colorectal liver metastases before the primary colorectal tumor is resected. Patients with minimal symptoms or asymptomatic colorectal cancer with locally advanced hepatic metastases may be submitted to the liver-first strategy with the aim of treating the systemic disease which affects the prognosis, avoiding unnecessary delays of the adjuvant therapy, and may downstage previously liver metastases believed unresectable6.
Brouquet et al.3 published the first study evaluating three different surgical strategies used to treat patients with sychronous colorectal liver metastases. They retrospectively analyzed the outcomes of 156 patients with synchronous colorectal liver metastases using three different approaches: classic (n = 72), combined (n = 43) and reverse (n = 27). Patients with complete reverse approach had more and larger liver metastases and this difference was significant. Mortality rates and cumulative postoperative mortality for the combined, classic and reverse approaches were 5%, 3% and 0%, respectively, and 47%, 51% and 31%, respectively.
ALPPS is a novel variant of two-stage hepatectomy that combines portal vein ligation and parenchymal transection in the first stage7. We present a male patient with synchronous colorectal liver metastases with partial response to chemotherapy who underwent the ALPPS technique using the reverse approach. The technique proved to be safe and feasible in selected patients when performed by hepato-pancreato-biliary surgeons.
Referencias bibliográficas /References
1. Schlitt HJ, Hackl C, Lang SA. ‘In-situ split’ liver resection/ALPPS - Historical development and current practice. Visc Med 2017; 33(6):408-412. PMID: 29344513. DOI: 10.1159/000479850 [ Links ]
2. Jegatheeswaran S, Mason JM, Hancock HC, Siriwardena AK. The Liver-First Approach to the Management of Colorectal Cancer With Synchronous Hepatic Metastases. JAMA Surg [Internet]. 2013 Apr 1 [cited 2018 May 8]; 148(4):385. Available from: Available from: http://www.ncbi.nlm.nih.gov/pubmed/23715907 PMID: 23715907 [ Links ]
3. Brouquet A, Mortenson MM, Vauthey J-N, Rodríguez-Bigas MA, Overman MJ, Chang GJ, et al. Surgical strategies for synchronous colorectal liver metastases in 156 consecutive patients: classic, combined or reverse strategy? J Am Coll Surg [Internet]. 2010 Jun [cited 2018 May 8]; 210(6):934-41. Available from: Available from: http://linkinghub.elsevier.com/retrieve/pii/S1072751510001249 PMID: 20510802 [ Links ]
4. Adam R, Pascal G, Castaing D, Azoulay D, Delvart V, Paule B, et al. Tumor progression while on chemotherapy: a contraindica tion to liver resection for multiple colorectal metastases? Ann Surg [Internet]. 2004 Dec [cited 2018 May 8]; 240(6):1052-61; discussion 1061-4. Available from: Available from: http://www.ncbi.nlm.nih.gov/pubmed/15570210 PMID: 15570210 [ Links ]
5. de Rosa A, Gómez D, Hossaini S, Duke K, Fenwick SW, Brooks A, et al. Stage IV colorectal cancer: Outcomes following the liver-first approach. J Surg Oncol [Internet]. 2013 Dec [cited 2018 May 8]; 108(7):444-449. Available from: Available from: http://www.ncbi.nlm.nih.gov/pubmed/24009161 PMID: 24009161 [ Links ]
6. Waisberg J. Liver-first approach of colorectal cancer with syn chronous hepatic metastases: A reverse strategy. World J Hepatol [Internet]. 2015 [cited 2018 May 8]; 7(11):1444. Available from: Available from: http://www.wjgnet.com/1948-5182/full/v7/i11/1444.htm [ Links ]
7. de Santibañes E, Clavien P-A. Playing Play-Doh to prevent postop erative liver failure: the »,» ®,® §,§ ­, ¹,¹ ²,² ³,³ ß,ß Þ,Þ þ,þ ×,× Ú,Ú ú,ú Û,Û û,û Ù,Ù ù,ù ¨,¨ Ü,Ü ü,ü Ý,Ý ý,ý ¥,¥ ÿ,ÿ ¶,¶ ALPPS »,» ®,® §,§ ­, ¹,¹ ²,² ³,³ ß,ß Þ,Þ þ,þ ×,× Ú,Ú ú,ú Û,Û û,û Ù,Ù ù,ù ¨,¨ Ü,Ü ü,ü Ý,Ý ý,ý ¥,¥ ÿ,ÿ ¶,¶ approach. Ann Surg [Internet]. 2012 Mar [cited 2018 May 8]; 255(3):415-7. Avail able from: Avail able from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00000658-201203000-00002 PMID: 22330039 [ Links ]
Received: June 23, 2020; Accepted: October 14, 2020











 texto em
texto em