Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista argentina de cirugía
versão impressa ISSN 2250-639Xversão On-line ISSN 2250-639X
Rev. argent. cir. vol.113 no.2 Cap. Fed. jun. 2021
http://dx.doi.org/10.25132/raac.v113.n2.1517.ei
Articles
Schwannoma of the cervical vagus nerve
1 Servicio de Cirugía de Cabeza y Cuello, Sanatorio Dr. Julio Méndez de Buenos Aires, Argentina.
The parapharyngeal space is a complex anatomic area, with deep location and bounded medially by the upper part of the pharynx, posteriorly by the prevertebral fascia and laterally by the parotid region. The parapharyngeal space takes the shape of an inverted pyramid. The base of the pyramid is at the skull base, and the inferior apex terminates at the greater cornu of the hyoid bone. The classical description distinguishes a midline compartment known as retropharyngeal space, and a lateral pharyngeal space at both sides and divided by the Riolan’s bouquet into the pre-styloid and post-styloid spaces.
Tumors of the parapharyngeal space account for approximately 0.5% of total head and neck neoplasms. Approximately 90% are primary neoplasms and most of them are benign tumors; yet 20% present malignant transformation. Nevertheless, the histological origin of these tumors is heterogeneous: 45% correspond to salivary gland tumors, 30% to neurogenic tumors and 15% are lymphomas or lymph node metastases1.
The term ‘schwannoma’, first introduced by Stout in 1935, identifies a benign tumor with sporadic malignant degeneration arising from cranial, peripheral and autonomic nerve sheath cells.
Schwannomas of the parapharyngeal space represent 0.09% of all head and neck tumors; 18% correspond to tumors of the parapharyngeal space and 60% to neurogenic tumors of this region. The most common nerves affected are the vagus nerve and those of the cervical sympathetic chain. Schwannomas present as slow-growing elastic masses with round or multilobed shape. They rarely cause functional deficit of the nerve affected, except in the sympathetic chain. Hoarseness is the most common specific symptom due to vocal cord paralysis, while a paroxysmal cough produced on palpation of the mass
is the pathognomonic sign. A review of the literature demonstrated that 4% of schwannomas of the cervical vagus nerve are malignant, mainly associated to neurofibromatosis type 13.
We report a rare case of schwannoma of the cervical vagus nerve of the right parapharyngeal space in a 42-year-old male patient.
A 42-year-old male patient was referred to the outpatient clinic of head and neck surgery due to a lateral neck mass with no further symptoms. He had no relevant medical history. On physical examination, a 4 x 4 cm right lateral neck mass, hard-elastic in consistency, was palpated in the mid part of the neck and extended upwards and downwards. Lymph nodes were not enlarged. A computed tomography (CT) scan and a carotid angiography were performed (Fig. 1).
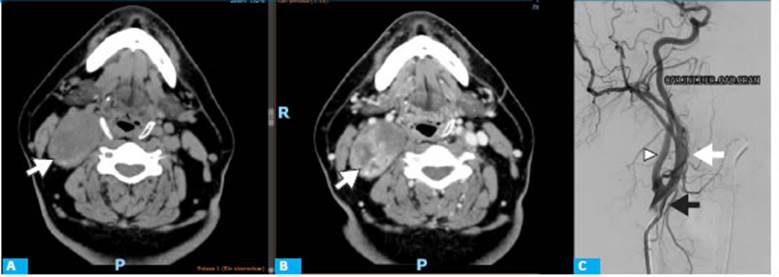
Figure 1 A. Contrast-enhanced CT scan of the neck and carotid angiography. A: Axial section without contrast agent. A rounded lesion, 55 × 39 × 64 mm in size with well-defined borders is observed at the level of the right jugular vein and carotid artery within the sternocleidomastoid muscle, displacing the adjacent structures without affecting them (arrow). B: Axial section with contrast agent. The mass has hyperdense areas in the phase without contrast with heterogenous enhancement post-contrast (arrow). C: The right common carotid artery does not show any abnormality (black arrow). The internal carotid artery is displaced inward and forward (white arrow). External carotid artery with mild dye. (arrowhead)
The patient was scheduled for surgery using a combined trans-cervical and a trans-parotid approach. During surgery, the mass was observed in close contact with the internal carotid artery but did not involve it. The sternocleidomastoid muscle was skeletonized and lateralized, and the tumor was identified in the vagus nerve (Fig. 2). An attempt was made to perform intracapsular dissection but failed, so the nerve was sacrificed.

Figure 2 Intraoperative image. After lateralization of the sternocleidomastoid muscle, a mass within the vagus nerve in close contact with the inter nal carotid artery is observed.
The pathology report confirmed the origin of the tumor. The gross examination showed a nodular mass with a size of 5.1 × 4.5 × 3.3 cm. The surface was smooth and, once sectioned, had clear brown appearance and was hard-elastic in consistency. Microscopic examination with routine stain showed spindle-shaped cells with elongated oval nuclei, dense chromatin and eosinophilic cytoplasm arranged in dense hypercellular fascicles containing Verocay bodies (Antoni A areas) alternating with hypocellular areas with hyalinized blood vessels and hemosiderin-laden macrophages (Antoni B areas). Immunohistochemical tests showed diffuse positive staining for S-100 protein with Ki-67proliferative index < 1% (Fig. 3).
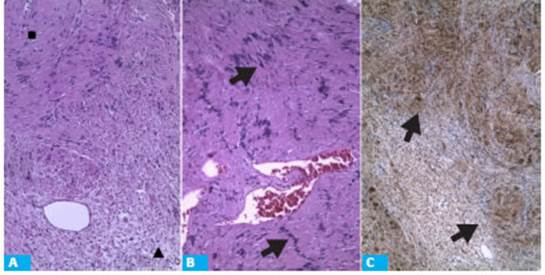
Figure 3 Optical microphotograph, hematoxylin and eosin stain and immunohistochemi cal staining for S-100 protein. A. Optical microphotograph, routine stain (10x) showing proliferation of spindle-like cells with biphasic pattern arranged in Antoni A (■) and Antoni B (▲) areas. B. Optical microphotograph, routine stain (10x), showing Antoni A areas along with Vero cay bodies (arrow). C. Optical micropho tograph, immunohistochemical staining for S-100 protein, showing diffuse posi tive staining within proliferation of cells with biphasic pattern (arrow).
The patient evolved wit hoarseness and underwent fibro-optic laryngoscopy, which shower right vocal cord paralysis.
Schwannomas of the lateral pharyngeal space represent a challenge to the surgeon due to issues in the surgical approach, tumor histology and vascular and nerve structures of the area.
Therefore, preoperative assessment is essential and should provide the best possible diagnostic approach for optimal treatment.
The presence of a mass in the neck with or without an oropharyngeal mass is the most suggestive sign. Physical examination should include the presence of deficits in the territory of the cranial nerves V, VII, IX, X, XI and XII4.
Imaging tests are essential as they provide information about tumor nature, the best surgical approach and probable surgical issues. Nowadays, these tests include CT scan, magnetic resonance imaging (MRI) and angiography.
High-resolution CT with contrast agent is the test of choice as it provides visualization of the tissues within the parapharyngeal space, detects the presence of calcifications and identifies tumor location, aspect, contours and vascularization. Schwannomas appearance can be homogeneous or heterogeneous and show contrast enhancement (leakage of contrast material).
The use of fine needle aspiration is still a matter of debate and is not recommended by most authors, and neither are open biopsy or core needle biopsy.
Surgical resection remains the treatment of choice, although vagus nerve injury is still an unresolved issue, as the tumor originates directly from the nerve fibers. For this reason, new techniques with nerve preservation are needed.
Several techniques have been described: complete tumor removal followed by primary anastomosis or interposition of a nerve graft, complete tumor removal with nerve preservation, tumor enucleation from the adjacent normal nerve fibers, and tumor resection with capsule preservation.
The treatment of choice is tumor enucleation with preservation of the nerve. If it is impossible to find a suitable plane and nerve preservation is technically difficult, end-to-end resection of the segment involved can be done and then anastomosed using microsurgery.
This type of procedure might result in permanent vocal cord paralysis, dysphagia and post-operative paroxysmal cough. The incidence of preoperative vocal cord paralysis is 12%, and 85% after surgery. In such cases, intensive voice therapy should be implemented to compensate.
Acknowledgments
Lucia Belén Giame
REFERENCES
1. Samarakkody ZM, Sayuti KA, Mat Zin AA, Wan Abdul Wahab W, Mohamad I. Coughing on palpation: A rare complication of vagal schwannoma. Malays Fam Physician. 2018; 13(3):40-3. Published 2018 Dec 31. [ Links ]
2. Carvallo G, Pattaro G, Iorio O, Avallone M, Silecchia G. A literature review on surgery for cervical vagal schwannomas. W J Surg Oncol 2015; 13:130. [ Links ]
3. Chiofalo MG, Longo F, Marone U, Franco R, Petrillo A, Pezzullo L. Cervical vagal schwannoma. A case report. Acta Otorhinolaryngol Ital. 2009; 29(1):33-5. [ Links ]
5. Yako T, Goto T, Kitazawa K, Horiuchi T, Kobayashi S. Inter-capsular resection of cervical vagus nerve schwannoma. J Clin Neurosci 2018; 54:161-4. [ Links ]
Received: August 05, 2020; Accepted: October 14, 2020











 texto em
texto em 


