Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista argentina de cirugía
versão impressa ISSN 2250-639Xversão On-line ISSN 2250-639X
Rev. argent. cir. vol.113 no.2 Cap. Fed. jun. 2021
http://dx.doi.org/10.25132/raac.v113.n2.1499.ei
Articles
Retroperitoneal leiomyosarcoma with resection of the vena cava
1 Servicio de Cirugía General. CEMIC. Buenos Aires, Argentina
2 Unidad de Trasplante Renal y Reno-pancreático. CEMIC. Buenos Aires, Argentina
3 Servicio de Cirugía Vascular Periférica. CEMIC. Buenos Aires, Argentina
Vascular leiomyosarcomas are rare mesenchymal tumors originating in the vascular smooth muscle. They most commonly present as slow-growing masses with significant local infiltration; few distant metastases are late symptoms.
The disease was first described by Perl in 1871, and since then less than 300 cases have been reported in the indexed literature, thus posing a challenge for its diagnosis and treatment1.
Vascular leiomyosarcomas occur in women int the 5th and 6th decade of life. The inferior vena cava (IVC) represents the most common site of vascular sarcomas. These tumors are classified into 3 groups according to the level of the IVC involved: above the hepatic veins, between the hepatic veins and the confluence of the renal veins or below the confluence of the renal veins2.
The clinical presentation varies from an incidental finding in imaging tests to pelvic congestion syndrome and lower extremity edema due to compression of the iliac vessels.
Radical en bloc resection with negative margins is the treatment of choice, with reconstruction of the IVC in case collateral drainage is not sufficient. Reconstruction can be performed using vascular prostheses, autografts or vascular grafts from cadaveric donors. Some groups do not recommend reconstruction with prosthesis or native patches.
Neoadjuvant treatments have not achieved good results due to the low replication rate of these tumors; therefore, wide vascular resections of the IVC and even of adjacent organs infiltrated by the tumor are necessary, but this decision must be tailored to each patient3.
The aim of this study was to report the case of a 66-year-old female patient referred to the department of general surgery with a solid retroperitoneal tumor. A computed tomography (CT) scan performed before surgery showed a solid retroperitoneal tumor involving the infrarenal IVC which displaced the entry of both renal veins. The tumor expanded in the lumbar fossa until reaching the second part of the duodenum, exceeding the upper right renal pole (Fig. 1 A, B).

Figure 1 Contrast-enhanced CT scan of the abdomen and pelvis in coronal (A) and axial (B) sections. A large mass is observed in the right hemiabdomen, in close contact with the right renal venal (without infiltration), duodenum, pancreas and retroperitoneal vessels. C: Cavography showing blood flow in the tumor (white arrow), compression of the IVC (black arrow) and collateral flow through the lumbar vessels (arrowhead).
A cavography was performed due to the involvement of the IVC, which showed stenosis of the infrarenal IVC with significant collateral flow through the lumbar vessels (Fig. 1 C).
No distant metastases were found, and the patient was scheduled for surgery with resection of the retroperitoneal tumor and replacement of the IVC with polytetrafluoroethylene (PTFE) graft.
The abdomen was approached via a midline supraumbilical and infraumbilical incision. The Cattell- Braasch and Kocher maneuvers were used to release the duodenal-pancreatic complex and give proximal and distal control of the IVC and both renal veins. The tumor was resected, encompassing the infrarenal IVC. The specimen weighted 3 kg and had a size of approximately 10 x 9 cm (Fig. 2. A, B). Heparin was then administered, the IVC was clamped and flow was restored with a PTFE graft. There was no need to resect adjacent organs, achieving an R0 resection with an operative time of 6 hours without requiring transfusions.
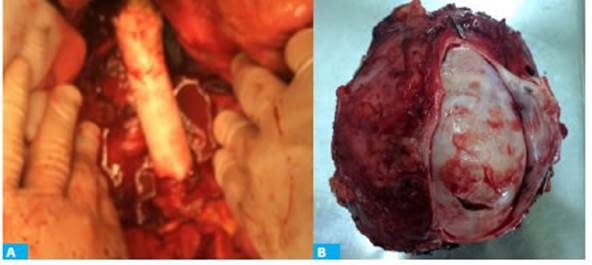
Figure 2 Surgical field after the specimen was removed and the reconstruction was completed (A). Part of the inferior vena cava is attached to the large tumor mass (B).
The patient evolved without complications and was discharged six days after surgery. Anticoagulation was maintained for six months and the patient is currently treated with aspirin.
The pathology report revealed a retroperitoneal leiomyosarcoma with Ki-67 of 25% (Fig. 3 A). There was no need for further treatment. The patient was followed up at one, six and 12 months after surgery with no signs of recurrence and with patent IVC graft (Fig. 3 B).

Figure 3 A. Spindle cells stained with hematoxilyn and eosin (magnification x63) with marked nuclear pleomorphism; hyperchromatic nuclei (arrow). B. Patent PTFE prosthesis used for replacement of inferior vena cava section (arrow)
Vascular leiomyosarcomas are rare tumors and are usually localized in the IVC. They constitute a challenge for surgeons due to their local expansion and need for complex vascular resections. For this reason, the consensus statement performed by a work group of surgeons from many hospitals and published in the Annals of Surgical Oncology in 2016 emphasized the need for multidisciplinary management3.
One of the first papers in the matter was conducted by Hardwigsen et al. and published in the same journal in 2001. In a series of 14 patients undergoing surgery, prosthetic replacement was not necessary in 6 patients, and half of them developed symptoms of venous obstruction, concluding that in wide resections, these symptoms are prevented by and better managed with replacement of the IVC4.
In 2010, Dylami et al. reported their experience with six cases without reconstruction of the IVC who developed lower extremity edema and renal failure, as it had been reported by other authors.
Finally, in 2018 Theodoraki et al. highlighted the need for IVC replacement in a series of five patients undergoing resection of the IVC and renal vein without prosthetic replacement, diverting the venous flow through collaterals. In consequence, inferior extremity edema and renal dysfunction developed as in the study by Dylami et al.
Such series suggest that pelvic congestion and low extremity edema may occur after wide resections of the IVC. These complications may be difficult to manage, adding morbidity for the patient.
The role of radiation therapy as neoadjuvant treatment in unclear due to the low number of cases.
In our case, we could perform total excision of the tumor with resection of infrarenal IVC and reconstruction with ringed PTFE graft, with good postoperative outcomes. We consider that, in case of wide IVC resections, as in our patient, reconstruction of the IVC with graft placement is a valid option supported by the literature, with excellent results when performed by trained surgeons.
Referencias bibliográficas /References
1. Daylami R, Amiri A, Goldsmith B, Troppmann C, Schneider PD, Khatri VP. Inferior vena cava leiomyosarcoma: is reconstruction necessary after resection? J Am Coll Surg. 2010; 210:185-90. http://doi:10.1016/j.jamcollsurg.2009.10.010 [ Links ]
2. Calleja Kempin IJ y col. Resección de leiomiosarcoma de vena cava inferior con reconstrucción mediante prótesis de PTFE anillada. Angiología. 2016. http://dx.doi.org/10.1016/j.angio.2016.08.004 [ Links ]
3. Management of Recurrent Retroperitoneal Sarcoma (RPS) in the Adult: A Consensus Approach from the Trans-Atlantic RPS Working Group. Ann Surg Oncol 2016; 23(11):1-10. http://doi:10.1245/s10434-016-5336-7 [ Links ]
4. Hardwigsen J, et al. Resection of the inferior vena cava for neo plasms with or without prosthetic replacement: a 14-patient se ries. Ann Surg. 2001;233(2):242-9. http://doi:10.1097/00000658-200102000-00014 [ Links ]
Received: July 15, 2020; Accepted: September 09, 2020











 texto em
texto em 


