Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista argentina de cirugía
versão impressa ISSN 2250-639Xversão On-line ISSN 2250-639X
Rev. argent. cir. vol.115 no.1 Cap. Fed. maio 2023
http://dx.doi.org/10.25132/raac.v115.n1.1658
Articles
Ectopic cervical thymoma
1 Servicio de Cirugía General del Hospital General de Agudos Donación Francisco Santojanni. Buenos Aires. Argentina.
2 Servicio de Patología del Hospital Británico. Buenos Aires. Argentina.
Ectopic cervical thymoma is a rare entity (4%) due to an anomaly in embryonic development. The thymus originates from the third pharyngeal pouch and during the 5th week of gestation migrates together with the inferior parathyroid glands to reach its final position. Ectopic thymic tissue may be located anywhere along the descending pathway but is most common near the lower pole of the thyroid gland, from the angle of the mandible to the superior mediastinum1.
There are two universally accepted classification systems:
▪ 1. The Masaoka system (1981) with the modification proposed by Koga (1994).
This system was described for mediastinal thymomas, is based on capsular invasion, and includes 4 stages1:
▪ Stage I: grossly and microscopically completely encapsulated tumor.
▪ Stage II: microscopic capsular invasion into mediastinal fatty tissue or pleura.
▪ Stage III: macroscopic invasion into adjacent organs or vessels.
▪ Stage IVa: dissemination to other thoracic organs.
▪ IVb: distant metastases.
▪ The most relevant prognostic factors are determined by the Masaoka-Koga staging system, histologic type and complete resection of the tumor2.
▪ 2. The WHO classifies thymomas according to the microscopic characteristics of the tumor cells in3:
▪ Type A: epithelial cells with spindle/oval shape; 15- year survival rate near 100%.
▪ Type AB: also known as mixed thymomas; cells with a round or polygonal shape with the features of type A thymoma with a component of lymphocytes with variable density.
▪ Type B: B1 predominantly cortical thymoma, B2 cortical thymoma, B3 well-differentiated thymic carcinoma, depending on the proportion of lymphocytes and emergence of atypia of the neoplastic epithelial cells. Survival at 15 years is 90%.
▪ Type C: cytologic atypia and loss of the organotypical characteristics of the thymus; the latter term is synonymous with thymic carcinoma, which is usually advanced at the time of diagnosis with a 5-year survival rate of 35%.
A 70-year-old woman, with grade II obesity, history of chronic obstructive pulmonary disease (COPD), former smoker of 1 pack/year, and no relevant family history sought medical advice due to a left lateral neck tumor which developed 6 years before, with progressive increase in size over the past year. She did not complain of other symptoms and had no history of thyroid disease. On physical examination, a tumor was palpable on the left lateral side of the neck, measuring approximately 7 × 5 cm, with hard-elastic consistency, and attached to the deep planes in lymph node levels II-III of the neck. Thyroid antibodies were negative and thyroid hormones were within normal ranges. A thyroid ultrasound and Doppler ultrasound of the thyroid gland and soft tissues were performed. The thyroid gland was decreased in size with heterogeneous echogenicity, but no nodular lesions were identified, and vascularization was preserved. A hypoechoic, poorly vascularized heterogeneous mass with regular borders measuring 70 ×40 × 45 mm, was observed in the left lateral cervical region. There were also lesions adjacent to the mass suggestive of lymph nodes; the greatest lesion measured 25 × 8 mm. Ultrasound-guided needle biopsy specimens revealed the presence of hematic material with lymphoid tissue and accumulation of epithelial cells, with slight anisokaryosis and evident nucleolus. Immunohistochemical staining showed that lymphoid cells were diffusely positive for CD3, and epithelial cells were positive for CK (AE1/AE3). Diagnosis: histologic and immunophenotypic findings suggestive of thymoma. Anti-acetylcholine receptor antibodies were negative. A contrast-enhanced computed tomography (CT) scan of the bones of the face, neck and thorax reported the presence of a 47 × 43 × 72 mm enhanced mass in the left lateral region which displaced the primitive carotid artery anteriorly and the internal jugular vein posteriorly (Fig. 1), partially covered by the sternocleidomastoid muscle. The mass reached the parapharyngeal space to the right and lied behind the laryngeal cartilages and the hyoid bone. Lymph nodes were visualized in the left jugulocarotid chain; the largest lymph node measured 11 × 7 mm. In the lower part of the superficial lobe of the left parotid gland, a similar rounded lesion of 13 × 10 mm was detected, which could correspond to an intraparotid lymph node. The mediastinum and axillae were free from lymph nodes. An anatomical variant of the right subclavian artery crossing behind the esophagus (arteria lusoria) was observed in the posterior mediastinum.
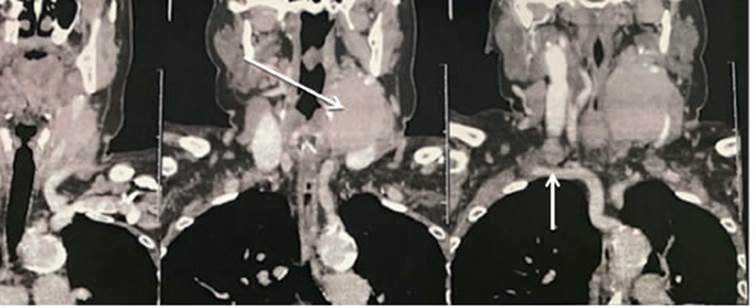
FIGURE 1 Contrast-enhanced computed tomography scan of the neck. The long arrow shows a 47 × 43 × 72 mm enhanced mass with soft tissue density displacing the primitive carotid artery anteriorly and the internal jugular vein posteriorly and reaches the parapharyngeal space to the right. The short arrow indicates an anatomical variant of the right subclavian artery crossing behind the esophagus (arteria lusoria).
Surgery was scheduled on April 12,2021, using a left cervical approach. A semicircular submandibular incision was performed in the neck (Fig. 2). A laterocervical solid mass measuring 7 × 6 cm, with regular borders, was observed in close contact with and displacing the internal jugular vein, the primitive carotid artery and its bifurcation. The upper side was in contact with the parotid gland. The tumor was separated from the carotid vessels by subadventitial dissection. Dissection continued in the caudal direction until the vague nerve was identified. The internal jugular vein and the X cranial nerve were separated, preserving both structures (Fig. 2). The tumor was resected en bloc together with the lower pole of the left parotid gland and adjacent lymph nodes (see Fig. 2). The intraoperative biopsy described a neoplasm consisting of spindle-shaped cells with a large component of small lymphocytes. The tumor was encapsulated and the diagnosis was differed. The patient was discharged on postoperative day two, with no complications or aftereffects; the last follow-up visit was three months later, without clinical abnormalities.

FIGURE 2 A y B. The posterior aspect of the tumor is in contact with the internal jugular vein (VYI, short arrow) and the X cranial nerve (X PAR, long arrow). C: Microscopic examination of the specimen, classified a type AB thymoma according to the WHO classification, with proliferation of spindleshaped cells, small lymphocytes and absence of microscopic capsular invasion.
The pathology report described a solid, lobulated, brownish surgical specimen, hard in consistency and measuring 7 × 6 cm. The microscopic examination classified it as a type AB thymoma according to the WHO classification, with proliferation of spindle-shaped cells with numerous small lymphocytes (Fig. 3). The lesion was encapsulated. Six lymph nodes were free from disease. Immunohistochemical staining showed that the epithelial cells were positive for cytokeratin, lymphocytes were positive for CD5 and CD3, and slightly positive for CD20. Ki-67 proliferative index was 3%. The diagnosis of the mass was stage I thymoma according to the Masaoka staging system of thymoma and type AB thymoma of the WHO classification. Thymomas are the most common mediastinal tumors, and ectopic thymomas represent a diagnostic challenge due to the unusual location of this neoplasm. The peak incidence occurs between the third and fifth decade of life. On presentation, symptoms are due to local mass effects or associated with systemic syndromes; among these, myasthenia gravis is the most common one. The differentiation between benign and malignant thymomas is based on the presence of macroscopic invasion of adjacent structures, metastases or microscopic signs of capsular invasion3.
The preoperative diagnosis of this type of tumor is difficult due to its low prevalence, absence of pathognomonic signs of disease and the fact that the histologic findings obtained from previous needle biopsy may not be specific since the diagnosis is primarily based on the exclusion of other conditions4. Differential diagnoses should be made with congenital neck masses and acquired lesions such as adenomas of the thyroid gland, neck lymph nodes, lymphoproliferative disorders, dermoid or epidermoid cysts or inflammatory lesions5.
In malignant cases, the prognosis and survival rate are determined by complete resection and invasion level (Masaoka-Koga). In advanced stages or recurrent disease, systemic chemotherapy has high response rates. The present case was interpreted as stage I according to the Masaoka-Koga system and type AB of the WHO classification. As the tumor was completely resected, there was no need to add any other complementary treatment. The patient is still undergoing periodic check-ups, with no evidence of remote postoperative complications or recurrence.
Referencias bibliográficas /References
1. Detterbeck FC, Nicholson AG, Kondo KVan Schil P, Morán C. The Masaoka-Koga Stage Classification for Thymic Malignancies Clarification and Definition of Terms. J Thorac Oncol. 2011;6: S1710-S1716. [ Links ]
2. Hyun Oh Park, Sung Hwan Kim, Seong Ho Moon. Ectopic Cervical Thymoma: A Case Report and Review. Korean J Thorac Cardiovasc Surg. 2017; 50(4): 312-5. [ Links ]
3. Okumura M, Ohta M, Tateyama H. The World Health Organization histologic classification system reflects the oncologic behavior of thymoma: a clinical study of 273 patients. Cancer. 2002;94:624- 32. [ Links ]
4. Lee YY, Wang WC, Li CF. Aspiration cytology of an ectopic cervical thymoma misinterpreted as a lymphoproliferative lesion of the thyroid: a case report. Oncol Lett. 2015;10:1255-8. [ Links ]
5. Tsukada J, Hasegawa I, Sato H. Ectopic Cervical Thymoma located in the carotid triangle. Japan Radiology Society. 2013;31:138-42. [ Links ]
Received: July 28, 2021; Accepted: November 24, 2021











 texto em
texto em 


