Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista argentina de cirugía
versão impressa ISSN 2250-639Xversão On-line ISSN 2250-639X
Rev. argent. cir. vol.115 no.4 Cap. Fed. dez. 2023 Epub 29-Nov-2023
http://dx.doi.org/10.25132/raac.v115.n4.1753
Original article
Development of a complex hepatobiliary surgery and liver transplantation unit in a public hospital: a decade after its creation
1Unidad de Cirugía Hepatobiliar Compleja y Trasplante Hepático. Hospital El Cruce, Florencio Varela, Buenos Aires. Argentina.
Background:
Centralizing hepatobiliary disease in specialized centers can reduce morbidity and mortality rates and improve long-term outcomes.
Objective:
The aim of the present study was to describe the clinical and pathological features and surgical outcomes of a series of patients operated on in the Hepatobiliary Surgery and Liver Transplantation Unit of Hospital El Cruce during its first 10 years, as well as the scientific and educational activity of its members.
Material and methods:
We conducted a descriptive and retrospective study. The information was retrieved from a prospective database. The procedures were classified according to their complexity. An analysis was conducted on liver transplantations (LTs), liver resections and complex biliary procedures, performed from 2013 to 2022.
Results:
Of 1449 surgical procedures, 832 were high-complexity interventions (58%). A total of 452 LTs were performed, 14 (3%) were combined liver and kidney transplantations; overall transplant survival was 83%, 77% and 75% at 1, 3 and 5 years, respectively. Primary graft dysfunction was observed in 5 cases (1.1%). There were 254 liver resections; 58 cases (23%) were related to benign liver diseases, 155 (61%) to malignancies, and 41 (16%) were associated with living donor transplants. Overall morbidity was 27% and in-hospital mortality was 2%. A total of 106 bilio-digestive bypass procedures were carried out, 53 in patients with bile duct injury. Thirty-day morbidity was 42%, and most cases were minor complications (28%). Other procedures included 17 cephalic pancreaticoduodenectomies and 3 splenectomies and distal pancreatectomies. We have published numerous papers, delivered presentations and courses, and implemented a fellowship program in the specialty since 2015.
Conclusion:
Centralizing hepatobiliary diseases at a high-complexity center led to comparable outcomes with those reported in international series.
Keywords: public hospital; surgery department; hospital units development; bile duct; liver surgery; liver transplantation
Introduction
Hepatobiliary and pancreatic surgery is a subspecialty of general surgery. Centralizing the disease in specialized centers can reduce morbidity and mortality rates and improve long-term outcomes. In Argentina, despite the long-standing practice of hepatobiliary surgery as a subspecialty, liver transplantation has enabled the possibility of performing much more complex procedures. Before 2007, there were no high-volume public centers with hepatobiliary surgery and liver transplantation capabilities in the province of Buenos Aires. The highcomplexity Hospital El Cruce (HEC) working in network was established in that year, with the aim of managing high complexity diseases1,2,3. The aim of the present study was to describe the clinical and pathological features and surgical outcomes of a series of patients operated on in the Complex Hepatobiliary Surgery and Liver Transplant Unit of Hospital El Cruce during its first 10 years, as well as the scientific and educational activity of its members.
Material and methods
We conducted a retrospective and descriptive study of the health care and surgical activity performed from January 1, 2013, to December 31, 2022. The information was retrieved from a prospective database. The procedures were classified according to their complexity. High-complexity procedures included LT, liver resections and complex biliary procedures. The data analyzed in LT were etiology, situation in the waiting list, type of transplant and survival. Comparative data was retrieved from the Central Reporting and Statistics of the National Organ Procurement and Transplantation Information System of Argentina (SINTRA)4. The etiology, type of liver resection performed5, morbidity and mortality were analyzed. Complex biliary procedures included bilio-digestive bypass procedures, either due to bile duct resection or repair. Pancreatic surgeries were only performed under exceptional circumstances, as pancreatic diseases fell under the responsibility of the department of general surgery. Teaching activity (fellowship program and courses) and scientific activity (publications and reports) during this period were considered.
Results
The number of visits to the outpatient clinic and surgical procedures experienced a steady increase, resulting in a total of 7485 visits and 1440 procedures, which were carried out on 947 patients (Table 1).
TABLE 1 Health care activity by year
| Activity | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Liver transplantations | 31 | 36 | 44 | 42 | 60 | 52 | 55 | 31 | 54 | 47 | 452 |
| Liver resections | 0 | 0 | 23 | 30 | 25 | 32 | 30 | 27 | 34 | 53 | 254 |
| Complex biliary procedures | 0 | 0 | 12 | 19 | 12 | 15 | 12 | 6 | 10 | 20 | 106 |
| Other procedures | 13 | 42 | 68 | 51 | 52 | 40 | 71 | 52 | 95 | 144 | 628 |
| Outpatient clinic visits | 63 | 240 | 470 | 594 | 655 | 786 | 1138 | 848 | 1218 | 1473 | 7485 |
Of these, 800 (84.5%) patients lived in the province of Buenos Aires, 589 lived in the outskirts of Buenos Aires and 211 in the province’s inland. Fifteen patients live in the City of Buenos Aires (CABA), and 132 in other provinces. Excluding transplant patients who require a financial backer to be included on the waiting list due to regulations of the Instituto Nacional Central Único Coordinador de Ablación e Implante (INCUCAI), 61% did not have social security coverage.
We identified three stages: The first stage covers the years 2013 and 2014 when we performed only LT and transplant-related complications (average 33.5 high-complexity procedures per year). The second period spans from 2015 to 2019. During this time, we started with complex hepatobiliary surgeries, resulting in a substantial rise to an average of 92.6 highly complex procedures annually. In 2020, the SARS-CoV-2 pandemic resulted in a decrease in LTs and other surgical procedures, causing a 23% decrease in surgical activity (64 procedures). In 2021 and 2022, we conducted 120 complex procedures (Table 1), resulting in a significant surge.
Liver transplantation
A total of 452 LTs were carried out on 438 patients, comprising 449 adults and 33 pediatric cases. Fourteen patients underwent combined liver and kidney transplantation. During the analyzed period, 3719 LTs from deceased donors were performed in Argentina at 33 authorized centers. Among them, the HEC performed 12.2% of the transplants, being the only public transplant center among the top five4. Only the right lobe of split livers was implanted in 134 patients. Of these patients, 30 underwent the procedure at HEC, representing 22.4% of the national activity and 6.8% of the entire HEC series.
The most common etiologies requiring LT were chronic liver disease secondary to hepatitis C virus infection, alcoholic liver disease and autoimmune hepatitis (Table 2). An association with hepatocellular carcinoma (HCC) was observed in 138 patients.
TABLE 2 Methods for registration, type and etiology of 452 livers transplantations
| Methods for registration in the waiting list | n (%) |
|---|---|
| MELD | 261 (58%) |
| AP/APS | 140 (31%) |
| Emergency | 51 (11%) |
| Type of transplantation | |
| Liver transplantations | 438 (97%) |
| Combiend liverand kidney transplantations | 14 (3%) |
| Etiologies | |
| Alcoholic cirrhosis | 88 (19.4%) |
| HVC-related cirrhosis | 86 (19%) |
| Autoimmune hepatitis | 73 (16%) |
| Fulminant hepatic failure | 48 (10.6%) |
| Primary biliary cholangitis | 38 (8.4%) |
| NASH-related cirrhosis | 25 (5.5 %) |
| Cryptogenic cirrhosis | 21 (4.6%) |
| Liver retransplantations | 18 (4%) |
| Alcohol intake and HVC-related cirrhosis cofactor | 14 (3.1%) |
| Primary sclerosing cholangitis | 9 (2%) |
| Secondary biliary cirrhosis | 8 (1.8%) |
| HVB-related cirrhosis | 7 (1.5%) |
| Polycystic liver disease | 4 (0.9%) |
| Familial amyloid polyneuropathy | 4 (0.9%) |
| Others | 10 (2.2%) |
AP: additional points; APS: Argentine Prioritization System; HVC: hepatitis B virus; HCV; hepatitis C virus; MELD: model of end liver disease; NASH: non-alcoholic steatohepatitis
Registration for waiting list was determined by the current model of end-stage liver disease (MELD) in 58% of cases, through standardized or non-standardized exceptions (MELD exception system) in 31% and based on emergency status in 11%. After excluding additional points and emergencies, mean MELD score was 27 at transplant. Of the 138 patients with HCC undergoing LTs, 112 received additional points. A total of 18 retransplantations were performed, 4 of them in patients who received their first transplant at another center and 14 (3.1%) at the HEC. The reasons for retransplantation were chronic rejection in 9 cases, vascular complications in 6, ischemic cholangiopathy in 2 and primary graft dysfunction in 1.
Overall survival of LT was 83%, 77% and 75% at 1, 3 y 5 years, respectively (Figure 1, a). One year survival after split LT was 80% and mean length of hospital stay was 12 days.
In-hospital mortality was evaluated in three similar periods (Figure 1, b) Primary graft dysfunction occurred in 5 cases (1.1%) and only one patient could be retransplanted.
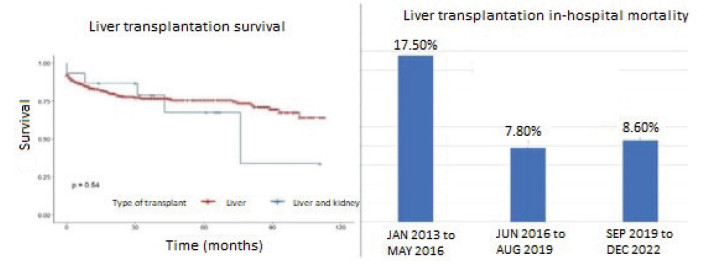
FIGURE 1 a) Survival of liver transplantation and combined liver and kidney transplantation. b) In-hospital mortality of liver transplantation by periods.
There were 21 vascular complications (4.6%): 10 acute arterial thromboses resulting in 8 successful arterial revascularizations and 2 retransplantations; 1 case of hepatic artery aneurysm requiring reoperation and retransplantation; and 5 late arterial thrombosis cases resulting in 3 retransplantations and 2 percutaneous interventions, 3 cases of portal vein thrombosis (1 treated with catheter-directed thrombolysis, 1 with jump graft reconstruction, and 1 requiring retransplantation), 1 case of acute arterial and portal thrombosis in a patient with bile duct injury (BDI) who presented with cholangiocarcinoma in explant and subsequently died, and 1 case of late portal vein stenosis. Biliary complications occurred in 66 cases, (14.6%) and included 39 anastomotic strictures, 5 cases of ischemic cholangiopathy, 5 cases of anastomotic fistulas, 7 non-anastomotic fistulas, 8 cases of choledocholithiasis, and 2 cases of bilomas.
Liver resections
A total of 254 liver resections were performed, comprising 188 minor hepatectomies and 66 major hepatectomies (26%). Fifty-eight cases (23%) were related to benign liver diseases, 155 (61%) to malignancies, and 41 (16%) were associated with living donor transplants. The etiologies are summarized in Table 3.
TABLE 3 Type and etiology of 254 liver resections
| Type of resection | n (%) |
|---|---|
| Minor liver resection | 188 (74) |
| Major liver resection | 66 (26) |
| Etiology | |
| Benign diseases | 58 (23) |
| Malignancies | 155 (61) |
| Living-related donor | 41 (16) |
| Benign disease | |
| Adenoma | 14 (24) |
| Cavernous hemangioma | 9 (15. 5) |
| Polycystic liver disease | 8 (13.8) |
| Cystic neoplasm | 8 (13.8) |
| Hydatid disease | 5 (8.6) |
| Focal nodular hyperplasia | 2 (3.4) |
| Intrahepatic duct lithiasis | 2 (3.4) |
| BDI | 2 (3.4) |
| Others | 8 (13.8) |
| Malignancies | |
| Colorectal liver metastasis | 53 (34) |
| HCC | 48 (31) |
| Gallbladder cancer | 12 (7.7) |
| Klatskin tumor | 10 (6.5) |
| Inthrahepatic cholangiocarcinoma | 8 (5) |
| NET metastasis | 7 (4.5) |
| Other metastasis | 14 (9) |
| Other primary tumors | 3 (2) |
BDI: bile duct injury; HCC: hepatocellular carcinoma; NET: neuroendocrine tumor
Overall morbidity was 27% and in-hospital mortality was 2%. Of note, 7 hepatectomies involved vascular resection, 19 were combined with multivisceral resection, 7 were associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) procedures, 8 were hepatectomies for polycystic liver disease, and 2 were for bile duct injuries (BDI).
Forty-eight resections were performed in patients diagnosed with HCC, and among them 31 were cirrhotic patients. Morbidity in these patients was 47% (88% were minor complications), with a 2% mortality rate. Survival rate at 1, 3, 5 and 5 years were 82%, 75% and 71%, respectively. Forty-one liver resections were performed for living donor transplants in pediatric patients over a 2.5-year period. This represents 34% of the activity of this practice in Argentina.
Complex biliary procedures
A total of 106 bilio-digestive bypass procedures were carried out, 53 in patients with BDI; 7 of these procedures were through laparoscopy, but 2 of them required conversion. Hepaticojejunostomy was performed in 9 cases (17%) (Table 4).
TABLE 4 Complex biliary procedures
| Bilio-digestive bypass | n (%) |
|---|---|
| BDI | 53 (50) |
| Open approach | 48 |
| Laparoscopic approach | 5 |
| Bile duct stricture after LT | 21 (19.8) |
| Rome protocol first | 14 |
| Surgery first | 7 |
| Palliative | 11 (10.4) |
| Cholangiocarcinoma | 6 (5.7) |
| Common bile duct lithiasis | 5 (4.7) |
| Choledocal cyst | 4 (3.8) |
| Previuos choledochoduodenostomy | 3 (2.8) |
| Gunshot injury | 1 (0.9) |
| Biliary neuroendocrine neoplasm | 1 (0.9) |
| Anastomotic dehiscence | 1 (0.9) |
BDI: bile duct injury LT: liver transplantation
Thirty-day morbidity was 42%, and most cases were minor complications (28%). Strictures occurred in 9.5% of the cases (n = 5) within a median of 17.2 months. Two patients were successfully managed with percutaneous dilation and the other 3 required reconstruction of the hepaticojejunostomy. During the study period, 84 patients with BDI were evaluated and managed; 40% of them presented complex BDIs6. The average number of patients referred with this condition was 10.3/year, which decreased to 3 in 2020, but rose to 19 in 2022. Twenty-one bilio-digestive bypass procedures were performed for benign strictures in transplant patients (4.6% of all LT); 14 of them had been previously unsuccessfully managed using the Rome protocol, while 18 cases were successfully solved with this method.
There were 29 minor liver resections, 4 major liver resections and 10 bilio-digestive bypass procedures entirely performed by laparoscopic approach. The other procedures not previously included (n = 628), were percutaneous drainage catheter placement (n = 197), and less complex biliary procedures such as 27 laparoscopic cholecystectomies and 9 cases of biliary tract exploration with primary closure. Other procedures included 17 cephalic pancreaticoduodenectomies and 3 splenectomies and distal pancreatectomies. The mortality rate of pancreatic surgery was 5%.
A total of 383 patients with diagnosis of HCC were evaluated. Of these, 138 received LT as the primary treatment, 156 underwent transcatheter arterial chemoembolization (TACE) with 41 as a bridge to LT, 48 underwent liver resection, 16 received systemic treatments, 1 underwent radiofrequency ablation, and 24 received palliative treatment7.
Regarding the national impact of the SARS-CoV-2 pandemic, scheduled surgeries decreased at all centers and the number of LTs was affected by donor shortages8. During 2020, the number of procedures in our unit decreased by 36.6%, and there was a 44.8% decrease in LTs and 40% decrease in biliary procedures. The number of hepatectomies did not decrease significantly (39 versus 42) but we performed 11 living related donor hepatectomies. The number of outpatient clinic visits decreased by 34%. During the period with the highest impact (March 20 through October 16, 2020), we were able to perform 21 hepatectomies, 16 LTs and 5 bilio-digestive bypass procedures.
Research, teaching and continuous education
We wrote six chapters in books of the specialty, published 12 articles in journals indexed in PubMed and 4 in other journals, performed 44 presentations in Argentine congresses of surgery, 26 in other Argentine congresses and 31 in international congresses. The HEC hosted 7 conferences and courses, while the Argentine Chapter of the International Hepato Pancreato Biliary Association (AC-IHPBA) organized 5 courses. Finally, we received 3 awards and 6 mentions.
Since 2015, we have started with the fellowship program with one fellow per year. The program has a duration of three years and includes an option for a chief resident. We prioritize health care, theoretical training, and the development of skills and abilities. Fellows actively participate in health care activities and in most procedures.
Discussion
Florencio Varela is in the southern area of Great Buenos Aires (2nd belt), about 27 km from downtown Buenos Aires, and has a population of 497,818 inhabitants1. Hospital El Cruce is the nation’s first high-complexity health care center within the public system structured for network collaboration. It is a self-sufficient hospital jointly funded by the national government and the province of Buenos Aires. It was opened in 2007 and has an area of influence of more than two million people, considering the entire network. The network is made up of the following hospitals: Mi Pueblo in Florencio Varela, Evita Pueblo in Berazategui, Iriarte in Quilmes, Oller in San Francisco Solano, Oñativia and Lucio Meléndez in Almirante Brown. These medium complexity hospitals had to refer complex conditions (cardiovascular diseases requiring interventional cardiology procedures or cardiovascular surgery, neurosurgery, pediatric intensive care, or therapeutic endoscopy, among others) to institutions in La Plata or the city of Buenos Aires2. Although defining high complexity is challenging, the HEC considers it as the ability to manage patients with complex diseases that demand precise care, as well as a highly specific human, technological and structural approach, or that cannot be provided by the hospitals in the network3. Networking is part of the health system’s strategy to integrate service networks of increasing complexity, to provide timely, equitable and high-quality care through inter-institutional agreements.
During its first years, the HEC became a referral center for certain specialties (neurosurgery, cardiology and cardiovascular surgery, ophthalmology and gastroenterology). Between 2011 and 2012, the board of directors made the decision that a high-complexity hospital must perform organ transplants. The activity started with heart transplantation and bone marrow transplantation. The activities of the Liver Transplant Unit began in early 2013 with the initial LT procedure. Soon afterwards, it earned a reputation as a referral center, taking in patients not only within the network but also from all over the country. It has since become one of the leading centers, performing the highest number of liver transplants in adult patients using cadaveric donors.
Since December 2015, the unit has also been authorized to perform pediatric transplants, although the priority for this group of patients is Hospital Garrahan, which is also considered a comprehensive community health care service. The kidney transplant program started later, motivated by the need for performing combined liver and kidney transplantation in a group of patients. We evaluated the impact of initiating our transplant activity in the public setting.
Access to liver transplants for adults in Argentina’s public health care system significantly increased by 40% following the launch of the HEC program. Although the impact of this program was not global, it has been especially beneficial for a population that previously faced challenges accessing LT. When we compared the national transplant activity with that of the HEC, we saw that one-third of our patients received “livers that nobody wants”9 (grafts rejected 12 times before) without statistically significant differences in terms of primary graft dysfunction, early extubation, dialysis, length of stay in the intensive care unit (ICU), length of hospital stay, or graft and patient survival10. Elder patients, SPLIT and length of stay in ICU were the main causes of graft rejection11. Considering the position on the waiting list determined by MELD score, the waiting time was substantially shorter in our center (19 days vs. 57 days); moreover, almost a quarter (22.5%) of the split livers distributed during the period analyzed were accepted. This showed significant graft acceptance, regardless of how patients evolved later12. Although the surgical team had prior experience, the learning curve of transplantation extends beyond just the surgical team and includes the entire hospital. We observe initially acceptable but higher in-hospital mortality that subsequently decreased during the following periods (Fig. 1, b) Survival rates of patients and grafts have been similar to those of international series13,14, particularly over the past few years (Fig. 1, a).
As for hepato-biliary surgery, the specialized staff from the start enabled us to achieve morbidity and mortality rates similar to those of the most important centers15. The inclusion of fellows facilitated the training of new specialized resources and led to valuable advancements in clinical research and teaching. We deem this development to have been significant in the past years. We proved that applying laparoscopic surgery for highly complex hepato-biliary diseases with an experienced team and suitable facilities at a public center, results in low morbidity and mortality rates. The positive correlation between volume and outcome in hepato-biliary surgery has been demonstrated, and the centralization of liver surgery in specialized “high-volume” hospitals has figured prominently in the debate on improving quality of health care. The factors that contribute to this improvement include a better understanding of anatomy, more precise patient selection, improved perioperative evaluation, and optimized management of complications. High volume is generally associated with better results, as evidenced by numerous studies that have demonstrated lower mortality rates and higher survival rates15,16.
Within the first 10 years, our unit grew into a significant referral center for complex hepatobiliary diseases, holding a prominent position in adult liver transplantation with cadaveric donor; our high standards provided excellent care to a population who had no previous easy access to treatment in this field.
In conclusion, based on the presented experience, we can state that centralizing hepatobiliary diseases at a high-complexity center resulted in achieving comparable outcomes to those reported in international series.
Our commitment for the future is to sustain and improve these objectives.
Referencias bibliográficas /References
1. INDEC, Instituto Nacional de Estadísticas y Censo de la República Argentina. INDEC: Instituto Nacional de Estadísticas y Censo de la República Argentina [Internet]. Gob.ar. [citado el 5 de junio de 2023]. Disponible en: https://www.indec.gob.ar/ [ Links ]
2. Medina A, Marini JE. Hospital El Cruce "Dr. Néstor Carlos Kirchner": Alta complejidad en red. Rev Argent Salud Pública. 2010;1. [ Links ]
3. Matera FJ. Pros y contras de la superespecialización. Rev Argent Cirug. 2018;110(Suplemento 1): S187-246. [ Links ]
4. Gov.ar. [citado el 5 de junio de 2023]. Disponible en: https://cresi.incucai.gov.ar. [ Links ]
5. Strasberg SM, Belghiti J, Clavien PA, Gadzijev E, Garden JO, Lau WY, et al. The Brisbane 2000 terminology of liver anatomy and resections. HPB (Oxford) [Internet]. 2000;2(3):333-9. [ Links ]
6. de Santibañes E, Ardiles V, Pekolj J. Complex bile duct injuries: management. HPB (Oxford) [Internet]. 2008;10(1):4-12. [ Links ]
7. Beltrame C, Sandoval V, Bueno D, Quiñónez ML, Poupard E, Lenz M. Managing hepatocellular carcinoma in cirrhotic patients in a national hospital in Argentina. HPB. O023. Disponible en: https:// www.hpbonline.org/article/S1365-182X(20)30450-0/pdf [ Links ]
8. Gondolesi GE, Reyes-Toso ML, Bisigniano L, De Santibañes M, Pekolj J, Maurette R. Impacto de la pandemia por COVID-19 sobre el trasplante hepático en la Argentina. Otro daño colateral. Medicina (B Aires). 2020;80(6):71-82. [ Links ]
9. Sotiropoulos GC, Lang H, Saner FH, Beckebaum S, Wandelt M, Molmenti EP, et al. Long-term results after liver transplantation with "livers that nobody wants" within Eurotransplant: a center's experience. Transplant Proc [Internet]. 2008;40(9):3196-7. [ Links ]
10. Quiñónez EG, Daciuk N, Poupard M, Durand Azourduy JP, Lenz M, Fernández ME, et al. Evaluation of liver transplant results with "livers that nobody wants". HPB (Oxford) [Internet]. 2018;20: S29. [ Links ]
11. Daciuk N, Quiñónez EG, Beltrame MC, Sandoval RV, Del Bueno ML, Mattera FJ. How unwanted are livers that nobody wants? HPB (Oxford) [Internet]. 2020;22: S377. [ Links ]
12. Daciuk NI, Quiñónez EG, Poupard M, Vergara Sandoval RM, Mattera FJ. Access to grafts in a liver transplant center: Does it rely on the severity of the waiting list population? Transplant Proc [Internet]. 2018;50(2):387-90. [ Links ]
13. European Liver Transplant Registry [Internet]. Eltr.org. [citado el 5 de junio de 2023]. Disponible en: http://www.eltr.org [ Links ]
14. Stepanova M, Wai H, Saab S, Mishra A, Venkatesan C, Younossi ZM. The outcomes of adult liver transplants in the United States from 1987 to 2013. Liver Int [Internet]. 2015;35(8):2036-41. [ Links ]
15. Quiñónez EG, Sandoval V, Poupard R, Cristiano M, Lenz A, Mattera M. Consecutive series of liver resections. Analysis of morbimortality in a newly created center. HPB. 19. [ Links ]
16. Chang CM, Yin WY, Wei CK, Lee CH, Lee CC. The combined effects of hospital and surgeon volume on short-term survival after hepatic resection in a population-based study. PLoS One [Internet]. 2014;9(1): e86444. [ Links ]
17. Franchi E, Donadon M, Torzilli G. Effects of volume on outcome in hepatobiliary surgery: a review with guidelines proposal. Glob Health Med [Internet]. 2020;2(5):292-7. [ Links ]
Received: May 20, 2023; Accepted: September 13, 2023











 texto em
texto em 



