Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista argentina de cirugía
versão impressa ISSN 2250-639Xversão On-line ISSN 2250-639X
Rev. argent. cir. vol.115 no.4 Cap. Fed. dez. 2023 Epub 29-Nov-2023
http://dx.doi.org/10.25132/raac.v115.n4.1731
Original article
Result of immediate prepectoral implant-based breast reconstruction
1División Cirugía Plástica, Hospital de Clínicas José de San Martín. Buenos Aires. Argentina
2División Cirugía General, Hospital Británico. Buenos Aires. Argentina
Background:
Prepectoral implant-based breast reconstruction has recently been added to the armamentarium for breast reconstruction. This technique provides natural-looking breasts, avoids complications, such as animation deformity, and reduces postoperative pain.
Objective:
The aim of this study was to describe the surgical outcomes in a series of patients undergoing immediate prepectoral breast reconstruction with silicone implants.
Material and methods:
A descriptive and retrospective study was carried out with review of the medical records and pathology reports of patients who underwent surgery using the described technique for invasive carcinoma, non-invasive carcinoma, and sarcoma of the breast from March 2018 to December 2021. All the patients were evaluated preoperatively with digital mammography and had fat coverage thickness in the operated breast > 2 cm.
Results:
A total of 52 reconstructions were performed on 40 patients. Mean age was 52 age (range 30- 76). The nipple sparing mastectomy was undertaken in all the cases. There were no major complications during the 40-month average follow-up. None of the patients experienced animation deformity, implant displacement, or rotation. After one year of follow-up, three patients who underwent postmastectomy radiotherapy showed grades III and IV capsular contracture. The aesthetic results were excellent and good in 40 breasts (80.0%), fair in 8 breasts (12.0%) and insufficient in 4 breasts (8.0%). Four breasts (7.7%) required surgical revision in the immediate postoperative period.
Conclusions:
Immediate prepectoral implant-based breast reconstruction is a feasible technique with enduring results and high level of satisfaction.
Keywords: prepectoral breast reconstruction; nipple sparing mastectomy; implant breast reconstruction
Introduction
In 1951, Rice and Stickler described mastectomy with preservation of skin and nipple areola complex (NAC) for the first time for the treatment of a benign breast disease1. Then, in 1962, Freeman introduced the term subcutaneous mastectomy, which was used until about 2003, when it became known as skin-sparing or NAC-sparing mastectomy2. Immediate prepectoral implant-based breast reconstruction is becoming the standard of care following NAC-sparing mastectomy3,4. The routine use of various types of mesh in association with the prepectoral technique has been described in several publications5,6,7.
Adequate selection of patients with cutaneous tissue coverage > 2 cm results in good outcomes without adding these materials to the reconstructive process8,9,10.
Prepectoral implant-based breast reconstruction is a technique that spares muscle and has recently been added to the armamentarium for breast reconstruction7.
With this technique, the implant is placed on the pectoralis major muscle in the subcutaneous plane, preserving the anatomical integrity of the muscle, eliminating animation deformity5,6 and reducing pain8,9,10. It also provides the reconstruction with a more natural appearance11.
The aim of this study was to describe the surgical outcomes in a consecutive series of patients undergoing immediate prepectoral breast reconstruction with silicone implants.
Material and methods
We conducted a retrospective review of 52 immediate single-stage prepectoral breast reconstructions in 40 patients who underwent NAC- sparing mastectomy between March 2018 and December 2021. All the patients signed an informed consent form approved by the Committee on Ethics of the institution.
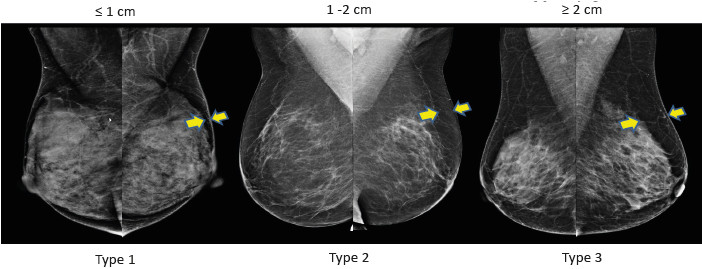
The patients were selected based on the findings of a preoperative digital mammogram. Patients were eligible if the thickness of the subcutaneous tissue in the upper breast flap was ≥ 2 cm. A single operator evaluated all mammograms, and measurements were obtained with OSIRIX® software (available at www.osirix-viewer.com). Breast tissue coverage measurements were reported in centimeters and millimeters. The patients were classified as type 1 to type 3 tissue coverage according to the thickness of the breast subcutaneous tissue: type 1: tissue coverage between 0 and 1 cm; type 2: between 1 and 2 cm; and type 3: > 2 cm (Fig. 1). The inclusion criteria were type 3 patients based on breast tissue coverage (subcutaneous tissue thickness of 2 cm or greater), small-to-moderate sized breasts (cup size A-B, 200-500g) stage I-II invasive carcinoma, carcinoma in situ (stage 0) and sarcoma, with grade 1 and 2 ptosis.
The exclusion criteria were inflammatory carcinoma, skin involvement, abnormal nipple secretion, previous radiotherapy, hypertrophic and ptotic breasts, recent (last 12 months) peri- or subareolar surgery, and smoking habits (> 12 cigarettes/day). A survey was conducted among all patients to assess their level of satisfaction with the aesthetic outcomes rated as poor, fair, good, and excellent.
Results
A total of 40 patients were operated on with the technique described. Mean age was 52 years (range 30-76).
Twenty-eight patients underwent unilateral therapeutic mastectomy (23 for invasive carcinoma, 4 for ductal carcinoma in situ, and 1 for sarcoma), while 12 BRCA-positive patients underwent bilateral mastectomy to reduce risk. Sentinel lymph node biopsy was performed through a separate incision during the 40 therapeutic mastectomy procedures. Six patients with a positive lymph node biopsy underwent level I and II axillary lymph node dissection.
After mastectomy, the breast implant was placed in the prepectoral space via a 10-cm submammary incision (Fig. 2 a-b-c).
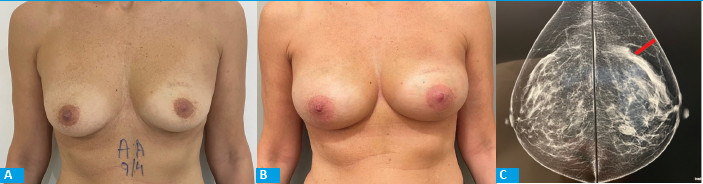
FIGURE 2 Result of prepectoral reconstruction with anatomical implants. A: Preoperative frontal view. B: Postoperative frontal view. C: Preoperative mammogram showing the subcutaneous tissue thickness.
In all the cases, we used microtextured anatomical implants with a volume between 225 and 495 cm3. The implants were not covered by mesh in any of the cases.
A drain was placed in the mastectomy pocket and another one in the axilla after axillary lymph node dissection. Immediate contralateral breast symmetrization was not performed in any patient. Length of hospital stay was one day in 23 cases and two days in 17.
There were no major complications. Four breasts (7.7%) required surgical revision in the immediate postoperative period. After a mean follow- up period of 40 months, no animation deformities, implant displacement of rotation, tumor persistence or recurrence were observed. Three patients who received postmastectomy radiotherapy on the reconstructed breast developed Baker grade III or IV capsular contracture at one year.
The aesthetic results were categorized by the patients as excellent and good in 40 breasts (80.0%), fair in 8 breasts (12.0%) and poor in 4 breasts (8.0%).
Discussion
Implant-based breast reconstruction is a feasible technique with enduring results. Although submuscular reconstruction has been routinely performed12,13,14, prepectoral implant-based reconstruction has recently been reported as the option to avoid muscle injury and its associated morbidity15.
Placing the implant in the prepectoral plane simplifies reconstruction and reduces pain16,17,18, animation deformity, and functional impairment of the muscle19,20. The feasibility and efficacy of prepectoral reconstruction has already been well documented by different authors21,22,23.
Gabriel et al. did not find any association between the postoperative complications of this technique and body mass index, but they observed a relationship with smoking habits and diabetes21.
In a series of 52 prepectoral reconstructions conducted by Sigalove et al., the authors compared the outcomes between 34 individuals who underwent postmastectomy radiotherapy and 18 who did not. The results showed a good tolerance in the entire group, with no differences in short-term adverse effects or capsular contracture in any of the cases22.
In Argentina, Serrano et al. demonstrated good cosmetic results, low morbidity and high level of patient satisfaction in a series of 98 mastectomies using the same reconstructive technique23.
Success with this technique relies on the careful selection of patients with cutaneous thickness > 2 cm and the implementation of meticulous surgical techniques24,25.
In conclusion, the study demonstrated that prepectoral implant-based breast reconstruction, performed in a single stage immediately after mastectomy while preserving the areola-nipple complex in patients with fatty tissue coverage > 2 cm, is a safe and simple technique enabling immediate breast reconstruction without the disadvantages associated with subpectoral implant placement. This technique has high level of satisfaction with aesthetic results and without recurrence or tumor persistence.
Referencias bibliográficas /References
1. Rice CO, Strickler JH. Adeno-Mammectomy for Benign Breast Lesions. [(accessed on 8 November 2022)]. Surg Gynecol Obstet. 1951;93:759-62. Disponible online: https://europepmc.org/article/med/14893082 [ Pub Med] [Google Scholar] [ Links ]
2. Freeman BS. Subcutaneous mastectomy for benign breast lesions with immediate or delayed prosthetic replacement. Plast Reconstr Surg Transplant Bull. 1962;30:676-82. doi: 10.1097/00006534-196212000-00008. [ Links ]
3. Bostwick J. Reconstruction after mastectomy. Surg Clin N Am. 1990;70:1125-1140. doi: 10.1016/S0039-6109(16)45234-5. [ Links ]
4. Abbate O, Rosado N, Sobti N, Vieira BL, Liao EC. Meta-analysis of prepectoral implant-based breast reconstruction: guide to patient selection and current outcomes. Breast Cancer Res Treat. 2020;182(3):543-54. [ Links ]
5. Li Y, Xu G, Yu N, Huang J, Long X. Prepectoral versus subpectoral implant-based breast reconstruction: a meta-analysis. Ann Plast Surg. 2020;85(4):437-47. [ Links ]
6. Mirhaidari SJ, Azouz V, Wagner DS. Prepectoral versus subpectoral direct to implant immediate breast reconstruction. Ann Plast Surg. 2020;84(3):263-70. [ Links ]
7. Mangialardi ML, Salgarello M, Cacciatore P, Baldelli I, Raposio E. Complication rate of prepectoral implant-based breast reconstruction using human acellular dermal matrices. Plast Reconstr Surg Glob Open. 2020;8(12):e3235. [ Links ]
8. Reitsamer R, Peintinger F, Klaassen-Federspiel F, Sir A. Prepectoral direct-to-implant breast reconstruction with complete ADM or synthetic mesh coverage - 36-Months follow-up in 200 reconstructed breasts. Breast. 2019;48:32-7. [ Links ]
9. Vidya R, Iqbal FM. A Guide to Prepectoral Breast Reconstruction: A New Dimension to Implant-based Breast Reconstruction. Clin Breast Cancer. 2017;17(4):266-71. [ Links ]
10. Sigalove S, Maxwell GP, Sigalove NM, Storm-Dickerson TL, Pope N, Rice J, et al. Prepectoral implant-based breast reconstruction: rationale, indications, and preliminary results. Plast Reconstr Surg. 2017;139(2):287-94. [ Links ]
11. Fracol M, Qiu CS, Chiu MW, Feld LN, Sood R, Mioton LM, et al. The relationship between animation deformity and patient-reported outcomes: application of the BREAST-Q to a quantitative stratification of animation severity. Plast Reconstr Surg. 2020;145(1):11-7. [ Links ]
12. Nigro LC, Blanchet NP. Animation deformity in postmastectomy implant-based reconstruction. Plast Reconstr Surg Glob Open. 2017;5(7):e1407. [ Links ]
13. Becker H, Fregosi N. The impact of animation deformity on quality of life in post-mastectomy reconstruction patients. Aesthet Surg J. 2017;37(5):531-6. [ Links ]
14. Gabriel A, Sigalove S, Sigalove NM, et al. Prepectoral revision breast reconstruction for treatment of implant-associated animation deformity: a review of 102 reconstructions. Aesthet Surg J. 2018;38(5):519-26. [ Links ]
15. Bernini M, Calabrese C, Cecconi L, Santi C, Gjondedaj U, Roselli J, et al. Subcutaneous direct-to-implant breast reconstruction: surgical, functional, and aesthetic results after long-term follow-up. Plast Reconstr Surg Glob Open. 2016;3(12):e574. [ Links ]
16. Cronin TD, Gerow FJ. Augmentation mammaplasty: a new "natural feel" prosthesis. In: Transactions of the Third International Congress of Plastic and Reconstructive Surgery. Amsterdam: Excerpta Medica; 1963. [ Links ]
17. Freeman BS. Technique of subcutaneous mastectomy with replacement; immediate and delayed. Br J Plast Surg. 1969;22(2):161-6. [ Links ]
18. Snyderman RK, Guthrie RH. Reconstruction of the female breast following radical mastectomy. Plast Reconstr Surg. 1971;47(6):565-7. [ Links ]
19. de Haan A, Toor A, Hage JJ, Veeger HE, Woerdeman LA. Function of the pectoralis major muscle after combined skin-sparing mastectomy and immediate reconstruction by subpectoral implantation of a prosthesis. Ann Plast Surg. 2007;59(6):605-10. [ Links ]
20. Spear SL, Schwartz J, Dayan JH, Clemens MW. Outcome assessment of breast distortion following submuscular breast augmentation. Aesthetic Plast Surg. 2009;33(1):44-8. [ Links ]
21. Gabriel A, Sigalove S, Sigalove NM, et al. Effect of body mass index on outcomes after prepectoral breast reconstruction. Plast Reconstr Surg. 2019;144(3):550-8. [ Links ]
22. Sigalove S, Maxwell GP, Sigalove NM, et al. Prepectoral implant-based breast reconstruction and postmastectomy radiotherapy: short-term outcomes. Plast Reconstr Surg Glob Open. 2017;5(12):e1631. [ Links ]
23. Serrano L, Mackfarlane M, Loza M, Colo F, Pefaure J. Reconstrucción mamaria inmediata prepectoral. Rev Argent Cir Plást. 2023;29(1):24-31. [ Links ]
24. Rancati AO, Angrigiani C, Hammond D, Nava M, González E, Rostagno R, et al. Preoperative digital mammography imaging in conservative mastectomy and immediate reconstruction. Gland Surg. 2016;5(1):9-14. [ Links ]
25. Rancati AO, Angrigiani CH, Hammond DC, Nava MB, González EG, Dorr JC, et al. Direct to implant reconstruction in nipple sparing mastectomy: patient selection by preoperative digital mammogram. Plast Reconstr Surg Glob Open. 2017;5(6):e1369.1. Rice CO, Strickler JH. Adeno-Mammectomy for Benign Breast Lesions. [(accessed on 8 November 2022)]. Surg Gynecol Obstet. 1951;93:759-62. Disponible online: https://europepmc.org/article/med/14893082 [ Pub Med] [Google Scholar] [ Links ]
Received: February 16, 2023; Accepted: August 08, 2023











 texto em
texto em