Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista argentina de cirugía
versão impressa ISSN 2250-639Xversão On-line ISSN 2250-639X
Rev. argent. cir. vol.115 no.4 Cap. Fed. dez. 2023 Epub 29-Nov-2023
http://dx.doi.org/10.25132/raac.v115.n4.1681
Scientific letter
Isolated pulmonary metastases from pancreatic ductal adenocarcinoma: a population with prolonged survival
1Departamento de Cirugía General Hospital Alemán de Buenos Aires. Buenos Aires. Argentina
2División de Cirugía Hepato-Pancreato-Biliar Hospital Alemán de Buenos Aires. Buenos Aires. Argentina
The incidence of isolated pulmonary metastases in pancreatic ductal adenocarcinoma is about 13%. Resection of these metastases is uncommon; however, patients presenting only with pulmonary metastases have better survival compared to those with metastases on other locations.
We report the case of a female patient who underwent lobectomy for metastases from pancreatic ductal adenocarcinoma. After resection, disease-free interval and specific diseases-free survival were 84 and 152 moths, respectively.
We consider that the next step in the treatment of this subpopulation of patients is to select those patients with favorable tumor biology who would benefit from a more aggressive approach.
Keywords: pancreatic cancer; lung metastasis; adenocarcinoma; survival; lobectomy
Pancreatic ductal adenocarcinoma is the most common pancreatic neoplasm. Nowadays, pancreatic cancer is the fourth leading cause of cancer death in the United States and its incidence is increasing. It is expected to become the second leading cause of cancer-related death by 2030. Survival at 5 years is approximately 7% and has not improved over the past decades1. Surgery remains the standard of care with curative criteria; however, most of these patients are not resectable when the diagnosis is made. About 20% of patients with pancreatic cancer are candidates for surgery; nevertheless, recurrences after resection occur in 85% of the cases2.
The course of metastatic disease depends on the organ involved. When we compare survival based on the organ affected, patients with isolated pulmonary metastases have longer survival compared to those with metastases in other locations4.
Although in this subpopulation of patients a more aggressive therapeutic approach would be justified, it is unclear whether resection of these pulmonary metastases would improve survival.
We report the case of an 82-year-old female patient who was a former smoker (2.5 pack-year), with a diagnosis of pancreatic ductal adenocarcinoma who underwent cephalic pancreaticoduodenectomy. The pathology report was suggestive of stage 1 T1N0. After surgery, the patient completed adjuvant systemic therapy with gemcitabine and radiotherapy.
Disease-free interval after pancreatic surgery was 84 months. A subsequent scan revealed an isolated pulmonary lesion in the right lobe (Fig. 1); the CA 19-9 was normal, as when the diagnosis was made. The lung function was normal.
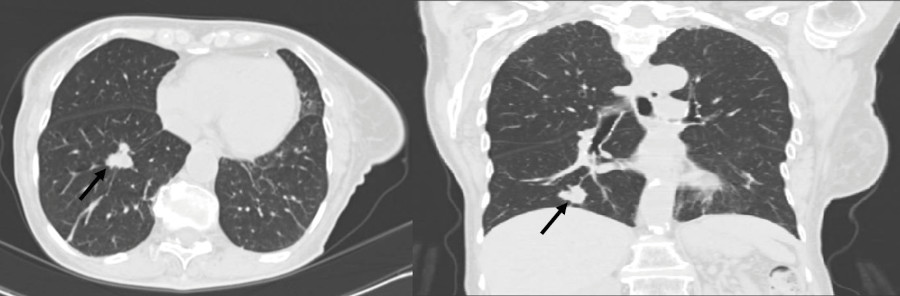
FIGURE 1 Computed tomography scan showing a 2.2 cm pulmonary nodule in the right lower lobe (black arrows).
A positron emission tomography/computed tomography (PET-CT) scan revealed a 2 cm hypermetabolic nodule in the apical segment of the right lower lobe, indicating a primary neoplasm.
Due to the patient’s history as a former smoker and the fact that her sister underwent surgery for a primary lung tumor, as well as the results of the PET-CT scan, it was determined that the lesion was also a primary lung tumor and therefore surgery was deemed necessary.
A lung lobectomy was performed. The pathology report was adenocarcinoma and the immunohistochemical tests were consistent with pancreatic cancer metastasis.
Forty-eight months later, a metastatic lesion in the left superior lobe was detected. The patient was provided with an explanation of the available therapeutic options and ultimately decided to pursue palliative treatment exclusively. Specific disease-free survival was 152 months.
We may assume that pulmonary metastases cannot exist without liver metastases, but it has been proven feasible. In a study of 130 autopsy cases, Kamisawa et al. found 16 patients with pulmonary metastases without liver metastases and postulated that this unusual pattern of spread could be due to portosystemic shunting induced by splenic vein obstruction, retrograde lymphatic infiltration from metastatic tracheobronchial lymph nodes, or aggressive characteristics of the tumors indicated by peculiar histologic features such as pleomorphic or mucoepidermoid carcinoma4. Resecting pulmonary metastases from pancreatic adenocarcinoma may seem unusual. Nevertheless, multiple studies have proven that patients with isolated pulmonary metastases have better survival. Downs-Canner et al. demonstrated that among patients who underwent surgical resection/ stereotactic radiosurgery of lung metastases, survival was significantly prolonged (67.5 months) compared to those receiving chemotherapy (33.8 months) or observation (29.9 months)5.
With these findings, the key is to select those patients with favorable tumor biology. In 96 patients with recurrence restricted to the lungs, Groot et al. identified that more than 5 pulmonary lesions and CA 19-9 >100 U/mL at time of recurrence were predictive of adverse outcome. In contrast, a recurrence-free interval of > 16 months was associated with improved outcome6.
It is unclear why patients with isolated pulmonary recurrence of pancreatic ductal adenocarcinoma have better survival rates than those with recurrence in other locations. It is also unclear whether these patients would benefit from pulmonary resection. Future studies should focus on identifying which subpopulation of patients with isolated lung metastases would benefit from a more aggressive approach.
Referencias bibliográficas /References
1. Saad AM, Turk T, Al-Husseini MJ, Abdel-Rahman O. Trends in pancreatic adenocarcinoma incidence and mortality in the United States in the last four decades; A SEER-based study. BMC Cancer. 2018;18(1):1-11. [ Links ]
2. Oettle H, Neuhaus P, Hochhaus A, Hartmann JT, Gellert K, Ridwelski K, et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: The CONKO-001 randomized trial. JAMA - J Am Med Assoc. 2013;310(14):1473-81. [ Links ]
3. Lovecek M, Skalicky P, Chudacek J, Szkorupa M, Svebisova H LR, et al. Different clinical presentations of metachronous pulmonary metastases after resection of pancreatic ductal adenocarcinoma: retrospective study and review of the literature. World J Gastroenterol. 2017;23:6420-8. [ Links ]
4. Kamisawa T, Isawa T, Koike M, Tsuruta K, Okamoto A. Hematogenous Metastases of Pancreatic Ductal Carcinoma. Pancreas. 1995;11(4):345-9. [ Links ]
5. Downs-Canner S, Zenati M, Boone BA, et al. The indolent nature of pulmonary metastases from ductal adenocarcinoma of the pancreas. J Surg Oncol. 2015;112(1):80-5. doi: 10.1002/jso.23943 [ Links ]
6. Groot VP, Blair AB, Gemenetzis G, Ding D, Burkhart RA, van Oosten AF, et al. Isolated pulmonary recurrence after resection of pancreatic cancer: the effect of patient factors and treatment modalities on survival. HPB (Oxford). 2019;21(8) :998-1008. doi: 10.1016/j.hpb.2018.12.002 [ Links ]
Received: July 25, 2022; Accepted: October 17, 2022; pub: October 10, 2023











 texto em
texto em 



