Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista argentina de cirugía
versão impressa ISSN 2250-639Xversão On-line ISSN 2250-639X
Rev. argent. cir. vol.116 no.1 Cap. Fed. mar. 2024 Epub 26-Fev-2024
http://dx.doi.org/10.25132/raac.v116.n1.1735
Scientific letter
Urgent right hepatectomy for infected hepatic necrosis secondary to endoscopic cholangiography
1Departamento de Cirugía General. Unidad de Cirugía Heptobiliopancreática y Trasplante hepático Hospital Central de las Fuerzas Armadas. Montevideo, Uruguay
Hepatic subcapsular hematoma is a rare but potentially lethal complication of endoscopic retrograde cholangiography. On the other hand, complications derived from the hematoma can be its rupture with the consequent massive bleeding, and/or portal thrombosis due to compression that evolves towards necrosis, which is susceptible to generally serious infections that require more aggressive management.
We present the case of a patient treated in our department who underwent retrograde endoscopic cholangiography as treatment for her acute cholangitis, presenting in the evolution a subcapsular hematoma that progressed to hepatic necrosis due to compression of the portal pedicle and later an infection of that necrosis. requiring an emergency right hepatectomy as surgical treatment.
Keywords: subcapsular hepático; complicación pos-CPRE; necrosis hepática infectada; hepatectomía derecha urgente
Subcapsular liver hematoma is a rare complication of endoscopic retrograde cholangiopancreatography. It can be potentially fatal and may result in rupture, massive bleeding, compression of the portal vein with thrombosis, necrosis and serious infections that require aggressive management.
A 23-year-old female patient, current smoker, was admitted for mild acute cholangitis. On admission, the abdominal ultrasound showed diffuse bile duct dilation and a gallstone of 9 mm in the distal common bile duct. The patient underwent endoscopic retrograde cholangiopancreatography (ERCP) and papillotomy, but as the gallstone could not be removed, a plastic stent was placed across the papilla.
Seventy-two hours later, the patient presented fever, abdominal pain, anemia and hypotension. The most significant findings in the laboratory tests were a 5-point drop in hemoglobin levels, raise in total bilirubin to 6 mg/dL and elevated acute phase reactants. A computed tomography (CT) scan revealed a subcapsular liver hematoma, portal vein thrombosis of the branch to segment 8 and middle hepatic vein thrombosis. The plastic stent had migrated to the colon. The surgical team decided to perform laparoscopic cholecystectomy and transcystic cholangiography. The cholangiography revealed an impacted stone in the distal common bile duct, bile duct dilation, and contrast leak in the right anterior sector of the liver. There was an ischemic area on the liver surface in segment 8 with a small bile leak. During surgery, the patient presented hemodynamic instability. To address this, a biliary drainage tube was placed in the cystic duct and an abdominal drainage tube was placed in the area of the bile leak. The operation was then concluded.
At 24 hours after surgery, the patient experienced multiple organ failure (MOF): kidney dysfunction requiring hemodialysis, hemodynamic failure requiring high doses of vasoactive agents, and pulmonary distress requiring mechanical ventilation (MV). Additionally, there were signs of liver dysfunction with a prothrombin time of 48% and hypoalbuminemia. The liver panel showed signs of liver injury/necrosis with elevated transaminases (AST 11,000 and ALT 3000).
Another CT scan was performed (Fig. 1). The right liver presented a hematoma measuring 15 cm and ischemia, as well as thrombosis of the portal vein right branch, middle hepatic vein, and right hepatic vein.

FIGURE 1 Computed tomography scan showing a hematoma measuring 15 cm (black arrow), elements of hypoperfusion of the right liver and thrombosis of the right portal vein branch (white arrow). The right and middle hepatic veins are not seen. The left hemiliver shows compensatory hypertrophy.
Empiric broad-spectrum antibiotic treatment was started with piperacillin/tazobactam plus amikacin. The hematoma was drained percutaneously, and a small amount of blood and purulent material was removed. The cultures of this material yielded negative results. The patient recovered hemodynamic stability and improved organ dysfunction, but remained was signs of sepsis.
Due to the patient’s extensive infected right liver necrosis and persistent sepsis after 6 days of medical and percutaneous treatment, the case was reviewed with the Hepatobiliary Surgery Unit. It was decided that an emergency right hepatectomy would be performed to remove the infected hepatic necrosis. During surgery, the right liver appeared ischemic, necrotic and fetid, and was enlarged due to the intrahepatic hematoma. Additionally, the left liver showed some degree of hypertrophy, which made it difficult to mobilize the organ (Fig. 2). There was an ischemic line along the axis of the middle hepatic vein. A right hepatectomy was performed via an anterior approach, with extra-Glissonian approach to the right portal pedicle and transection along the ischemic line. This was done with almost no need for usual technology (ultrasonic dissector and vessel sealer device), as the parenchyma was necrotic.
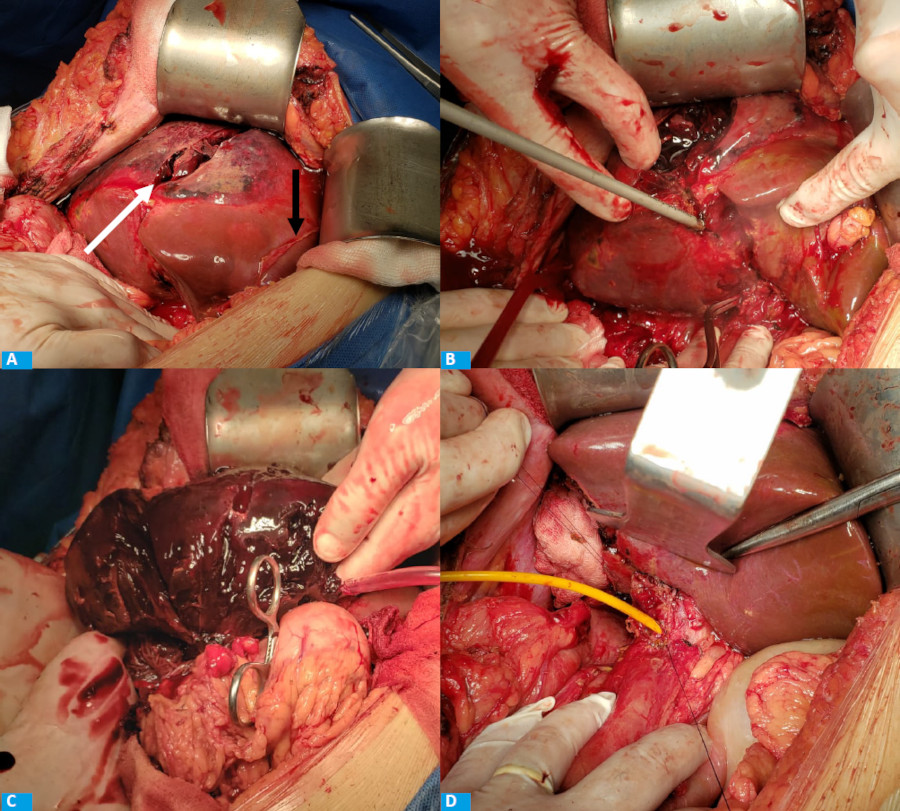
FIGURE 2 Surgery, 2A: Surgical exploration. The right liver is enlarged and has areas of ischemia/necrosis (white arrow), respecting segment 4. The black arrow corresponds to the falciform ligament. 2B. Right hepatectomy via an anterior approach, parenchymal transection. 2C. Right hepatectomy, necrotic right liver (white arrow). 2D: Final photograph, remnant liver (left liver), T-tube placed in the common bile duct
After liver resection, we attempted to clear the common bile duct stone through the transcystic route, but this was not possible because the stone was impacted in the papilla. Therefore, the stone was removed via choledochotomy, and a T-tube was inserted.
The patient stayed at the intensive care unit for 4 days after surgery and was extubated 48 hours after the procedure. She was discharged 20 days after liver resection. Two weeks later, the cholangiography showed that the bile duct was clear, and the T-tube was removed.
Hepatic necrosis is the result of hepatic hypoperfusion with or without associated hepatic arterial of portal venous occlusion. Although rare, this complication may be secondary to invasive procedures that involve manipulating the portal pedicle1.
There are case reports of subcapsular hepatic hematoma after ERCP in the published literature. Hepatic hematoma is the result of iatrogenic vascular injury caused by the tip of the guidewire perforating the intrahepatic bile duct2. Another hypothesis is that the liver injury is secondary to the traction force that the balloon exerts on the bile duct when attempting to remove a retained stone. This force could rupture vessels and bile ducts, resulting in bleeding. Intrahepatic or subcapsular hematomas can cause local mass effect on the parenchyma. This, combined with decreased perfusion due to vascular injury, can lead to greater ischemia and necrosis of the hepatic parenchyma3.
Patients with liver necrosis are at high risk of developing complications, particularly infections. Secondary infection of the necrotic parenchyma can cause liquefactive necrosis and abscesses. The mortality rate of infected hepatic necrosis is approximately 50%4.
Treatment options for infected hepatic necrosis include intravenous antibiotics, percutaneous or open surgical drainage, and liver resection. Most patients are managed with a conservative approach based on medical treatment and percutaneous drainage of collections/hematomas. When a patient’s performance status deteriorates despite previous treatment5, resection of the hepatic parenchyma should be considered because the effectiveness of a minimally invasive treatment decreases with the volume of affected parenchyma. This is the case of our patient who had infected hepatic necrosis that involved a large area of the right liver.
Referencias bibliográficas /References
1. Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR., Spirito F, Forlano R. Incidence Rates of Post-ERCP Complications: A Systematic Survey of Prospective Studies. Am JGastroenterol2007; 102(8):1781-8. doi:10.1111/j.1572-0241.2007.01279. [ Links ]
2. Ortega Deballon P, Fernández Lobato R, Garcfa Septiem J, Nieves Vizquez MA, Martínez Santos ZC, Moreno Azcoita M. Liver hematoma following endoscopic retrograde cholangiopancreatography (ERCP). Surg Endosc. 2000; 14:767-8. DOI: 10.1007/ s004640040001 [ Links ]
3. González-López R, García-Cano E, Espinosa-González O, Cruz-Salgado Á, Montiel Jarquin, Á.-J, Her-nández-Zamora V. Tratamiento quirúrgico para hematoma subcapsular hepático posterior a colangiografía retrógrada endoscópica; caso inusual. Cirugía y Cirujanos. 2015;83(6):506-9. doi:10.1016/j.circir.2015.05.028 [ Links ]
4. García Tamez A, López Cossio JA, Hernández Hernández G, González Huezo MS, Rosales Solís AA, Corona Esquivel E. Subcapsular hepatic hematoma: An unusual, but potentially life-threating postERCP complication. Case report and literature review. Endoscopia. 2016; 28(2):75-80. doi:10.1016/j.endomx.2016.04.001 [ Links ]
5. Sotelo JC, Sambresqui A, Ubeira R, Orbe G, Fernández JL, Ortiz N y cols. Hematoma hepático poscolangiopancreatografía retrógrada endoscópica. Presentación de un caso y revisión de la literatura. Acta Gastroenterol Latinoam. 2019;49(4): 367-74. [ Links ]
Received: February 05, 2023; Accepted: June 22, 2023











 texto em
texto em 



