Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Acta Odontológica Latinoamericana
versão On-line ISSN 1852-4834
Acta odontol. latinoam. vol.25 no.1 Buenos Aires abr. 2012
ARTÍCULOS ORIGINALES
Influence of different materials and techniques to transfer molding in multiple implants
Júlio C.B. Faria1, Fernando L.G. Cruz1, Laís R. Silva-Concílio2, Ana C.C. Neves2
1 Department of Restorative Dentistry, Prosthodontics Area, Dental School, Federal University of Juiz de Fora, Juiz de Fora, Minas Gerais, Brazil
2 Department of Restorative Dentistry, Prosthodontics Area, Dental School, University of Taubaté, Taubaté, São Paulo, Brazil
ABSTRACT
The aim of this study was to compare different materials and techniques used in transfer molding of multiple implants, by evaluating the space between implants and superstructure. Four external hexagon implants were fixed in a master template and the same on a superstructure. Transfer molding of implants were done using the direct and indirect techniques, with transfers united or not, using the union chemically activated acrylic resin (QA) and other groups polymerized acrylic resin (FT), and sectioned and not split. The casts were made with polyether and models divided into 8 groups (n = 5). The space between the superstructure and the master implants was measured with a microscope and the data was analyzed statistically by Student's t test (p <0.05). For the material of union there was no significant difference, except when the groups were compared with the resin Duralay QA (G4) and the resin Duolay FT (G8) and groups using resins Duolay QA (G5) and Duolay FT (G7) for the union of the transfers. When comparing the groups who had the union between the transfers and sectioned again united with those in which the union was not severed there was no statistically significant difference. QA resin was superior to the FT with respect to the union of transfers. Techniques with united transfers or not were similar.
Keywords: Dental impression technique; Dental Implants; Dental materials.
RESUMO
Influencia de diferentes materiais e técnicas de moldagem de transferência em múltiplos implantes
O objetivo deste estudo foi comparar diferentes materiais e técnicas utilizados na moldagem de transferência em implantes múltiplos, por meio da avaliação do espaço entre supra-estrutura e implantes. Quatro implantes de hexágono externo foram fixados em um modelo mestre e sobre os mesmos uma supraestrutura. Moldagens de transferência dos implantes foram feitas utilizando as técnicas indireta e direta, com transferentes unidos ou não, utilizando para a união resina acrílica quimicamente ativada (QA) e em outros grupos resina acrílica fotoativada (FT), sendo seccionadas e não seccionadas. As moldagens foram reali - zadas com poliéter e os modelos divididos em 8 grupos (n=5). O espaço existente entre a supra-estrutura mestre e os implantes foi mensurada com microscópio e os dados obtidos analisados estatisticamente pelo teste t de Student (p<0.05). Para o material de união não houve diferença significativa, exceto quando comparados os grupos com a resina Duralay QA (G4) e a resina Duolay FT (G8) e as resinas Duolay QA (G5) com a Duolay FT (G7) para união dos transferentes. Quando comparados os grupos que tiveram a união entre os transferentes seccionada e novamente unida com aqueles em que a união não foi seccionada, não foi observada diferença estatística significativa. A resina QA se mostrou superior à FT no que diz respeito à união dos transferentes. As técnicas com transferentes unidos ou não se mostraram similares.
Palavras-chave: Técnica de moldagem odontológica; Implantes dentários; Materiais dentários.
INTRODUCTION
Oral rehabilitation treatments with osseointegrated implants have a high rate of success1. Yet, several conditions may affect the predictability and the success rates of dental implants and of implant-supported prostheses. One of the main factors, among other, is the biomechanical condition2,3. The passive fit of the prosthetic supra-structure4,5 is extremely important for the success of implantsupported prostheses, thus enabling a consistent distribution of the occlusal stresses generated by them. Even though most of the components of implant-supported prostheses are pre-fabricated and, as such, they have a more accurate level of fitting than conventional prostheses, the transfer of the fitting of such components still remains a problem for the development of a work model according to the laboratory work. Such difficulties increase according to the number of implants and to their fitting6.
The techniques most widely used in transfers are the indirect technique, with a closed mold, and the direct technique, in which an open mold is used. In the indirect technique, transfers are rounded or conical and are not fixed into the mold, but may be refitted inside it before the mold is filled with the cast to obtain the model. On the other hand, the direct technique allows the normally retentive transfer to remain inside the mold, thus reducing the tilting effect of the implants and turning their refitting unnecessary. Obtaining an accurate mold is possible through the union of the mold transfers with dental floss and chemically-activated acrylic resin7. Yet, this technique requires a higher clinical timing8. An alternative for decreasing this clinical timing would be using a photopolymerizable acrylic resin9,10 Based on these possibilities and on the need for the passivity of the prostheses, the purpose of this study was to assess the accuracy obtained with three different techniques of implant transfer molds, apart from assessing how the activation of the resins used in the union impact on the level of accuracy of the technique.
MATERIALS AND METHODS
For the calculation of the samples in this study, a ttest for independent samples was used, assisted by the BioEstat 5.0 software, with a 0.9-power and a significance level equal to 0.05. Data used for this calculation was obtained from studies available in the literature, which used a methodology similar to the one applied in this work9. As a result of the ttest, it was suggested that each one of the groups be made up of three test specimens. Yet, by using a factor of safety, it was determined that five specimens be used for each group. A master model in self-polymerizable acrylic resin was made (Duralay, Reliance Dental Mfg. Co., Worth, Ill., USA). Length: 50 mm; Width: 20 mm, and Height: 15 mm. Four Neodent (Batch # 140207. Titamax, Neodent, Curitiba, Brazil), external hexagonal implants, with a 3.75mmdiameter and a 13mm-length, were loaded into the master model. For fitting the implants, a Neopronto System surgical bar, (Batch # 92327, Neodent, Curitiba, Brazil) was used as a guide and four drills were made on the model with a surgical drill - 3.0mmx15mm - (Neodent, Curitiba, Brazil), assembled on a Driller BLM 600 Plus (Driller, São Paulo, Brazil). The diameter of the drills was larger than that of the implants, thus allowing the latter to be locked onto the master model by adding condensed acrylic resin in that space. The implants were fitted and numbered from 1 to 4, clockwise (Fig. 1). The layout, parallelism and distance between the implants were supplied by means of the surgical bar.
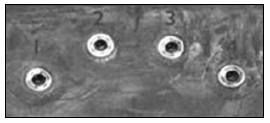
Fig. 1: Master Model with Clockwise Numbering.
A supra-structure was waxed onto UCLA-type calcinable cylinders, without anti-rotational and with Tilite strip (Neodent, Batch # 666464, Curitiba, Brazil), loaded into the implants previously fitted into the master model (Fig. 2). The supra-structure was cast with an Tilite – nickel-chrome-titanium alloy (Talladium do Brasil, Curitiba, Paraná, Brazil) by means of the lost wax casting method11 (Fig. 3). The fitting and passivity of the settling were checked by means of a probe (Exploratory Probe # 5, Duflex, SSWhite, Juiz de Fora, MG, Brazil) and of the Sheffield single-screw test12,13. After these checks, the supra-structure/master model set was analyzed by a microscope (Olympus STM, Olympus, Tokyo, Japan) to check the level of accuracy of the settling of the interface (Magnification: 30x and Accuracy: 0.001mm.
Fig. 2: Calcinable Cylinders (Front View).
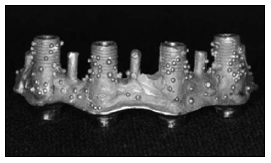
Fig. 3: Master Supra-Structure (Vestibular View).
This master model and supra-structure combination were named as Control Group, and became the standard for fitting and measuring of the specimens. For producing the individual molds that were subsequently used for the molding, the relief of the Control Group was made by means of a #7 Wax Strip (Uraby, Rio de Janeiro, Brazil). Immediately after this, the molding process was performed with Stern Tek (Stern Gold, Germany) and with the mold filled with a special Type IV cast (Troquel/ Quattro, Polidental, Brazil). The model that was thus obtained was included in a similar way to the one followed in the procedures of inclusion and acrylization of total prostheses and the individual molds of acrylic resin were pressed7. This procedure was repeated until forty individual molds were obtained, and five molds were destined to each group in the study. The molds destined to the molding technique with square transfers were drilled so as to allow for access to the screws of the transfers. Rounded transfers were used, Batch # 700399 (Neodent, Curitiba, Brazil), as well as square transfers, Batch # 679564 (Neodent, Curitiba, Brazil). For techniques using united transfers, the union was used with dental floss (Oral B, Gillette do Brasil, Brazil) and Duralay acrylic resin (Reliance Dental Mfg. Co., Worth, Ill., USA), or Duolay acrylic resin (Vipi, São Paulo, Brazil) (Fig. 4). The latter, supplied with a liquid for chemical activation and another liquid for photoactivation. When using the Duralay chemical resin, after flossing the dental floss through the four transfers, the acrylic resin was applied by means of the "brush technique" over the dental floss and around the transfers. In the sectioning techniques, a section was performed between the transfers with a diamond double-faced disk (Fava, São Paulo, SP, Brazil) and then a new union was made with the same resin. In the techniques in which Duolay chemical acrylic resin was used, the procedures followed were the same as above, for the techniques involving sectioning as well as for those without sectioning. When using the Duolay photoactivated acrylic resin, after flossing the dental floss through the transfers, the acrylic resin was applied and photopolymerized during approximately four minutes; when the technique with no sectioning was used, the application took approximately ten minutes (four minutes for pre-sectioning, two minutes for sectioning, and four additional minutes for the new union). The photopolymerization equipment used was an Optilux 401 with halogenous lamp (Demetron, Kerr Corp, Danbury, CT, USA).

Fig. 4: Square Transfers (Union with RAAQ).
In the mold made by means of closed molding, the transfers were removed from the master model and coupled to their corresponding replicas and refitted in the mold. In the open mold technique, as the transfers were removed during the molding process, only the coupling of the replicas to the transfers was performed. All the eight experimental groups were molded with polyester (Impregum, 3M ESPE, Seefelf, Germany). After the pressing of the material recommended by the manufacturer, a model with special casting Type IV was made (Troquel/Quatro, Polidental, Brazil). Once the complete crystallization of the material was obtained, the fitting of the master supra-structure onto the implants was analyzed. The assessed groups can be seen in Table 1. Before the analysis, the supra-structure was screwed (square screws, 4.1 mm Ø – Neodent, Batch # 800015664, Curitiba, Brazil), Torque: 32Ncm (Dyna Torq, ITL Dental, Irvine, CA, USA, Series # 222851), following the tightening sequence of the implants. 2, 3, 4 and 1. Measurings were made at the central point, previously marked in the master supra-structure by means of a drill (# 3203, KG Sorensen, São Paulo, Brazil), from the vestibular and lingual face with the aid of a linear microscope (Measuring Microscope STM - OLYMPUS®, Tokyo, Japan) (Fig. 5).
Table 1: Specification of Assessed Groups.
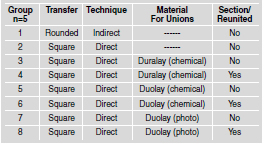

Fig. 5: View of the Specimen being Assessed by means of Linear Olympus STM Measuring Microscope.
For the statistical analysis, when means were parametric, a t-test was used for independent samples (p¡Ü0,05) and when they were not parametric, the Mann-Whitney test was used (p¡Ü0,05).
RESULTS
For the material used for unions, there was no significant difference, except when the groups using Duralay chemically activated resin (QA) (G4) and Duolay photoactivated resin (FT) (G8), were compared with the groups using Duolay QA resins (G5) and Duolay FT (G7) for unions of the transfers. When both groups were compared, the group whose union was sectioned and then reunited and the group with no sectioned union, no significant statistical difference was observed (Tables 2 and 3).
Table 2: Assessment of the Material for Unions in the Groups.
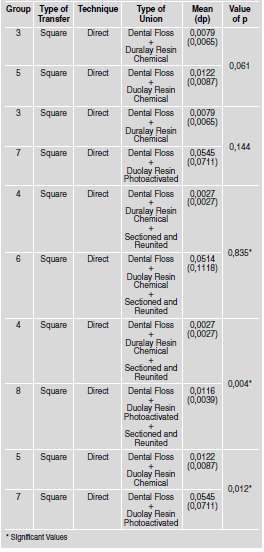
Table 3: Assessment of the Technique, With and Without Sectioning in the Groups.

DISCUSSION
The mold techniques most widely used are the "closed or indirect mold technique", that uses rounded transfers, and the "open or direct mold technique", that uses square transfers, whether united or not14-16. In general, distortions inherent with the indirect technique are related to the refitting of transfers within the molds14,17. In the direct technique, used after being recommended by Bränemark et al.7, square transfers may be united by means of an acrylic resin. Even though several authors have been doing research on the efficacy of this technique14,17,18, results have not been conclusive so far as regards their superiority in relation with the other transfer techniques. In this research, apart from the techniques with nonunited transfers, other techniques were compared, such as those that make the union of transfers with acrylic resin and those in which, after the union of transfers, the sectioning of the union takes place and transfers are united once again with a lower amount of resin so as to minimize distortions in the material19,20. The union of the transfers in the indirect technique can be made only with self-polymerizable or photo-polymerizable acrylic resin9, with self-polymerizable acrylic resin associated with dental floss, with orthodontic floss and even with the use of bars or pre-machined pins21. Self-polymerizable acrylic resins have been the most widely used materials, nevertheless, due to contraction of about 6.5% to 7.9% occurring during polymerization20,22, distortions are associated to the use of this material in the union of transfers17,23. Besides, another disadvantage derived from the use of self-polymerizable acrylic resins is the long time necessary for this technique, increasing the level of tiredness in patients and the costs of treatment due to the increase in clinical timing. Due to these factors, in this research, the union made with photopolymerizable acrylic resin was tested, and this might decrease treatment costs because of the reduction of clinical timing, and would make this treatment more comfortable for patients. Polyether is the material chosen for moldings in prostheses on implants due to its high linear stability, its low residual contraction during storage, its great rigidity and resistance to the rotation of the transfers.10,24. The measuring procedures with the microscope was used because of their scientifically proved level of accuracy (0.001mm) and efficacy5,14,17,18. In other surveys, accuracy levels were measured by means of other measuring devices, for example, softwareassisted devices10. As regards the assessment of the material used for unions, the Duolay acrylic resin chosen was chemical polymerization or by means of light, as it would decrease the time needed for union in approximately four minutes, when the technique without sectioning was used; and in ten minutes when the technique with sectioning was used (four minutes for pre-sectioning; two minutes for sectioning, and four additional minutes for the new union), vis a vis the twenty minutes used in the technique without sectioning and forty minutes, in the technique with sectioning elapsed when using the conventional Duralay resin22. This showed to be possible in different tested groups as the statistically significant difference of the adjustment was only verified when groups 4 and 8 were compared (p=0,004) and 5 and 7 (p=0,012). In both cases this may have happened due to the absence or to the excess of polymerization of Duolay resin applied with light. Insufficient or excessive time used for the application of the light and the volatilization of the liquid of the resin may bring about a greater contraction of the Duolay acrylic resin25. In the assessment of the techniques with or without sectioning no significant difference was observed between the assessed groups (Table 3). This result is consistent with studies undertaken by Herbst et al.5, Kim et al.25 and Del'Acqua et al.26. Due to the contraction of polymerization in the acrylic resins, several researchers have studied ways of minimizing the distortion present in this material20,27. According to Mojon et al.22 the reduction in the volume of the acrylic resin used in the union of the transfers would reduce the contraction of the material. Yet, this was not observed in this study, probably due to the excellence of the prosthetic components or of the material of the molding used, or to the attention given to the timing of polymerization of the resins and for that of the pouring of the molds. As this was an in vitro study, it did not have the adverse conditions typical of clinical practices such as the presence of saliva, adaptation difficulty of components of molds and/or prosthetics, angle of implants, accurate adaptation of moldings, among other. Nevertheless, there was a high level of difficulty, irrespective of the technique that was adopted, in obtaining accurate models in the molds of transfer in multiple implants.
CONCLUSION
From the results obtained, it was possible to conclude that the use of the techniques with transfers, whether united or not, did not alter the accuracy of the fitting of the supra-structure. Yet, the use of chemically activated resin for the union of transfers supplied a better fitting when compared with the photoactivated resin.
1. Suito H, Tomotake Y, Watanabe M, Nagao D, Ishida Y, Ichikawa T. Survival of immediate implant restoration: A retrospective study through 9-year-observation. J Prosthod Res 2011;55:141-145. [ Links ]
2. Miyata T, Kobayashi Y, Araki H, Ohto T, Shin K. The influence of controlled occlusal overload on peri-implant tissue. Part 4: a histologic study in monkeys. Int J Oral Maxillofac Implants 2002;17:384-390. [ Links ]
3. Esposito M, Grusovin MG, Kakisis I, Coulthard P, Worthington H.V. Interventions for replacing missing teeth: treatment of perimplantitis. Cochrane Database Syst Rev. 2008 Apr 16;(2):CD004970. [ Links ]
4. Jemt T, Lekholm U. Measurements of bone and frame-work deformations induced by misfit of implant superstructures. A pilot study in rabbits. Clin Oral Implants Res 1998;9: 272-280. [ Links ]
5. Herbst D, Nel JC, Driessen CH, Becker PJ. Evaluation of impression accuracy for osseointegrated implant supported superstructures. J Prosthet Dent 2000;83:555-561. [ Links ]
6. Vigolo P, Majzoub Z, Cordioli G. Evaluation of the accuracy of three techniques used for multiple implant abutment impressions. J Prosthet Dent 2003;89:186-192. [ Links ]
7. Bränemark PI, Zarb GA, Albrektsson T. Tissue-integrated prostheses. Chicago: Quintessence; 1985. [ Links ]
8. Barnabé W, Santos Júnior GC, Mendonça Neto T, Rubo JH. Uso simplificado de moldeiras de estoque e barras de resina acrílica nas moldagens em implantodontia. RBP Rev Bras Implantodon Prótese Sobre Implant 2005;12:105-108. [ Links ]
9. Assif D, Nissan J, Varsano I, Singer A. Accuracy of implant impression splinted techniques: effect of splinting material. Int J Oral Maxillofac Implants 1999;14:885-888. [ Links ]
10. Assunção WG, Tabata LF, Cardoso A, Rocha EP, Gomes EA. Prosthetic transfer impression accuracy evaluation for osseointegrated implants. Implant Dent 2008;17:248-256. [ Links ]
11. De La Cruz JE, Funkenbusch PD, Ercoli C, Moss ME, Graser GN, Tallents RH. Verification jig for implant-supported prostheses: A comparison of standard impressions with verification jigs made of different materials. J Prosthet Dent 2002;88:329-336. [ Links ]
12. Henry PJ, Tan AE, Uzawa S. Fit discrimination of implantsupported fixed partial dentures fabricated from implant level impressions made at stage I surgery. J Prosthet Dent 1997;77:265-270. [ Links ]
13. Kan JY, Rungcharassaeng K, Bohsali K, Goodacre CJ, Lang BR. Clinical methods for evaluating implant framework fit. J Prosthet Dent 1999;81:7-13. [ Links ]
14. Carr AB. Comparison of impression techniques for a twoimplant 15-degree divergent model. Int J Oral Maxillofac Implants 1992;7:468-475. [ Links ]
15. Assif D, Fenton A, Zarb G, Schmitt A. Comparative accuracy of implant impression procedures. Int J Periodontics Restorative Dent 1992;12:112-121. [ Links ]
16. Hsu CC, Millstein PL, Stein RS. A comparative analysis of the accuracy of implant transfer techniques. J Prosthet Dent 1993; 69:588-593. [ Links ]
17. Spector MR, Donovan TE, Nicholls JI. An evaluation of impression techniques for osseointegrated implants. J Prosthet Dent 1990;63:444-447. [ Links ]
18. Goiato MC, Domitti SS, Consani S. Influência dos materiais de moldagem e técnicas de transferência em implante, na precisão dimensional dos modelos de gesso. JBC J Bras Odontol Clín 1998;2:45-50. [ Links ]
19. Ivanhoe JR, Adrian ED, Krantz WA, Edge MJ. An impression technique for osseointegrated implants. J Prosthet Dent 1991; 66:410-411. [ Links ]
20. Dumbrigue HB, Gurun DC, Javid NS. Prefabricated acrylic resin bars for splinting implant transfer copings. J Prosthet Dent 2000;84:108-110. [ Links ]
21. Naconecy MM, Teixeira ER, Shinkai RS, Frasca LC, Cervieri A. Evaluation of the accuracy of 3 transfer techniques for implant-supported prostheses with multiple abutments. Int J Oral Maxillofac Implants 2004;19:192-198. [ Links ]
22. Mojon P, Oberholzer JP, Meyer JM, Belser UC. Polymerization shrinkage of index and pattern acrylic resins. J Prosthet Dent 1990;64:684-688. [ Links ]
23. McDonnell T, Houston F, Byrne D, Gorman C, Claffey N. The effect of time lapse on the accuracy of two acrylic resins used to assemble an implant framework for soldering. J Prosthet Dent 2004;91:538-540. [ Links ]
24. Chee W, Jivraj S. Impression techniques for implant dentistry. Br Dent J 2006;201:429-432. [ Links ]
25. Kim S, Nicholls JI, Han CH, Lee KW. Displacement of implant components from impressions to definitive casts. Int J Oral Maxillofac Implants 2006;21:747-755. [ Links ]
26. Del'Acqua MA, Arioli-Filho JN, Compagnoni MA, Mollo Jr F de A. Accuracy of impression and pouring techniques for an implant-supported prosthesis. Int J Oral Maxillofac Implants. 2008;23:226-36. [ Links ]
27. Hussaini S, Wong T. One clinical visit for a multiple implant restoration master cast fabrication. J Prosthet Dent 1997; 78:550-553. [ Links ]














