Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista argentina de cirugía
versão impressa ISSN 2250-639Xversão On-line ISSN 2250-639X
Rev. argent. cir. vol.115 no.1 Cap. Fed. maio 2023
http://dx.doi.org/10.25132/raac.v115.n1.1646
Articles
Spontaneous hepatic hemorrhage as unusual cause of acute intra-abdominal hemorrhage
1 Sector Cirugía Hepatobiliopancreática (HPB), Servicio de Cirugía General. Hospital Municipal de Agudos Dr. Leónidas Lucero de Bahía Blanca. Buenos Aires. Argentina.
There are different causes that can lead to acute intra-abdominal hemorrhage (IAH); abdominal trauma, vascular lesions as ruptured aneurysms or postoperative bleeding are the most common ones. Other gynecological causes as ectopic pregnancy or HELLP (hemolysis, elevated liver enzymes, low platelets) syndrome are also described in the literature. Spontaneous hepatic hemorrhage (SHH) is an unusual cause of acute IAH. This rare condition results from a breach in the hepatic parenchyma that occurs without an external cause. It is an acute surgical emergency as it results in intra-abdominal bleeding that, if untreated, will progress to hemorrhagic shock and death. The prognosis of SHH is favorable in patients with benign tumors (adenoma, focal nodular hyperplasia and hemangioma) and polyarteritis, with mortality rates of 0%. In patients with hepatocellular carcinoma (HCC), 40% die within 12 months of treatment, and in 20% of them mortality occurs within the first week of presentation.
A 74-year-old woman with a history of chronic obstructive pulmonary disease (COPD), hypertension, type 2 diabetes and obesity sought medical advice for dyspnea and productive cough. She was admitted to the internal medicine ward due to COPD exacerbation. During hospitalization the patient evolved with sudden pain, abdominal bloating, hypotension and tachycardia. A computed tomography (CT) scan of the abdomen (Fig. 1) showed free peritoneal fluid, a hypodense lesion covering almost the entire left liver lobe, and a 20-mm rounded and hyperdense lesion in segment III. The diagnostic paracentesis was positive for hemoperitoneum. An exploratory laparotomy was decided. On surgery, an extensive hemoperitoneum was found, with a large thrombus attached to the left liver lobe. After removing the thrombus, an indurated bleeding lesion was observed in segment III (Fig. 2A). The hepatobiliary and pancreatic surgical team performed an atypical resection to control bleeding and offer a possible single-stage curative treatment. The pathology examination reported the presence of a well-differentiated hepatocellular carcinoma (Fig. 2 B and C)).
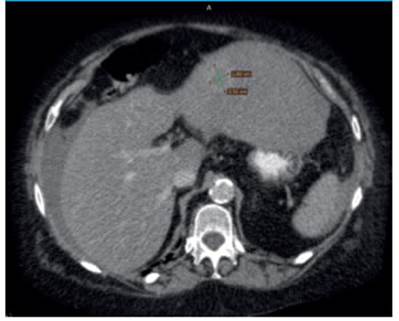
FIGURE 1 Computed tomography (CT) scan of the abdomen showing free peritoneal fluid, a 2.51 × 1.86-cm rounded, hypodense lesion with surrounding hyperdense halo in the left liver lobe (green lines).
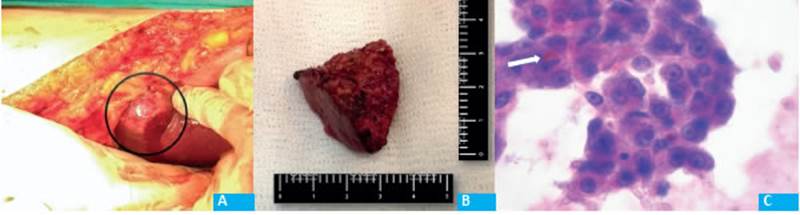
FIGURE 2 A: Indurated liver lesion with active bleeding in segment III (black circle) found during laparotomy. B: Surgical specimen of atypical liver resection of liver segment III measuring 3 × 3.5 cm. C: Microscopic image 40x. Well differentiated hepatocellular carcinoma with trabecular pattern with sinusoids and Mallory bodies (white arrow).
The patient had a favorable response to the initial treatment but died in the intensive care unit (ICU) on postoperative day 16 due to a respiratory tract complication. Hepatocellular carcinoma (HCC) accounts for 15% of all SHHs. However, only 10% of HCC present as SHH1. The most common benign causes of SHH are adenomas, hemangiomas, and focal nodular hyperplasia. Malignant causes include hepatocellular carcinoma, angiosarcoma and metastatic tumors2. Many of these patients have advanced underlying cirrhosis or fibrosis and are preferentially managed non-operatively either with conservative management (active resuscitation) or embolization. In advanced cases palliative care is preferred1. The case here described was a non-cirrhotic liver (NCL), which is even rarer since, according to the literature, 90% of HCCs develop in patients with cirrhotic liver or with chronic liver disease, which constitutes the main risk factor7.
In patients with persistent or recurrent bleeding, embolization is effective to achieve hemostasis in almost 80%, but is not feasible in up to 20% of cases due to technical issues, such as thrombosis of the main portal vein3. In the acute setting, transarterial chemoembolization (TACE), a combination of embolization with delivery of chemotherapy, has similar rates of hemostasis in patients with HCC1. Up to 20% of patients undergoing embolization will require surgical intervention to achieve hemostasis owing to persistent or recurrent bleeding4.
It should be emphasized that, according to the literature reviewed, a liver resection should not be performed in the acute setting for the sole purpose of achieving hemostasis. Patients who are candidates for local or segmental resection should be carefully selected: those patients well-compensated, with peripheral tumors and with minimal underlying liver disease are the best candidates. On the other hand, it is now known that resections in non-cirrhotic livers can be safely performed, with low perioperative morbidity and mortality and low incidence of postoperative liver failure, since the liver remnant is healthy and liver function is maintained. However, this selection is not possible in 20% of SHH because patients are hemodynamically unstable, require emergency laparotomy, and the diagnosis of the source of bleeding is made intraoperatively1. Therefore, the basic maneuvers that are usually recommended for this type of patients who require rapid management are hepatic packing associated with ipsilateral hepatic artery ligation. Both maneuvers successfully stop bleeding in twothirds of patients5. According to Zhu et al., emergency transcatheter arterial embolization (TAE) with Gelfoam instead of coils remains a good option in patients with certain hemodynamic stability, is minimally invasive and has showed good results6. On the other hand, emergency TACE is usually an option available in few high complexity centers3.
In the case reported, an atypical resection was decided due to many factors, particularly the hemodynamic stability of the patient during surgery. In addition, the lesion was small and peripheral. Finally, a team of hepatobiliary and pancreatic surgeons was available during the emergency.
Based on this presentation, a small, inexpensive, low-complexity resection may be considered in selected cases of HCC presenting as SHH, depending on the availability of resources. This would not only stop the bleeding but would offer the patient the opportunity of a possible curative treatment in a single procedure as long as it does increase the operative time. Further studies or case series are needed to confirm this consideration.
Referencias bibliográficas /References
1. Srinivasa S, Lee WG, Aldameh A, Koea JB. Spontaneous hepatic haemorrhage: a review of pathogenesis, aetiology and treatment. HPB (Oxford). [Internet]. 2015 Oct; 17(10):872-80. [ Links ]
2. Battula N, Tsapralis D, Takhar A, Coldham C, Mayer D, Isaac J, et al. Aetio-pathogenesis and the management of spontaneous liver bleeding in the West: a 16 years single-center experience. HPB (Oxford). [Internet]. 2012 Jun; 14(6):382-9. [ Links ]
3. Liu CL, Fan ST, Lo CM, Tso WK, Poon RT, Lam CM, et al. Management of spontaneous rupture of hepatocellular carcinoma: single centre experience. J Clin Oncol. 2001;19:3725-32. [ Links ]
4. Fan WZ, Zhang YQ, Yao W, Wang Y, Tan GS, Huang YH, Yang JY, Li JP. Is Emergency Transcatheter Hepatic Arterial Embolization Suitable for Spontaneously Ruptured Hepatocellular Carcinoma in Child-Pugh C.Cirrhosis? J Vasc Interv Radiol. 2018;29(3):404-12. e3. doi: 10.1016/j.jvir.2017.09.022. Epub 2017 Dec 14. [ Links ]
5. Kirikoshi H, Saito S, Yoneda M, Fujita K, Mawatari H, Uchiyama T, et al. Outcomes and factors influencing survival in cirrhotic cases with spontaneous rupture of hepatocellular carcinoma: a multicenter study. BMC Gastroenterol. 2009; 9:1-9. [ Links ]
6. Zhu LX, Wang GS, Fan ST. Spontaneous rupture of hepatocellular carcinoma. Br J Surg. 1996;83:602-7. [ Links ]
Received: September 14, 2021; Accepted: November 19, 2021











 texto em
texto em 


