Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista argentina de cirugía
versão impressa ISSN 2250-639Xversão On-line ISSN 2250-639X
Rev. argent. cir. vol.116 no.1 Cap. Fed. mar. 2024 Epub 26-Fev-2024
http://dx.doi.org/10.25132/raac.v116.n1.1740
Original article
Algorithm to select chest wall perforator flaps in immediate conservative breast surgery reconstruction
1División Cirugía Oncológica. Hospital de Clínicas José de San Martín. Universidad de Buenos Aires. Argentina.
2Programa de Cirugía Oncoplástica. Hospital de Clínicas José de San Martín. Universidad de Buenos Aires. Argentina.
Background:
Chest wall perforator flaps are a good option for immediate breast reconstruction after conservative surgery.
Objective:
The aim of this study was to describe the clinical results of an algorithm for using chest wall perforator flaps for breast reconstruction after breast-conserving surgery for breast cancer.
Material and methods:
We conducted a descriptive and retrospective study. The information was retrieved from the medical records of the patients diagnosed with breast cancer who underwent breast-conserving surgery and required reconstruction using chest wall perforator flaps between January 2020 and March 2022. The indications included volume deficit, contour defect and asymmetry. The vascular pedicle of the flap was evaluated by color Doppler ultrasound in all cases, which allowed us to follow an algorithm for selecting the best flap option.
Results:
Twenty flaps were made in 19 patients. Mean age: 52 years ± 11 (range 30-76). There were no intraoperative complications. One patient required reoperation due to a hematoma with compression of the vascular pedicle of the flap with partial flap loss, and another flap presented superficial epidermolysis. There were no cases of complete flap loss. All the patients underwent postoperative radiation therapy without loss of volume or retractions. Mean follow-up was 15 months. At 6 months, patients rated the results as excellent, good, and fair in 7, 11, and 2 cases, respectively.
Conclusion:
The selection of local perforator flaps to correct breast defects after conservative surgery, using preoperative color Doppler ultrasound to identify the vascular pedicle and a specific algorithm, allowed us to obtain satisfactory aesthetic results without the need for alloplastic elements or subsequent revisions.
Keywords: breast cancer; breast conserving surgery; segmental mastectomy; perforator flap; algorithm
Introduction
Breast reconstruction surgery restores the shape and volume to the affected tissues. The use of flaps is an important tool of its armamentarium. The description of different flaps based on chest wall artery perforators has enabled the use of donor sites with the same texture and color as the breast, while also concealing the scar in the inframammary line.
Choosing the most appropriate flap for each reconstruction is crucial to achieve optimal results. Several factors determine which perforator flap to choose and include the defect generated after tumor resection, location of the perforator that vascularizes the possible flap and its diameter, which is a reliable indicator of the perfusion capacity and therefore of the possible flap size to be achieved with this pedicle, and finally the evaluation of the donor site in terms of the final resulting scar.
The use of an algorithm to select flaps based on these factors has proven useful for their indication.
The aim of this study was to describe the clinical results of an algorithm for using chest wall perforator flaps for breast reconstruction after breast-conserving surgery for breast cancer.
Material and methods
We conducted a retrospective and descriptive study. The information was retrieved from the medical records of patients diagnosed with breast cancer who underwent oncoplastic surgery: tumor resection with immediate conservative breast surgery reconstruction using chest wall perforator flaps, between January 2020 and March 2022.
Post-resection defects were evaluated in the following locations: upper outer, lower outer, central, upper inner and lower inner quadrants.
Before surgery, the presence and thickness of the vascular pedicle was identified in all the cases using Doppler ultrasound (EDAN True Sonotrax Vascular Doppler, USA) to evaluate the vascular pedicles (cutaneous perforators) of the possible flaps to be used according to the region of the affected breast (Figures 1 and 2). The necessary flaps were then designed and made in each case, according to the algorithm described in Figure 3.

FIGURE 2 Mapping of chest wall perforators and different options for designing the different flaps, based on the origin of each perforator
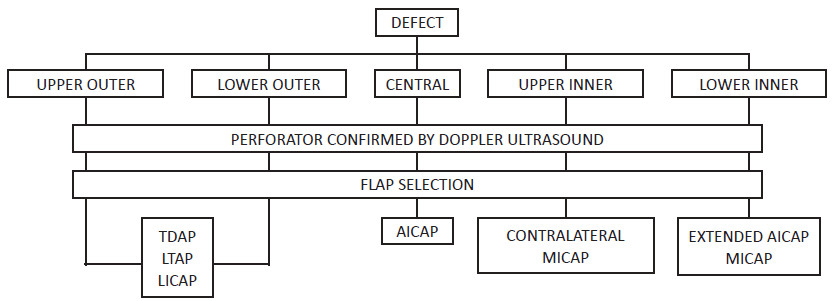
FIGURE 3. Algorithm for selecting chest wall perforator flaps according to the location of the postoperative tissue defect and the presence of perforators confirmed by color Doppler ultrasound. AICAP: Anterior Intercostal Artery Perforator. LICAP: Lateral Intercostal Artery Perforator. MICAP: Medial Intercostal Artery Perforator. LTAP: Lateral Thoracic Artery Perforator. TDAP: Thoraco Dorsal Artery Perforator
The inclusion criterion was the identification of the pedicle corresponding to the chest wall flap by preoperative Doppler ultrasound. Current smokers were excluded from the analysis.
The information recorded included demographic data, type of flaps chosen and intraoperative and postoperative results.
The aesthetic results were evaluated by the patients using a satisfaction questionnaire, which rated the results as poor, fair, good, or excellent.
The study was approved by the institutional review board.
Results
During the study period 19 patients met the inclusion criteria. Mean age was 52 ± 11 years (range, 30-76). Mean body mass index was 22.4 kg/m2 (range: 20-35). Two patients had type 2 diabetes and one had hypertension.
The histologic types were invasive carcinoma (n = 13), ductal carcinoma in situ (n = 4), Paget’s disease (n = 2) and phyllodes tumor (n = 1). One patient presented bilateral invasive carcinoma.
Sentinel-node biopsy was made via a separate axillary incision and was positive in 3 cases.
Twenty perforator flaps were used in 19 conservative surgeries: 7 AICAP (Anterior Intercostal Artery Perforator) flaps, 3 LICAP (Lateral Intercostal Artery Perforator) flaps, 4 MICAP (Medial Intercostal Artery Perforator) flaps, 4 TDAP (Thoraco Dorsal Artery Perforator) flaps and 2 LTAP (Lateral Thoracic Artery Perforator) flaps.
Of the flaps used, 19 (95%) survived well and only one (5%) presented superficial epidermolysis that did not affect flap vitality.
LICAP and TDAP flaps had the largest size.
TDAP flaps were used in 4 cases for coverage and volume replacement of upper inner and outer inner quadrants. LICAP flaps were used in 3 cases for volume reconstruction (2 cases) and coverage (1 case). AICAP flaps were used to replace volume and for coverage of the lower inner and central quadrants in 7 cases. MICAP flaps were used for lower inner and central quadrants in 4 cases (Figures 4 and 5).

FIGURE 4 Patient with a defect in the lower inner and central quadrants: flap design, transposition and immediate result with MICAP flap
The proposed algorithm for flap selection successfully identified the appropriate flap for reconstruction in all 20 patients.
There were no intraoperative complications during surgery. One patient developed a compressive hematoma that required surgical revision at 24 hours. The patients were discharge on postoperative day 1 or 2.
All the patients underwent postoperative radiation therapy without loss of volume or retractions.
Mean follow-up period was 15 months. None of the patients received aesthetic corrections on longterm follow-up and there were no local recurrences.
The patients rated the aesthetic results of the reconstructions at 6 months. Seven cases were rated as excellent, 11 cases as good, and two cases as fair.
Discussion
The results of this study indicate that the use of a Doppler-based algorithm to evaluate breast perfusion and perforator deficit was a useful tool for selecting the appropriate flap for reconstructive breast surgery.
The vascularization of the breast has been extensively and thoroughly studied and published by
many authors1,2. It is based on the main vascular pedicles (internal mammary artery, external mammary artery,
intercostal arteries and lateral thoracic artery)3,4. Many of these pedicles are usually sectioned or necessarily coagulated during the surgical procedure.
The remaining pedicles are of utmost importance not only to ensure vascular supply to the mastectomy skin flaps, but they can also be used to provide vascularization to adjacent skin flaps useful for immediate breast reconstruction5,6. The use of color Doppler ultrasound is necessary and results superior to conventional Doppler to evaluate perforators and compare their diameters which are directly related to their blood flow and therefore to the amount of tissue they can vascularize7,8.
The perforator vessels to the breast are branches of either the internal mammary artery (3rd and 4th intercostal perforators) and of other arteries as MICAP, AICAP, or LICAP9,10. These branches are used as perforator flaps for the reconstructions described in these series. The lateral intercostal artery perforator (LIAP), branch of the axillary artery, and the thoracodorsal artery perforator (TDAP) are also used as flaps for breast reconstruction.
It is important to understand the origins of the anatomy of the intercostal vessels11 which form an arcade between the aorta posteriorly and the internal mammary vessels anteriorly. The arcade is divided into vertebral, costal and muscular segments giving the dorsal, lateral, medial and anterior perforators. For descriptive purposes, the area of the chest wall beneath the inframammary fold can be equally divided into three regions7. The medial intercostal artery perforator (MICAP) is present medially and the anterior intercostal artery perforator (AICAP) is present in the central region.
The lateral intercostal artery perforator (LICAP) is present in the outer third.
Preoperative localization of the deep inferior epigastric artery perforator provides optimal surgical planning for autologous breast reconstruction with deep inferior epigastric artery perforator flaps. This information is useful to identify the location and diameter of these perforating vessels to improve the probability of reconstruction success. The use of preoperative breast vascular imaging is still an underutilized strategy despite the theoretical benefits including the identification of the intercostal breast vascularization. We highlight the versatility of local perforator flaps to correct breast defects for both immediate and delayed reconstruction.
The results of the present study should be confirmed in a larger sample before recommending the use of this algorithm as a standard tool for flap selection for breast reconstruction surgery.
In conclusion, the selection of perforator flaps can be performed using the algorithm described, based on the location of the defect. Understanding the vascular anatomy and mapping of the perforator branches can aid in dissection and preserve vascularization of the selected flap.
Referencias bibliográficas /References
1. Macmillan RD, McCulley SJ. Oncoplastic breast surgery: what, when and for whom? Curr Breast Cancer Rep. 2016;8:112-7. [ Links ]
2. Hamdi M, Van Landuyt K, de Frene B, Roche N, Blomdeel P, Monstrey S. The versatility of the intercostal artery perforator (ICAP) flap. J Plast Reocnstr Aesthet Surg. 2006;59:644-52. [ Links ]
3. Munhoz AM, Montag E, Arruda E, Brasil JA, Mendes Alrighi J, Gemperli R, et al. Immediatie conservative breast surgery reconstraction with perforator flaps: new challenges in the era of partial mastectomy reconstruction? Breast. 2011;20: 233-40. [ Links ]
4. Martellani L, Manar M, Renzi N, Papa G, Ramella V, Arnež Z. Use of licap and ltap flaps for breast reconstruction. Acta Chir Plast. 2019;60:4-8. [ Links ]
5. Wang X, He YJ, Li JF, Xie YT, Wang TF, Fan ZQ. Breast conserving surgery with immediate partial breast reconstruction using pedicled thoracodorsal artery perforator flap: a clinical analysis of 33 patients. Zhonghua Wai Kw Za Zhi. 2017; 55:120-25. [ Links ]
6. Hamdi M, Zulfikar Rasheed M. Advances in autologous breast reconstruction with pedicled perforator flaps. Clin Plat Surg. 2012;39(4):477-90. [ Links ]
7. Hamdi M, Spano, Van Landuyt K, D'Herde K, Blondeel P, Monstrey S. The lateral intercostal artery perforators: anatomical study and clinical application in breast surgery. Plat Reconstr Surg. 2008;121:389-99. [ Links ]
8. Youssif S, Hassan Y, Tohamy A, Eid S, Ashour T, Malahias M, et al. Pedicled local flaps: a reliable reconstructive tool for partial breast defects. Gand Surg. 2019;8(5):527-36. [ Links ]
9. Hakakian CS, Lockhart RA, Kulber DA, Aronowitz JA. Lateral intercostal artery perforator flap in breast reconstruction: a simplified pedicle permits an expanded role. Ann Plast Surg. 2016;76 (Suppl 3):S184-S190. [ Links ]
10. Rozen WM, Ashton MW. Radiotherapy and breast reconstruction: oncology, cosmesis and complications. Gland Surg. 2012;1(2):11927. [ Links ]
11. Gupta Roy P, Mustata L, Hu J, Phillips B, Parulekar V, Bhattacharyya M, et al. Partial breast reconstruction with lateral chest wall perforator flap to facilitate breast conservation in breast cancer: first 100 cases with cancer outcomes at 8 years follow-up and the lessons learned. Cancer Manag Res. 2021;13:9453-66 [ Links ]
Received: March 02, 2023; Accepted: August 18, 2023











 texto em
texto em 





