Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista argentina de cirugía
versão impressa ISSN 2250-639Xversão On-line ISSN 2250-639X
Rev. argent. cir. vol.116 no.1 Cap. Fed. mar. 2024 Epub 26-Fev-2024
http://dx.doi.org/10.25132/raac.v116.n1.1706
Scientific letter
ALPPS in synchronous colorectal cancer in times of COVID-19
1Hospital Escuela Gral. José F. de San Martín, Corrientes. Argentina.
2Grupo Quirúrgico HPB NEA. Argentina.
3Servicio de Oncología, Centro Médico, Corrientes. Argentina.
During the SARS-CoV-2 pandemic, we observed an increase in morbidity and mortality secondary to surgical procedures. The mortality rate for elective surgery is estimated at 19.1% and is 26% for emergency procedures. Additionally, approximately half of patients who undergo surgery while infected with SARS-CoV-2 experience postoperative pulmonary complications. Due to limitations caused by the health emergency, cancer treatments in our country have been affected in terms of hospitalization capabilities and implementation of chemotherapy treatments. We report the first ALPPS (associating liver partition with portal vein ligation for staged hepatectomy) procedure performed in northeastern Argentina on a patient with multiple colorectal metastases during the SARS-CoV-2 pandemic, with successful outcomes.
Keywords: colorectal cancer; liver metastasis; ALPPS; thrombosis; portal vein ligation; SARS-CoV-2; COVID 19
The World Health Organization (WHO) declared the outbreak of the new coronavirus disease (COVID-19) a pandemic on March 11, 2020. For this reason, almost all the healthcare resources were exclusively dedicated to the care of this incompletely described disease. The Argentine government decreed social, preventive, and mandatory isolation (SPMI) as well as social distancing. This was an appropriate temporary policy adopted in response to a disease with uncertain consequences. However, this policy had immeasurable consequences for patients with noncommunicable diseases and cancer, as they avoided hospital visits to avoid infection1,2.
Cancer patients are more prone to infections because they are immunosuppressed because of the disease and treatments, such as chemotherapy or surgery3. Therefore, patients with cancer could be at higher risk for adverse COVID-19 outcomes.
As a result, and while waiting for a more favorable moment, we have observed prolonged chemotherapy treatments, loss of follow-up, and impossibility of performing surgical interventions during the health emergency. These measures were taken to prevent or reduce transmission to the healthcare workers and to avoid higher postoperative mortality in COVID-19-positive patients.
The main limitation in the treatment of patients with malignant liver tumors is the risk of posthepatectomy liver failure. We report a case of ALPPS (associating liver partition with portal vein ligation for staged hepatectomy) procedure performed as a first experience by a team of hepatobiliary and pancreatic surgeons during the SARS-CoV-2 pandemic in a public hospital in northeastern Argentina.
A 45-year-old female patient with a performance status of 0 and body mass index (BMI) of 28 was referred to our center. She had a history of left conventional hemicolectomy plus protective ileostomy for colorectal adenocarcinoma with unresectable synchronous metastases according to the treating surgeon. The surgical procedure had been performed 2 months before the pandemic lockdown. Pathology report: colorectal adenocarcinoma; KRAS.pG12D mutation. Tumor markers: CA 19-9 > 10,000 (< 37 IU/mL); carcinoembryonic antigen (CEA) > 10,000 (< 5 ng/mL).
After 4 cycles of capecitabine, oxaliplatin, and bevacizumab, the tumor markers decreased (CA19-9: 1280 UI/ mL; CEA; 470 ng/mL). Additionally, the computed tomography (CT) scan showed that the disease was stable. The patient completed 8 cycles of chemotherapy, with favorable response (Ca 19-9: 160 UI/mL; CEA: 35 ng/mL). The magnetic resonance imaging (MRI) showed a liver with multiple pseudonodular, confluent, infiltrative lesions with central necrosis in segments IV, V, VII and VIII, heterogeneous signal intensity, restricted diffusion, and heterogeneous enhancement with gadolinium (Fig. 1). The size of liver lesions in segments V and VIII had decreased compared with the previous scan. A colonoscopy performed 8 months after the initiation of chemotherapy did not reveal any abnormalities. During the pandemic lockdown in November 2020, drug dispensing was delayed, operating room hours were restricted, and there was a shortage of medical personnel. As a result, two additional cycles of the same regimen were administered (Ca 19-9: 63 IU/mL; CEA: 26 ng/mL), followed by maintenance therapy with capecitabine plus bevacizumab. The treatment was delayed due because the patient developed respiratory symptoms and tested positive for COVID-19 on a nasopharyngeal swab. Therefore, the patient had to be isolated, and the treatment was interrupted until the symptoms resolved.
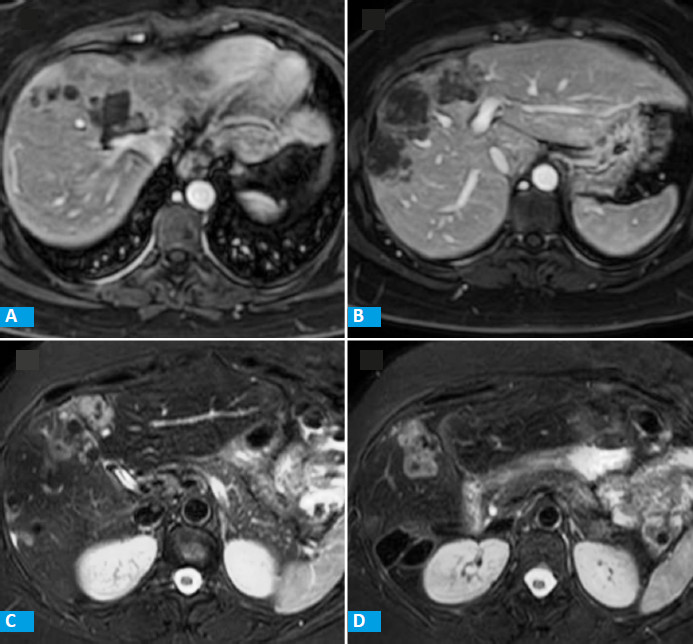
FIGURE 1 MRI of the abdomen with and without contrast agent showing multiple liver metastases. A and B: axial T1-weighted images with contrast agent. C and D: axial STIR
After receiving the 2nd dose of the vaccine, the patient was evaluated by a multidisciplinary team. As the liver volume was insufficient, ALPPS was considered the only treatment feasible. The first stage of the procedure was performed through a conventional approach via a right subcostal incision with extension to the subxiphoid region. After dissecting the hepatic ligaments, the intraoperative ultrasound did not show lesion in liver segments III, II and I. The gallbladder was resected, the liver pedicle was dissected, and the right portal vein was ligated. The line of demarcation was identified until reaching the Cantlie’s line. Parenchymal hepatic transection was performed along the right side of the falciform ligament using ultrasonic surgical aspirator until the vena cava was visualized. Blood loss of 500 mL occurred during parenchymal transection. The portally deprived liver lobe was covered with a sterile plastic bag. The patient stayed 24 hours in the intensive care unit (ICU) and was discharged on postoperative day 3. The future liver remnant was evaluated on postoperative day 10 by CT volumetry. The residual liver volume (RLV) was 350 cm3 and the preoperative volume was 210 cm3, corresponding to an increase of the RLV from 19% to 31.3% of the total liver volume (TLV). The second stage of the ALPPS procedure was carried out on postoperative day 13. The right pedicle was individualized, the right and middle hepatic veins were divided using 60-mm linear staplers with white cartridge, and trisectionectomy was completed (Fig. 2). Intraoperative blood loss was 1000 mL. During her stay in the ICU, the patient evolved with biliary leak on postoperative day 3 with drainage of 200 ml of bile per day through the drain tube placed near the transection site. On postoperative day 5, pneumonia was diagnosed. Blood cultures were positive for Klebsiella pneumoniae and the corresponding antibiotic therapy was started. The patient was discharged on postoperative day 15.
On posoperative day 27, the patient developed lower extremity edema associated with dyspnea, coughing, fever and drainage of 80 mL of bile through the abdominal drain tube. The nasopharyngeal swab test was positive for SARS-CoV-2. The CT scan indicated bilateral infiltrates consistent with COVID-19, while the Doppler ultrasound of the lower limbs revealed bilateral deep venous thrombosis despite receiving prophylactic treatment that had been initiated 48 hours postoperatively. Treatment was initiated and the patient was discharged after completing isolation. Percutaneous drainage was performed to address the residual abdominal collection. The drains were removed three months after the operation.
The pathology examination reported the presence of multiple liver metastases of welldifferentiated colorectal adenocarcinoma and clear margin.
During the first and second waves of the SARSCoV-2 pandemic, the healthcare system focused almost exclusively on managing the pandemic. This resulted in challenges for monitoring cancer patients within the provincial healthcare system. In our case, during cancer monitoring, it was difficult to perform tests due to travel restrictions, staff shortage caused by contagion, patients’ fear of visiting health facilities, and the unavailability of positron emission tomography (PET) in the province while the patient was being evaluated.
As cancer patients are almost twice as likely to be infected with SARS-CoV-2 and have more chance of more severe events compared to noncancer patients (39% versus 8%, respectively; p = 0.0003), it may be advisable to consider intentional postponing of adjuvant chemotherapy or elective surgery for stable cancer in endemic areas during a pandemic4. El-Boghdadly et al. reported that surgery performed within 7 weeks after COVID-19 infection was associated with increased morbidity and mortality. Therefore, they proposed that elective surgery should not be performed during this period unless the risk of postponing surgery outweighs it5.
Surgical resection is the only potentially curative treatment for patients with synchronous colorectal liver metastases6. Given the decrease in the number of SARS-CoV-2 cases in our environment in October 2021, surgery was decided based on the epidemiological context and the patient’s oncologic and clinical status. The rate of postoperative respiratory events was greater than expected, including reinfection and hospital readmission due to COVID-19. Although the patient was receiving deep venous thrombosis prophylaxis, we attributed the thrombotic event to the high Caprini score.
In this paper we report the case of a surgical approach using the classical ALPPS technique during the SARS-CoV-2 pandemic in a patient with synchronous metastasis of colorectal cancer who had partially responded to chemotherapy. The procedure was performed by specialists in hepatobiliary and pancreatic surgery and was the first of its kind described in northeastern Argentina.
Referencias bibliográficas /References
1. COVID Surg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396(10243):27-38. doi: 10.1016/S0140-6736(20)31182-X. [ Links ]
2. De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020; 41(22): 2083-8. [ Links ]
3. Kamboj M, Sepkowitz KA. Nosocomial infections in patients with cancer. Lancet Oncol. 2009; 10(6): 589-97. [ Links ]
4. Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020; 21(3): 335-7. [ Links ]
5. El-Boghdadly K, Cook TM, Goodacre T, Kua J, Blake L, Denmark S, et al. SARS-CoV-2 infection, COVID-19 and timing of elective surgery: A multidisciplinary consensus statement on behalf of the Association of Anaesthetists, the Centre for Peri-operative Care, the Federation of Surgical Specialty Associations, the Royal College of Anaesthetists and the Royal College of Surgeons of England. Anaesthesia. 2021; 76(7): 940-6. [ Links ]
6. Jegatheeswaran S, Mason JM, Hancock HC, Siriwardena AK. The liver-first approach to the management of colorectal cancer with synchronous hepatic metastases: a systematic review. JAMA Surg. 2013; 148(4): 385-91. [ Links ]
Received: April 10, 2022; Accepted: July 25, 2022











 texto em
texto em 




