Extracorporeal cardiopulmonary resuscitation (ECPR) is the use of extracorporeal membrane oxygenation (ECMO) in patients in whom standard cardiopulmonary resuscitation (SCPR) measures do not achieve a sustained return of spontaneous circulation after cardiac arrest (CA). 1 Patients undergoing ECMO implantation during or immediately after CA have a particularly unfavorable prognosis. 2
Despite there are no current systematic recommendations on the indication of ECMO in CA, it could be considered an emerging therapy in selected cases when SCPR fails. 3 At present, no randomized controlled trials have been reported comparing the results of ECPR versus SCPR in in-hospital CA (IHCA). 1 Though numerous cohort studies have shown that this therapy is associated with a higher survival rate until discharge, and with favorable neurological results, 4 to our knowledge, limited information has been published in our setting.
The aim of this study was to analyze and report the characteristics and clinical results of a retrospective and consecutive cohort of adult patients treated with ECPR after IHCA in a high complexity center of Argentina.
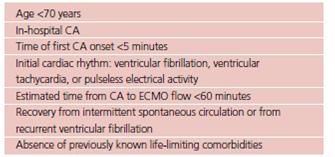
Patients over 18 years of age treated with venoarterial (VA) ECMO for IHCA between 2014 and 2022 were analyzed. The study included patients with witnessed IHCA, possibly of cardiac origin (mainly ventricular tachycardia or ventricular fibrillation as initial rhythm, extending for more than 20 minutes), 1 even with adequate CPR since its onset. Patients with CA during cardiac surgery were excluded from the study. Table 1 summarizes the inclusion criteria for ECPR at our center.
An analysis of the ventricular assistance database, which is prospectively completed, including among its main variables, demographic characteristics, information on the type of ventricular assistance, complications, relevant clinical events and clinical evolution, biochemical and echocardiographic predictors was performed. Regarding relevant clinical events, two types of survival were evaluated:
- Survival in ECMO: It assesses survival in ECMO and up to 24 hours from ventricular assistance weaning. In this case, the reasons for weaning from ECMO are cardiac function recovery or heart transplantation.
- Survival at discharge. It evaluates survival at hos pital discharge, either by release from hospital or referral to another healthcare center (e.g., third level of rehabilitation).
In addition, neurological complications, brain death (irreversible loss of consciousness and neurovegetative functions, including breathing capacity) and stroke (acute neurological focus and new ischemic or hemorrhagic changes in brain computed tomography) were analyzed.
The analysis included 8 patients, representing 11.9% of VA ECMO implanted during this period in the center. Median (interquartile range, IQR) age was 46 years (IQR 30-58) and 66% were women. Three pa tients had history of hypertension and dyslipidemia and one of diabetes. No patient presented with previ ous history of obstructive pulmonary disease, chronic kidney disease, stroke, peripheral vascular disease, atrial fibrillation, or anemia.
Three patients presented with acute coronary syndrome, two with electrical storm and the remaining causes were peripartum cardiomyopathy, myocarditis, and unidentified restrictive cardiomyopathy.
Cannulation was peripheral in 87.5% of cases (7 patients). The same number of patients required use of intra-aortic balloon pump, and 2 cases needed surgical left ventricular decompression, through pulmonary vein venting. In all the cases, ECMO was implanted as bridge to recovery.
Median circulatory assistance duration was 5 days (IQR 2-8). Successful VA ECMO weaning was achieved in 5 patients.
The rate of survival in VA ECMO was 62.5% (n=5) and at discharge 37.5% (n=3). The cause of death was non-cardiovascular in 4 of the 5 deaths.
Complications included major hemorrhage (66%), non-dialytic acute kidney failure (66%), infection (33%), seizures (11%) and thromboembolic complications (33%). No brain death was reported, and one patient suffered an ischemic stroke.
Median follow-up after discharge was 14 months (IQR 7-30). One of the 3 surviving patients is on the waiting list for elective heart transplantation, and 2 are followed-up with preserved biventricular function.
There is an increasing worldwide use of ECPR as a rescue technique in patients with refractory CA. Although controlled randomized trials are still missing demonstrating its efficacy in this setting, observational studies have reported 20% to 40% survival. 5 Currently, there is no sufficient data available to identify patients who could benefit from ECPR. It is internationally recommended to establish agreed inclusion criteria in each center to guide physicians on how to balance the intelligent use of resources among patients who are believed to have a better probability of survival after CA. 2 In our center, inclusion criteria were standardized since the creation of the multidisciplinary “ECMO team” (Table 1), considering that decision making for ECPR is often time critical and influenced by external factors such as hours and day of the week. It is therefore essential to present with adequate logistics, 24/7 trained staff for cannulation (as it is recommended that ECMO is functioning within 60 minutes after CA) and for the fast assembly and purge of the device in the emergency, and healthcare professionals who can detect within 10 minutes of CA the possible ECPR candidates.
Protocols and algorithms endeavor to quickly identify the cases with higher probability of survival with a favorable neurological outcome, as well as patients with witnessed CRA in whom high-quality CPR was quickly administered, and also cardiac arrests with a presumably reversible disorder, such as acute coronary obstructions. 2 Other factors which may influence ECPR indication are age, cause of CA, time, comorbidities and cardiac rhythm at CA onset. 3 Recently, the RESCUE-IHCA survival predictive score derived from 1075 patients was published, showing 28% survival at discharge, and identifying 6 variables associated with in-hospital mortality: age, time of day, initial rhythm, history of kidney failure, type of patient (cardiac vs. non-cardiac and clinical vs. surgical) and duration of cardiac arrest. 5 The greatest probability of success occurs in a young patient (in some working teams 50 years of age is considered the limit for ECPR), with few comorbidities, with a witnessed CA, preferably during daytime (when logistics is easier and there is more access to trained staff), with adequate CPR maneuvers performed immediately (preferably in intensive care units), and of cardiac origin, with a shockable initial rhythm.
Our results are comparable to those reported by the ELSO (Extracorporeal Life Support Organization) international multicenter registry, in which ECMO survival was 41%, and at hospital discharge 30% at an international level, 6 and to the results of the RESCUE-IHCA. 5
In our center, VA ECMO as treatment for IHCA presented an acceptable survival at hospital discharge, and it can be considered an effective treatment in highly selected patients when conventional therapies fail, being useful and applicable in a country with low and medium income and limited access to circulatory assist devices. Probably these results cannot be extrapolated to other centers of the region, as our institution is a referral VA ECMO high complexity monovalent cardiovascular center, with a developed care program, more than 7-year experience and currently, with more than 15 implants per year. Although the number of patients included in this series was low, it is still a novelty, as it would be the first experience published analyzing the results of VA ECMO in refractory IHCA in our country.