INTRODUCTION
Oral health-related quality of life (OHRQoL) was defined by Locker and Allen in 2007 as the effect of oral conditions on aspects of everyday life that are important to people. Those effects are of sufficient magnitude, whether in terms of frequency, severity or duration, to affect the individual’s perception of his/her life in general1. It is a complex, dynamic construct that includes multidimensional indicators of health and wellbeing2. OHRQoL not only measures the influence of oral conditions on a person’s physical, emotional and social wellbeing, but also evaluates the repercussions of dental treatment on his/her life3,4.
Oral conditions can affect the quality of life of children and adolescents and may have impact on their daily activities, including eating, sleep, speech, communication, and social interaction, as well as on their self-esteem5. The presence of dental caries6, malocclusion7, and dental trauma8 has been associated with a negative impact on child and adolescent quality of life. The impact of these and other oral disorders on child and adolescent quality of life has been measured by epidemiological research, which, in addition to clinical measurements, uses individuals’ self-perception of their health and of how oral conditions impact their daily lives9.
The literature contains few epidemiological studies on rural populations10,11, in particular regarding the evaluation of oral health12. It is important to assess the rural population because it has different social characteristics from the urban population. Thus, the aim of this study was to assess the impact of oral conditions on the quality of life of early adolescents, aged 11 to 14 years, in the rural area of a Brazilian municipality.
MATERIALS AND METHODS
This study was approved by the Human Research Ethics Committee of the Federal University of Minas Gerais, registered under protocol number 07939819.1.0000.5149. The adolescents who agreed to participate in the study signed a voluntary informed assent form and their parents/guardians signed a voluntary informed consent form authorizing their children to take part in the study.
Participants, eligibility criteria, study setting and period of data collection
This cross-sectional study was conducted with early adolescents aged 11 to 14 years, of both sexes, living in the rural area of Paula Cândido, Minas Gerais, Brazil. Data were collected between April and November 2019. Adolescents who had undergone or were undergoing orthodontic treatment and those with syndromes or cognitive impairment were excluded from this study.
Sample size calculation
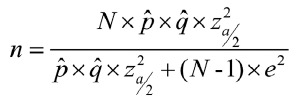
According to the Municipal Health Department, Paula Cândido has 255 adolescents aged 11 to 14 years who live in rural areas. Thus, the sample for this study was defined by calculating the sample for finite populations13:
where N is the number of individuals in the finite population, p is the sample proportion (proportion of the impact of oral conditions on quality of life), q is the complement of the proportion (1-p), z is the confidence level (95% confidence interval), and e is the margin of error.
Considering the number of early adolescents aged 11 to 14 years living in rural areas as 255, a 50% prevalence of the impact of oral conditions on their quality of life, a confidence level of 1.96 (95% confidence interval), and a margin of error of 5%, the minimum sample comprised 154 adolescents. As data would be collected in multiple settings (schools in Paula Cândido), an effect factor of 1.2 was employed to mitigate imprecision. Thus, the minimum sample size was 185 participants. To compensate for possible losses, 20% was added. Thus, the final sample was 222 adolescents from rural areas.
Data collection
OHRQoL was assessed using the short Brazilian version14 of the Child Perceptions Questionnaire (CPQ11-14), which consists of a set of questions that measure how oral conditions impact quality of life15.
The short version of the CPQ11-14 consists of 16 questions distributed across four domains: oral symptoms, functional limitations, emotional wellbeing, and social wellbeing. Each question addresses the frequency of events in the past three months and a five-point response scale is used with the following options: never = 0; once/twice = 1; sometimes = 2; often = 3; and every day/almost every day = 4. A higher score indicates more negative perception regarding the impact of oral conditions on quality of life14,15.
Oral health status was clinically evaluated by one trained examiner at public schools in Paula Candido. Calibration for dental caries, dental trauma and malocclusion was performed before data collection. A lecturer in Pediatric Dentistry coordinated the calibration of the examiner. For the three oral conditions, inter- and intra-examiner agreement were above 0.70. The examiner wore personal protective equipment (disposable gloves, mask, white coat, cap, and protective glasses) and used equipment for clinical examination such as mouth mirrors, wooden spatulas, and clinical probes. A note-taker recorded appropriate notes on a clinical record sheet.
Dental caries was evaluated according to the decayed, missing and filled teeth index (DMFT), following World Health Organization (WHO) criteria16. Participants were examined and the number of teeth with dental caries, missing teeth, and filled teeth were recorded. Malocclusion was assessed according to the Dental Aesthetic Index (DAI). This index assesses 10 occlusal characteristics according to three components: dentition (number of missing incisors, canines, and premolars), crowding and/or spacing (crowding and/or spacing in the upper arch, crowding and/or spacing in the lower arch, greater upper anterior irregularity, greater lower anterior irregularity and diastema between the upper central incisors) and occlusion (overjet, anterior crossbite, open bite and anteroposterior molar relation). The value found for each occlusal characteristic was multiplied by its specific weight and added up. To this sum, the value 13 was added to obtain the final DAI score. According to their DAI score, the adolescents could be assigned to one of four groups of malocclusion severity: normal or mild malocclusion (DAI < 25), definitive malocclusion (26 < DAI < 30), severe malocclusion (31 < DAI < 35) or very severe malocclusion (DAI > 36)17. The analysis of dental trauma was based on the Andreasen classification,18 through which only the upper and lower incisors were evaluated. The teeth were classified as: without evidence of dental trauma, teeth with mild trauma (fracture involving only enamel), teeth with severe trauma (fracture involving dentin and fracture involving dentin and pulp) and teeth with trauma that had been filled19.
Directed acyclic graph
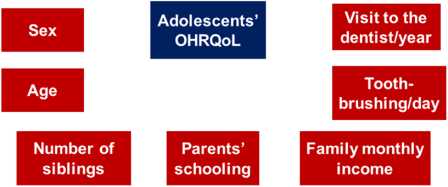
A directed acyclic graph (DAG)20 was used to identify potential confounding factors for the association between oral conditions and the OHRQoL. The confounding variables sex21 and age22, number of siblings23, parents’ schooling22, family income23, number of tooth-brushing times/day24 and visits to the dentist/year25 were incorporated into the model (Fig. 1).
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS, version 23.0, SPSS Inc., Armonk, USA). A descriptive analysis was performed. For the assessment of the association of oral conditions with the total score and the scores of the CPQ11-14 domains, regression models were used to control the influence of confounding variables. For the regression models, sex and dental trauma were analyzed as categorical variables. Age, number of siblings, parents’ schooling, family income, number of tooth-brushing times, visits to the dentist, DMFT and malocclusion were analyzed as quantitative variables. The level of statistical significance was p<0.05.
RESULTS
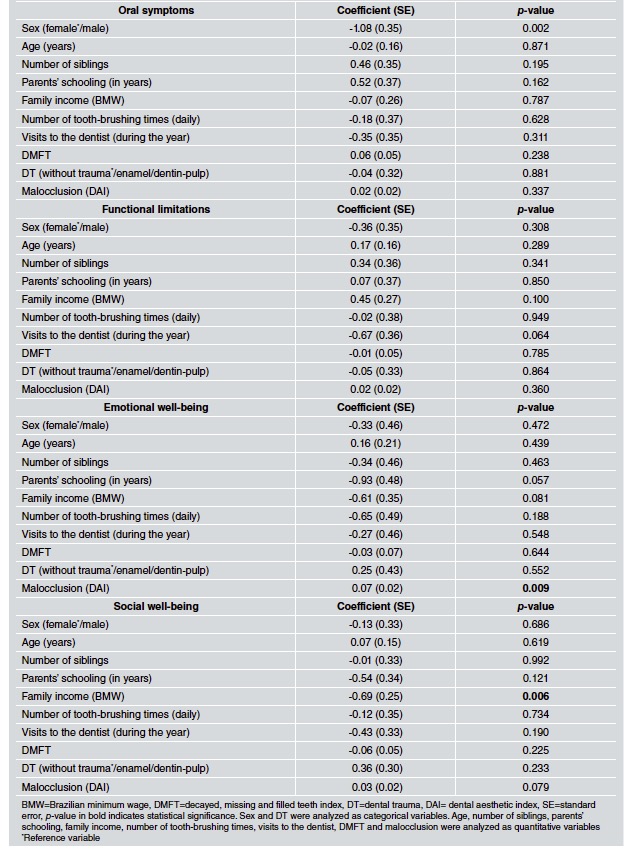
Of the 222 adolescents from rural areas, 202 were evaluated. Of these, 94 (46.5%) were male and 108 (53.5%) female. Mean age was 12.64 years (± 1.09). The regression models showed that adolescents whose families had a lower monthly income (p=0.042) and adolescents with more severe malocclusion (p=0.037) had a higher total CPQ11-14 score (Table 1). Adolescents with more severe malocclusion also scored higher in the emotional wellbeing domain (p=0.009). Finally, females scored higher than males in the oral symptoms domain (p=0.002), and adolescents from lower income families scored higher in the social wellbeing domain (p=0.006) (Table 2).
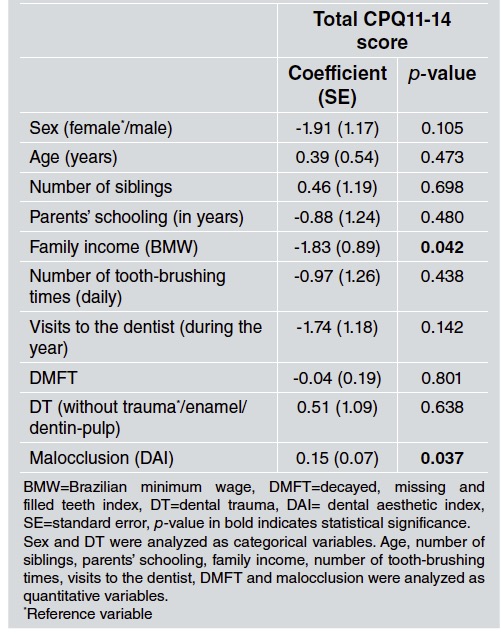
Table 1 Regression model evaluating the association of the total CPQ11-14 score with oral conditions and confounding variable
DISCUSSION
The aim of this study was to assess the impact of oral status on the OHRQoL of adolescents in rural areas. The results showed that subjects whose families had a lower monthly income and subjects with more severe malocclusion had a more negative perception of their OHRQoL. The main negative effect of malocclusion was on the emotional wellbeing domain. There is growing awareness that oral disorders can significantly impact young people’s physical, social, and psychological wellbeing. Malocclusion may have undesirable emotional and social effects26. This negative impact is likely due to the aesthetic impairment that dental and/or skeletal discrepancies can cause on the individual’s face. An altered smile or an unfavorable facial appearance can cause psychological discomfort in young people affected by malocclusion, inhibiting them from maintaining social interactions with their peers. The fear of maintaining interpersonal relationships may occur due to the adolescent’s growing apprehension of being a target of pejorative comments related to his/her dentofacial characteristics, which can produce feelings of inferiority and low selfesteem7,27.
According to the results of this study, the main negative impact of the family income variable is on the social well-being domain. Socioeconomic factors during adolescence can lead to inequalities in general and in the oral health of individuals from less privileged social strata23. The impact of socioeconomic factors such as family income on an adolescent’s social wellbeing and OHRQoL can be explained by material or psychosocial mechanisms28,29. Regarding the material issues, low family income can be one of the main barriers to access dental care services, where the individual can be advised regarding preventive measures and treated23. Psychosocial issues, on the other hand, address each individual’s experience related to social inequality, under psychological stress and lack of social protection, which can contribute to worsening his/her oral health and ultimately impair his/her OHRQoL30,31.
The results of the present study also demonstrated that female adolescents from rural areas had a more negative perception of the oral symptoms domain compared to male adolescents. Previous studies have highlighted the individual’s sex as a variable of significant influence on adolescents’ quality of life32,33. Differences related to sex can influence the way the individual responds to the presence of health issues/oral conditions or to a medical/dental treatment, which reflect on the quality of life and its domains34. In addition, several articles in the literature show that women are more concerned with health and oral health and seek more dental treatment than men, as the presence of any oral disorder has more negative repercussions on their quality of life21,35,36.
This study presents some limitations due to its crosssectional design, as it was not possible to directly determine cause-and-effect relationship between the independent variables and the OHRQoL outcome37. Another limitation is the fact that the sample is restricted to rural adolescents aged 11 to 14 years from a single Brazilian municipality. Thus, the external validity of these findings is limited and the results of this study should be used with caution when applied to rural populations with different characteristics from the population investigated herein.
In view of the results obtained, the present study may be useful for proposing and designing public health policies and services aimed specifically at populations living in rural areas. Rural populations, in general, use fewer health services38. The difficulties encountered by this population, such as lack of transportation, great distances to healthcare facilities, lack of means of communication, and low income23 can make it difficult for adolescents to access oral health services27. Thus, public policies are essential to facilitate their access to dental care services. Such services should also focus on guiding and advising their users, in addition to providing prevention measures and early treatment of certain oral disorders, such as malocclusion, to improve oral health status and provide better quality of life for adolescents living in rural areas39.