INTRODUCTION
Diffuse posterior maxillary pain and certain abnormalities can be difficult to diagnose given the close anatomic relationship between the maxillary sinus and the posterior maxillary teeth 1 . It is important to distinguish orofacial odontogenic pain/disorders from pain/disorders associated with maxillary sinusitis, to avoid unnecessary dental procedures and properly refer patients to colleagues/ dentists and vice versa.
Periapical infection is one of the most important etiologic factors responsible for sinus abnormalities of odontogenic origin 2 . The development of periapical lesions on teeth that are close to or even in contact with the maxillary sinus can cause inflammatory changes in the sinus mucosa and lead to the onset of sinusitis 3 . After the onset of pulpal necrosis, bacterial virulence factors such as enzymes and lysosomal toxins promote bacterial invasion and tissue breakdown in the periapical bone 4 . The resulting inflammation can lead to rupture of Schneiderian membrane 5 , causing dental infection and the spread of its byproducts into the maxillary sinuses. This process impairs muco-ciliary function in the maxillary sinuses and irritates the maxillary sinus mucosa 6 . As the bacteria reach the maxillary sinus and sinusitis sets in 7 , symptoms progressively worsen.
The prevalence of odontogenic maxillary sinusitis is often underestimated by medical radiologists and otolaryngologists because they are unaware of the association between apical disease and odontogenic sinusitis. Consequently, this association is rarely investigated in routine clinical practice 1 .
Studies based on cone beam computed tomography (CBCT) images have demonstrated positive association between odontogenic sinusitis and the presence of periapical or periodontal lesions. The prevalence rates of this association range from 10% to 86% of sinusitis cases 8 , 9 . Accurate diagnosis of the odontogenic origin of maxillary sinusitis by all professionals involved is crucial for effective management of this condition. It is important to note that the recommended treatment of odontogenic sinusitis differs significantly from those for other forms of maxillary sinusitis 7 . A comprehensive approach therefore needs to be used, including detailed anamnesis, complete physical examination, and imaging studies such as intraoral (periapical and occlusal) radiographs, extraoral (panoramic and Waters incidence) radiographs, and CBCT 10 .
CBCT provides a three-dimensional view of the affected anatomical structures in the axial, sagittal, and coronal planes, enabling more accurate assessment of the maxillary sinus, posterior teeth, and surrounding structures than do other imaging modalities 1 . CBCT offers high-resolution imaging in multiple planes and eliminates overlap of maxillary molars, enabling detailed examination of the patient’s maxillary sinus anatomy and detection of sinus inflammation 11 .
While other tests such as magnetic resonance imaging, ultrasound, endoscopy, and scintigraphy may also be indicated, CBCT is the most commonly used and preferred method due to its high quality and ability to provide an accurate assessment of sinus anatomy, sinus mucosa lesions, bone structures, presence of air in the sinuses, and anatomic changes of the sinuses 12 .
During the past decade, CBCT has gained popularity as avaluable technique for dentomaxillofacial images. However, multi-slice computed tomography images (MSCT) remain more familiar to radiologists and the medical profession. MSCT replaced conventional radiography as the gold standard for facial sinus examination many years ago and continues to be the preferred imaging modality in cases with suspected complicated sinusitis. This is due to the need to evaluate the soft tissues surrounding the sinuses to rule out orbital or intracranial complications, regardless of whether the examination is conducted with or without intravenous contrast material 13 . Nevertheless, there are few studies in the literature that have explored the relationship between apical lesions and paranasal sinus disease using MSCT 13 . Therefore, the aim of this study was to investigate the relationship between periapical lesions and paranasal sinus changes on multi-slice computed tomography scans, as well as the concordance between diagnoses made by an endodontist, a radiologist, an oral and maxillofacial surgeon, and an otolaryngologist.
MATERIALS AND METHOD
This retrospective observational study was approved by the local research ethics committee (number 4.601.417) and conducted in accordance with the requirements of resolution 196/96 of the National Health Council. Examination reports and images were retrieved from a private medical diagnostic radiology service and analyzed after obtaining written permission from the technical director of the service. The selected images were analyzed after careful anonymization of the patients.
Selection of images
A total 385 axial, coronal, and sagittal MSCT scans were selected using an image archiving and communication system (PACS). The examinations had been performed between 2018 and 2022. Inclusion criteria were MSCT examinations of patients aged 20 to 65 years, of either sex, with all first and second premolars, at least one of the maxillary first and second molars, and fully erupted teeth with fully developed roots. Images of edentulous patients, images with questionable tips of posterior teeth, images of patients with an orthodontic retainer, bone abnormalities, or suspected tumors around the zone of interest were excluded.
Calculation of the sample size required to determine the association between the presence of periapical lesions and sinus disease was based on previous studies 4 , 7 , 14 Sample size was estimated using the SurveyMonkey Audience program (https://pt.surveymonkey.com/mp/sample-size-calculator/; Momentive.ai, San Mateo, CA, USA), considering a 95% confidence level and a 5% margin of error, resulting in a minimum size of 385images.
Image assessment
Images were analyzed independently by four previously trained and calibrated examiners: an endodontist, a radiologist, an oral and maxillofacial surgeon, and an otolaryngologist, all of whom had extensive experience in radiology. OsiriX Lite software (Pixmeo, Bernex, Switzerland) was used to evaluate images in DICOM (Digital Imaging and Communications in Medicine) format. The variables evaluated were the presence of an apical lesion or bone thickening (no/yes), the location of the sinus change (bilateral/unilateral), contact of the lesion with the sinus floor (absent/present), discontinuity of the sinus floor (absent/present), mucosal thickening (absent/present), thickness of mucosa (1, 2, or 3 cm), opacity (absent/present), tooth involvement (both, molars, premolars, or neither), and previously performed endodontic treatment (no/yes). Data were recorded individually in a spreadsheet and the degree of agreement between investigators was assessed.
Statistical analysis
The mean age of patients with and without periapical lesion was compared using Student’s t-test. The association between the presence of an apical lesion and the other variables of interest was evaluated using the Pearson chi-square test with Bonferroni correction, the Pearson chi-square test, and Fisher’s exact test. Agreement between the diagnoses made by the endodontist and those made by the other investigators was assessed using the Kappa agreement test. Statistical analyses were performed using the software IBM SPSS (version 26.0, IBM Corporation, Armonk, NY, USA) with a significance level of 5%.
RESULTS
The mean age of patients with an apical lesion was higher than that of patients without an apical lesion (41.81 ± 10.92 versus 38.58 ± 8.74; p = 0.003). Apical lesions were observed in 36.10% of all cases of maxillary sinusitis, 73.8% of cases of unilateral maxillary sinusitis, 48.7% of cases of sinus floor discontinuity, and 67.2% of cases with previous endodontic treatment ( Fig. 1 , Table 1 ).
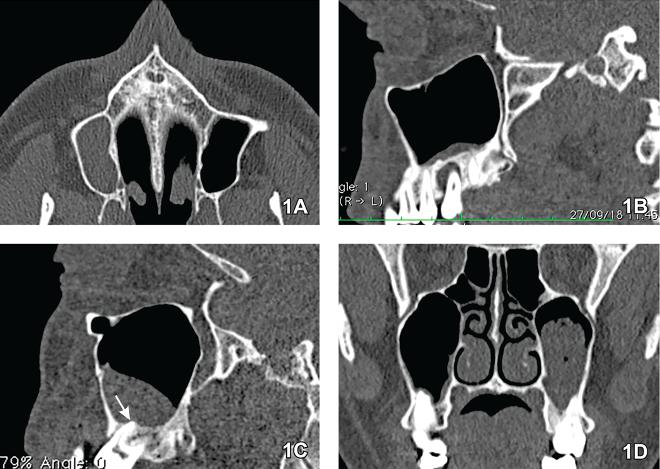
Fig. 1 Representative images of the MSCT evaluated in the study. A) Axial section. Unilateral maxillary sinusitis with total opacification of the right maxillary sinus. B) Sagittal section. Alveolar bone resorption surrounding the apices of the maxillary second molar, with involvement of the maxillary sinus. C) Sagittal section. Discontinuity of the maxillary sinus floor related to the apex of the buccal root of the maxillary molar, with resorption of the cortical bone (arrow). D) Coronal section. Intense opacification of the left maxillary sinus. Note the close contact of the maxillary molar roots with the sinus floor.
Agreement between diagnoses made by the endodontist and those made by the radiologist, oral and maxillofacial surgeon, and otolaryngologist was substantial for most study variables (k > 0.60), except for mucosal thickening, for which agreement between endodontists and the other investigators was intermediate (k = 0.397); and presence of a periapical lesion, previous endodontic treatment, and mucosal thickness, for which agreement between endodontists and radiologists was low (0 < k > 0.20; Table 2 ).
DISCUSSION
The purpose of this study was to determine the presence of apical disease and its association with sinus disease on MSCT scans. This finding of this study confirms the observations made by numerous authors 9 , 15 , 16 regarding the direct impact of periapical lesions on the maxillary sinuses. Factors such as the size of the lesion its proximity to the maxillary sinus 9 , 17 , the presence or absence of previous endodontic treatment 14 , 18 , and the anatomic relationship between the maxillary sinus and the maxillary posterior teeth7play a role in this association.
One study 17 analyzed the frequency of anatomic changes and pathologic findings in the maxillary sinuses of patients undergoing CBCT. The prevalence of maxillary sinus disease ranged from 7.5% to 66%, with mucosal thickening and opacification, or sinusitis, being the most common conditions observed. These broad findings reflect the wide variation in the scientific literature regarding the definition of maxillary sinusitis. Another study 19 defined sinusitis as any obvious thickening of the maxillary sinus mucosa. However, this definition does not distinguish between sinogenic and odontogenic causes of sinusitis, and clinical findings alone are generally insufficient to make this distinction. Therefore, imaging examination of the maxillary sinuses under various conditions is recommended for an accurate diagnosis 2 .
Different radiographic techniques are used to diagnose maxillary sinus mucosal thickening and apical periodontitis, including conventional radiography of the face sinuses, magnetic resonance imaging, CBCT, and conventional periapical radiography 9 . Among these options, CBCT provides more detailed information about changes in the maxillary sinus 20 , 21 , and high-resolution images that enable accurate assessment of the maxillary sinuses, teeth, and adjacent tissues in all planes, as well as the relationships between these structures 4 , 14 . However, in the present study, MSCT images were chosen for evaluation by different healthcare professionals because these images are considered the gold standard for assessing the soft tissues surrounding the sinuses 13 .
According to one study 21 , odontogenic infection was unilateral in approximately 70% of cases of patients treated for sinusitis, which is consistent with the findings of the present study (73.8%). Furthermore, the present study revealed that patients with an apical lesion were on average older (41.81 ± 10.92) than those without apical lesion (38.58 ± 8.74; p = 0.003), confirming the results of other studies 5 , 9 . This can be attributed to the fact that increasing age increases the likelihood of dental diseases, particularly periodontal diseases, apical abscesses, missing teeth, or other pathologic conditions, which also increases the risk of maxillary sinusitis 22 .
Table 1 Analysis of the association between the presence of apical lesión and the other variables of interest
| Variable | Apical lesion | p-value | ||
|---|---|---|---|---|
| No | Yes | |||
| Location of sinus change | Bilateral | 209 (85.7%) | 35 (14.3%) | < 0.001** |
| Unilateral | 37 (26.2%) | 104 (73.8%) | ||
| Lesion contact with the sinus floor | Absent | 40 (52.6%) | 36 (47.4%) | 0.001* |
| Present | 206 (66.6%) | 103(33.4%) | ||
| Discontinuity of the sinus floor | Absent | 125 (83.9%) | 24 (16.1%) | < 0.001* |
| Present | 121 (51.3%) | 115 (48.7%) | ||
| Mucosal thickening | Absent | 2 (50.0%) | 2 (50.0%) | 0.278* |
| Present | 244 (63.9%) | 13 (36.1%) | ||
| Thickness of the mucosa | 1 cm | 78 (67.2%) | 38 (32.8%) | 0.465** |
| 2 cm | 107 (64.5%) | 59 (35.5%) | ||
| 3 cm | 61 (59.2%) | 42 (40.8%) | ||
| Opacification | Absent | 3 (60.0%) | 2 (40.0%) | 0.081* |
| Present | 243 (63.9%) | 137 (36.1%) | ||
| Tooth involved | Both | 18 (50.0%) | 18 (50.0%) | 0.001* |
| Molar | 148 (60.7%) | 96 (39.3%) | ||
| Premolar | 80 (77.7%) | 23 (22.3%) | ||
| None | 0 (0.0%) | 2 (100.0%) | ||
| Endodontic treatment | No | 226 (69.7%) | 98 (30.3%) | < 0.001 ** |
| Yes | 20 (32.8%) | 41 (67.2%) | ||
It is estimated that dental origin accounts for 10% to 12% of all cases of maxillary sinusitis 17 . The present study demonstrated a positive correlation between apical lesion and thickening of the maxillary sinus mucosa, which is consistent with previous studies 8 , 9 . Earlier studies reported prevalence rates of sinus mucosal thickening ranging from 37% to 62% 9 , 23 , 24 . In the present study, mucosal thickening was observed in 36.1% of patients with periapical lesions, in agreement with Block and Dastoury25and Souza-Nunes 3 , who reported rates of 36.8% and 38.19%, respectively.
This discrepancy in prevalence rates can be attributed to differences in inclusion criteria and diagnostic techniques. In the present study, the thickness of the maxillary sinus mucosa was recorded at three levels, although there is still no consensus on what mucosal thickness should be considered pathological. Various authors have defined pathologic thickening as > 1 mm 31 , > 2 mm 13 or > 3 mm 23 . Mucosal thickening greater than 2 mm (grades 2 and 3), with or without a periapical lesion, was found in 269 (69.8%) of patients in the present study. Additionally, the prevalence of mucosal thickening greater than 2 mm with a periapical lesion was 26.2% of patients, which can be considered relatively low compared to the 42.1% rate found by another study 7 .
The association between mucosal thickening and periapical lesions in the maxillary posterior region is attributed to their anatomic proximity. Another study reported that odontogenic sinusitis most commonly involves the maxillary first molars, followed by maxillary second molars and maxillary first premolars 7 . Therefore, both maxillary
premolars and maxillary molars were examined in the present study. Maxillary first molars, being the first permanent teeth to erupt, are more prone to caries, pulp disease and surgical procedures. This, along with their anatomy, may explain their higher prevalence as an etiologic factor of maxillary sinusitis 15 .
The anatomical proximity between the maxillary sinus and the apices of maxillary teeth can result in inflammatory changes in the mucosa that may remain asymptomatic and persist for months or even years if the affected tooth is left untreated 2 , 5 . Another study 26 found that the risk of odontogenic sinusitis decreased by up to 2.5-fold when the location of the endodontically infected tooth moved away from the maxillary sinus (p < 0.05).
Subsequently, the affected mucosa becomes more susceptible to infection, becoming a risk factor for the development of sinusitis. Sinus inflammation may be limited to the floor of the maxillary sinus, such as in osteoperiostitis or mucositis, or may also progress and cause partial or complete obstruction of the maxillary sinus due to mucous secretions and inflammatory exudate, exhibiting clinical and radiographic features resembling those of sinogenic sinusitis 2 . The presence of vital pulp excludes the possibility of sinusitis of endodontic origin since the tooth must have necrotic pulp or an unsuccessful root canal treatment 2 .
After pulp necrosis occurs, potent bacterial virulence factors promote bacterial invasion and tissue breakdown in the periapical bone 4 , 9 . Consequently, dental infections and their byproducts may spread to the maxillary sinuses and irritate the sinus mucosa. Odontogenic sinusitis is more likely to involve anaerobic bacteria 27 , making any antibiotics used to treat normal sinusitis less effective in odontogenic cases. It is therefore crucial to diagnose the cause of sinusitis accurately before starting treatment 9 . In addition, imaging findings should be correlated with clinical information to ensure an accurate diagnosis and appropriate treatment of sinusitis 14 . Patients with periapical lesions and possibly associated mucosal thickening in the sinus floor should be referred to an endodontist for evaluation, even if they are asymptomatic 2 .
Table 2 Analysis of inter-examiner agreement regarding the diagnoses performed by the endodontist versus those performed by the radiologist, oral and maxillofacial surgeon and otorhinolaryngologist based on the assessment of MSTC
| Variable | Endodontist | Kappa | ||||
|---|---|---|---|---|---|---|
| Apical lesion | No | Yes | ||||
| Radiologist | No | 130 | 75 | 0.010 | ||
| Yes | 116 | 64 | ||||
| OMF surgeon | No | 246 | 4 | 0.977 | ||
| Yes | 0 | 135 | ||||
| OL physician | No | 246 | 4 | 0.977 | ||
| Yes | 0 | 135 | ||||
| Location of sinus change | Bilateral | None | Unilateral | |||
| Radiologist | Bilateral | 242 | 0 | 1 | 0.983 | |
| None | 0 | 0 | 0 | |||
| Unilateral | 2 | 0 | 140 | |||
| OMF surgeon | Bilateral | 244 | 0 | 0 | 0.983 | |
| None | 0 | 0 | 3 | |||
| Unilateral | 0 | 0 | 138 | |||
| OL physician | Bilateral | 244 | 0 | 0 | 0.983 | |
| None | 0 | 0 | 3 | |||
| Unilateral | 0 | 0 | 138 | |||
| Lesion contact with the sinus floor | Absent | Present | ||||
| Radiologist | Absent | 68 | 3 | 0.176 | ||
| Present | 7 | 305 | ||||
| OMF surgeon | Absent | 76 | 0 | 1.000 | ||
| Present | 0 | 309 | ||||
| OL physician | Absent | 76 | 0 | 1.000 | ||
| Present | 0 | 309 | ||||
| Discontinuity of the sinus floor | Absent | Present | ||||
| Radiologist | Absent | 149 | 235 | 0.747 | ||
| Present | 1 | 0 | ||||
| OMF surgeon | Absent | 143 | 5 | 0.940 | ||
| Present | 6 | 231 | ||||
| OL physician | Absent | 143 | 5 | 0.940 | ||
| Present | 6 | 231 | ||||
| Mucosal thickening | Absent | Present | ||||
| Radiologist | Absent | 2 | 0 | 0.397 | ||
| Present | 2 | 381 | ||||
| OMF surgeon | Absent | 2 | 0 | 0.397 | ||
| Present | 2 | 381 | ||||
| OL physician | Absent | 2 | 0 | 0.397 | ||
| Present | 2 | 381 | ||||
| Thickness of the mucosa | 1 cm | 2 cm | 3 cm | |||
| Radiologist | 1 cm | 36 | 51 | 38 | 0.024 | |
| 2 cm | 30 | 72 | 37 | |||
| 3 cm | 50 | 43 | 28 | |||
| OMF surgeon | 1 cm | 116 | 0 | 0 | 0.996 | |
| 2 cm | 0 | 165 | 0 | |||
| 3 cm | 0 | 1 | 103 | |||
| OL physician | 1 cm | 116 | 0 | 0 | 0.996 | |
| 2 cm | 0 | 165 | 0 | |||
| 3 cm | 0 | 1 | 103 | |||
| Opacification | Absent | Present | ||||
| Radiologist | Absent | 0 | 5 | 0.855 | ||
| Present | 15 | 365 | ||||
| OMF surgeon | Absent | 5 | 0 | 1.000 | ||
| Present | 15 | 365 | ||||
| OL physician | Absent | 5 | 0 | 1.000 | ||
| Present | 15 | 365 | ||||
| Tooth involved | Both | Molar | Premolar | None | ||
| Radiologist | Both | 36 | 1 | 0 | 0 | 0.990 |
| Molar | 0 | 242 | 0 | 0 | ||
| Premolar | 0 | 1 | 103 | 0 | ||
| None | 0 | 0 | 0 | 2 | ||
| OMF surgeon | Both | 36 | 0 | 0 | 0 | 1.000 |
| Molar | 0 | 244 | 0 | 0 | ||
| Premolar | 0 | 0 | 103 | 0 | ||
| None | 0 | 0 | 0 | 2 | ||
| OL physician | Both | 36 | 0 | 0 | 0 | 1.00 |
| Molar | 0 | 244 | 0 | 0 | ||
| Premolar | 0 | 0 | 103 | 0 | ||
| None | 0 | 0 | 0 | 2 | ||
| Previous endodontic treatment | No | Yes | ||||
| Radiologist | No | 273 | 51 | 0.013 | ||
| Yes | 51 | 11 | ||||
| OMF surgeon | No | 324 | 0 | 1.000 | ||
| Yes | 0 | 61 | ||||
| OL physician | No | 324 | 0 | 1.000 | ||
| Yes | 0 | 61 | ||||
All sinusitis cases investigated in the present study were reported as non-odontogenic, neglecting the possibility of endodontic involvement. This observation highlights the importance of incorporating the endodontics discipline into treatment planning for maxillary sinus disease, not only to preserve teeth and promote oral cavity health, but also to address the health of other areas, including the maxillary sinuses. Further research is needed to investigate both imaging and clinical aspects to provide more comprehensive information for dental and medical professionals.
In conclusion, this study, within its limitations, demonstrates a clear association between maxillary sinus changes and apical lesions in the maxillary premolars and molars as observed through MSCT. There was also overall agreement among the diagnoses made by the endodontist and other specialists for most sinus and tooth changes. However, there were disagreements between the endodontist and the radiologist regarding the presence of a periapical lesion, previous endodontic treatment, and mucosa thickness. These results underscore the importance of interdisciplinary collaboration among healthcare professionals to ensure precise diagnosis and effective treatment of maxillary sinusitis.















